Presentation
A 58-year-old man complained of having had pain for the past 12 hours in his left-lower quadrant, with nausea and vomiting. His pain was well localized and without radiation. He had not had a bowel movement since the onset of the pain. He had had no previous similar episodes, and had no other significant past medical or surgical history.
Upon examination, he was focally tender in the left lower quadrant, with a tender mass palpable about halfway from the umbilicus to the anterior superior iliac spine. Bowel sounds were absent; the remainder of the examination was noncontributory. His white blood cell count was elevated at 12 800 х 106/L.
A preoperative diagnosis of diverticulitis was entertained and a CT image of the abdomen requested (Fig. 1).

FIG. 1. Abdominal computed tomographic image of patient with left-lower quadrant pain and nausea.
What is the diagnosis?
Diagnosis
The CT image demonstrates a Spigelian hernia in the left lower abdomen (Fig. 2). A loop of bowel is visibly herniated through the linea semilunaris and contained within the external oblique aponeurosis. At surgery, a paramedian incision was made over the mass. An incarcerated, strangulated loop of small intestine was found herniated through a 2 cm х 2 cm defect along the linea semilunaris. Approximately 20 cm of small intestine was resected, with primary anastamosis. The defect was closed with primary suture repair. The patient's postoperative course was uneventful.
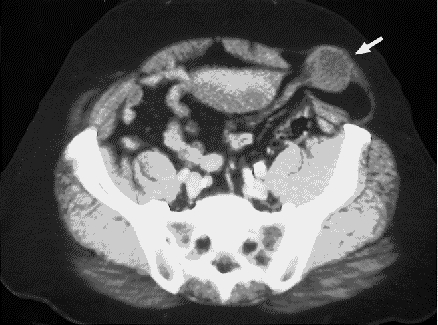
FIG. 2. Location of the Spigelian hernia.
Spigelian hernia is a rare type of ventral hernia most commonly occurring interior to the umbilicus along the linea semilunaris, the union of the aponeuroses of the external oblique, internal oblique and transversus abdominis just lateral to the rectus abdominis muscles. Spigelian hernias are interparietal hernias located between the external oblique aponeurosis and the aponeurosis of the internal oblique and transversus abdominus. They most often occur where the semicircular line crosses the linea semilunaris at the level of the arcuate line. Although pediatric Spigelian hernias have been described, patients are usually over the age of 50 years, with men and women being equally affected.1
The presentation of patients with Spigelian hernias is varied. In a report from the Mayo Clinic1 reviewing 81 cases of Spigelian hernias managed over a 21-year period (1976– 1997), the most common presentations included an intermittent mass (36%), pain (25%), pain with a mass (27%), bowel obstruction (6%), no symptoms (4%) and an incidental finding at operation (2%). A preoperative diagnosis was established in 64% of those patients. In a series of 28 cases reported by Moreno-Egea and colleagues,2 a correct preoperative diagnosis was possible in 75% of patients, whereas in another study of 19 cases from the United Kingdom2,3 the diagnosis of Spigelian hernia was suspected preoperatively in only 53% of patients. The diagnosis is often difficult, even when a mass is present on examination: the location of the hernia sac is deep to the external oblique aponeurosis, making it difficult to determine whether the mass is intra- or extra-abdominal.
As the diagnosis can be difficult to confirm clinically, diagnostic imaging methods such as ultrasound and CT have been utilitzed as preoperative adjuncts. In the study by Larson and Farley,1 19 patients were scanned preoperatively with CT, with 18 positively demonstrating the hernia. In that series only 2 patients had preoperative ultrasound scans; both were diagnostic. In a series of Spigelian hernias reported by Spangen,4 18 patients underwent preoperative ultrasound, with 17 demonstrating the hernia.
Since Spigelian hernias have a high incidence of incarceration (around 17% in the Mayo Clinic series),1 surgical repair is recommended at diagnosis. Treatments include primary aponeurotic closure and mesh repair; more recently, laparoscopic repair has also had good results.5
Submissions to Radiology for the Surgeon, soft-tissue section, should be sent to the section editor: Dr. Lawrence A. Stein, Department of Radiology, Royal Victoria Hospital, 687 Pine Ave. W, Montréal QC H3A 1A1; lawrence.stein@muhc.mcgill.ca
Competing interests: None declared.
Correspondence to: Dr. Jeff Marschall, Westview Medical, Ste. 101, 550 Carmi Ave., Penticton BC V2A 3G6; fax 250 493-9166; jeffmarschall@hotmail.com
References
- 1.Larson DW, Farley DR. Spigelian hernias: repair and outcome for 81 patients. World J Surg 2002;26:1277-81. [DOI] [PubMed]
- 2.Moreno-Egea A, Flores B, Girela E, Martin JG, Aguayo JL, Canteras M. Spigelian hernia: bilbiographical study and presentation of a series of 28 patients. Hernia 2002;6:167-70. [DOI] [PubMed]
- 3.Artioukh DY, Walker SJ. Spigelian herniae: presentation, diagnosis and treatment. J R Coll Surg Edinb 1996;41:241-3. [PubMed]
- 4.Spangen L. Spigelian hernia. Surg Clin N Am 1984;64:351-66. [DOI] [PubMed]
- 5.Moreno-Egea A, Carrasco L, Girela E, Martin JG, Aguayo JL, Canteras M. Open vs. laparoscopic repair of Spigelian hernia: a prospective randomized trial. Arch Surg 2002;137:1266-8. [DOI] [PubMed]


