Müllerian cysts are rare retroperitoneal lesions, the majority of which occur in women. Most develop in the pelvis but a few involve the upper abdomen, manifesting as a mass at the tail of the pancreas. The cysts are large and often displace adjacent organs. Precise preoperative diagnosis is seldom possible. Surgical excision is curative, but many cysts are multilocular and may recur if removal is incomplete. Histologically the lining is epithelium, ordinarily ciliated but occasionally mucinous. The cyst wall usually includes some smooth muscle.
Although uncommon, cystic lesions in the retroperitoneum are of 2 predominant types: epithelial cysts arising from large retroperitoneal organs, and cystic lesions originating from soft tissues of the retroperitoneum. Epithelial cysts arising from the pancreas and kidneys are relatively common. In rare cases such cysts may become detached from the organ, making the site of origin difficult to determine. Cystic upper-abdominal retroperitoneal lesions are difficult to diagnose; other cysts arising primarily from retroperitoneal connective tissues include lymphangiomas,1 mesothelial cysts (so-called cystic mesotheliomas),2 enterogenous cysts,3 urogenital cysts and cystic neoplasms such as teratomas or schwannomas.
The overall incidence of retroperitoneal cysts is reported as anywhere from 1 in 5750 individuals to 1 in 250 000 (average, 1 in 105 000).4 Urogenital cysts are very uncommon. Upon histologic differentiation, such cysts may be subclassified as pro-, meso- or metanephric (müllerian) in type.5 In women, müllerian cysts may occur within the pelvis (where they clinically mimic ovarian lesions) or in the upper abdomen. They also occur in the pelvis in men, where they arise in association with embryologic remnants of the regressed müllerian (paramesonephric) duct system. Typical locations include the prostatic utricle6 and the appendix testis.7
Case report
Ten years ago, a 36-year-old woman. complained of epigastric discomfort; a mass was found in her upper abdomen. Upon surgical exploration to establish a pathologic diagnosis, a large retroperitoneal cystic mass was discovered extending inferiorly from the tail of the pancreas but not arising from it. The duodenum, ligament of Treitz and left ureter were displaced. The cyst was resected, along with 3 smaller adjacent cysts.
A follow-up examination 7 years ago found recurrent cystic lesions in the retroperitoneum at the tail of the pancreas: 2 large cysts were present. Radiologically they measured 6.9 х 4.8 х 4.8 and 3.5 х 2.8 х 2.0 cm and caused displacement of the left kidney. The cysts were drained by percutaneous fine-needle aspiration; 3 subsequent aspirations were required for symptom relief.
Recently, the patient arrived again with a left upper quadrant mass and intermittent nausea and vomiting. Abdominal CT revealed a complex cystic mass in the region of the tail of the pancreas (Fig. 1). A radical excision of the cyst was planned.

FIG. 1. Computed tomographic image of the upper abdomen. A multicystic mass is present at the tail of the pancreas between the posterior wall of the stomach, the spleen and the left kidney.
Exploratory laparotomy revealed the cyst to be adherent to the pancreas along the neck, body and tail, as well as to the left kidney and transverse colon. Inferiorly, it was entwined with the aorta, left renal vein and left lateral renal artery, with displacement of the left ureter. After excision of the mass in its entirety, the patient recovered uneventfully and has remained well.
Pathologic examination of the specimen excised 10 years ago and the current specimen found them similar in appearance. Both were multilocular and about 12 cm in maximal diameter. Walls were up to 1.2 cm thick and composed of solid grayish-brown tissue (Fig. 2). The inner linings were smooth with some trabeculation and granularity but no papillae. Outer surfaces were grayish- brown with fibrous adhesions and attached fibrofatty tissue.

FIG. 2. A portion of the wall of the main cyst, with a thickened fibromuscular appearance and smaller cystic spaces. The internal lining is smooth, without papillae.
Under microscopic examination (Fig. 3), both cysts were lined with epithelium consisting of a single layer of ciliated columnar, secretory and intercalated cells (peg cells). Beneath this was a variably thick stromal layer, followed by a prominent muscular layer of interlacing bundles of smooth muscle cells. The histologic appearances of the epithelial lining and muscularis were entirely similar to normal fallopian tube.
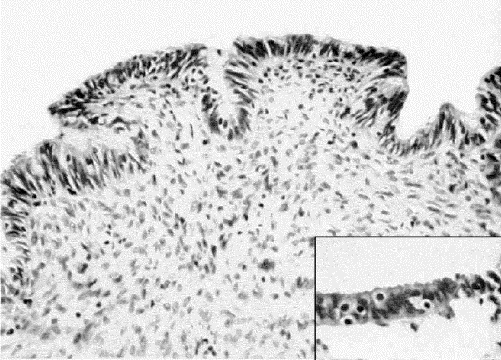
FIG. 3. Photomicrograph of the cyst wall. A single layer of ciliated epithelium (inset) containing peg cells lies above a müllerian-type stroma.
Comment
Müllerian cysts are rare lesions derived from remnants of the müllerian duct system. In men they are located in the pelvis, primarily near the prostatic utricle.6 In women most cysts of this type have also been located in the pelvic retroperitoneal tissues, where they may be confused clinically with primary ovarian and tubal cysts.8 In most reported examples in the female pelvis, the cyst lining was mucinous and similar to endocervical epithelium. Some case reports of pelvic cysts in women are confusing, because they describe retroperitoneal mucinous cystadenomas and cystadenocarcinomas as müllerian cysts. Histologic evidence that the neoplasms arose within pre-existent developmental nonneoplastic cysts is often lacking.9 The fact that these developmental cysts occur in women rather than girls has lead to speculation that growth is hormonally induced by exogenous estrogen or by endogenous hyperestrogenemia from obesity.4
Müllerian cysts of the upper abdomen are rare in women and unreported in men.4,8,10,11 There is some controversy as to their histogenesis; theories of origin include caudal growth of the developing mesonephric (wolffian) duct,10 ectopic ovarian tissue,12 a secondary müllerian system derived from invaginated celomic epithelium13 and endometriosis.
People with cysts in the upper abdomen are likely to present clinically to either a gastroenterologist or a general surgeon. A definitive preoperative diagnosis is seldom possible; even at surgery, the true nature of müllerian cysts may be difficult to determine by gross inspection. They may be multilocular, adherent to adjacent organs, or even located within the spleen.14 They may, like a lymphangioma, contain cream-coloured turbid fluid.
The lining is typically smooth and without papillary projections. A recent immunohistochemical study of lining cells15 found cytokeratins CK7, CK18, CAM 5.2 and AE1 / AE3; epithelial membrane antigen; CA125; and estrogen and progesterone receptors. Staining for CK20, CEA, calretinin and CD10 was negative.15 These results are similar to those for other müllerian-derived cystic lesions such as endometriosis and endosalpingiosis.
Multiple cysts and multilocular cysts are not uncommon, which has lead to speculation that the lesions may represent a low-grade cystadenoma. Although that suggestion can not be entirely refuted, the single-cell lining layer, lack of papillary infolding and presence in cyst walls of mature smooth muscle are more in keeping with a lesion of developmental origin. Furthermore, in contrast to müllerian cysts arising within the pelvis, malignancy in upper abdominal cysts has not been recorded.
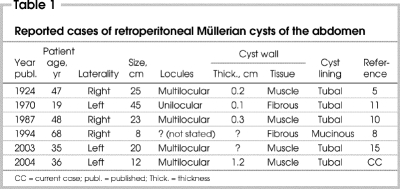
The clinical features of the 6 reported cases5,8,10,11,15 of müllerian cysts in the upper abdomen are listed in Table 1. The majority are large, thin-walled and occur in premenopausal women. As in the case we describe, some cysts have recurred, presumably because they were multilocular and originally incompletely excised. Simple but complete surgical excision with preservation of adjacent structures has always resulted in a favourable outcome.
Table 1
The major problem in the differential diagnosis of müllerian cysts at pathologic examination (including intraoperative frozen section) is with cysts arising within the pancreas. Mucinous cystic tumour (mucinous cystadenoma) of the pancreas should always be considered. These tumours typically arise in the tail of the pancreas, almost exclusively in women. They may harbour small foci of mucinous carcinoma, or may later become malignant if left in situ. Mucinous cystic tumours are usually multicystic, but unicystic or oligocystic variants exist. Their lining of mucinous epithelium may be difficult to discern or distinguish from ciliated epithelium if the biopsy taken is small or from an area where the epithelium is attenuated. The fibrous stroma of mucinous cystic tumours displays features similar to ovarian stroma; this can be very helpful in differential diagnosis. The presence of this specialized “ovarian” stroma has led to speculation that mucinous cystic tumours are also derived from ectopic ovarian tissue within the tail of the pancreas.
Competing interests: None declared.
Correspondence to: Dr. David A. Owen, Department of Pathology, 855 W 12th Ave., Vancouver BC V5Z 1M9; fax 604 875-5707; dowen@vanhosp.bc.ca
References
- 1.Nuzzo G, Lemmo G, Marrocco-Trischitta MM, Boldrini G, Giovannini I. Retroperitoneal cystic lymphangioma. J Surg Oncol 1996;61:234-7. [DOI] [PubMed]
- 2.Smith VC, Edwards RA, Jorgensen JL, Goldfarb RA, Kadmon D, Cagle P, et al. Unilocular retroperitoneal cyst of mesothelial origin presenting as a renal mass. Arch Pathol Lab Med 2000;124:766-9. [DOI] [PubMed]
- 3.Dardik H, Klibanoff E. Retroperitoneal enterogenous cyst: report of a case and mechanisms of embryogenesis. Ann Surg 1965;162:1084-6. [DOI] [PMC free article] [PubMed]
- 4.Lee J, Song SY, Park CS, Kim B. Mullerian cysts of the mesentry and retroperitoneum: a case report and literature review. Pathol Int 1998;48:902-6. [DOI] [PubMed]
- 5.Handfield-Jones RM. Retroperitoneal cysts: their pathology, diagnosis and treatment. Br J Surg 1924;12:119-34.
- 6.Coppens L, Bonnet P, Andrianne R, de Leval J. Adult mullerian duct or utricle cyst: clinical significance and therapeutic management of 65 cases. J Urol 2002;167:1740-4. [PubMed]
- 7.Johnson DB, Sarda R, Uehling DT. Mullerian-type epithelial tumor arising within a torsed appendix testis. Urology 1999;54:561. [DOI] [PubMed]
- 8.de Peralta MN, Delahoussaye PM, Tornos C, Silva E. Benign retroperitoneal cysts of Mullerian type: a clinicopathologic study of three cases and a review of the literature. Int J Gynecol Pathol 1994;13:273-8. [DOI] [PubMed]
- 9.Pennell T, Gusdonn J. Retroperitoneal mucinous cystadenoma. Am J Obstet Gynecol 1989;160:1229-31. [DOI] [PubMed]
- 10.Harpaz N, Gellman E. Urogenital mesenteric cysts with fallopian tube features. Arch Pathol Lab Med 1987;111:78-80. [PubMed]
- 11.Steinberg L, Rothman D, Drey NW. Mullerian cyst of the retroperitoneum. Am J Obstet Gynecol 1970;107:963-4. [DOI] [PubMed]
- 12.Lachman M, Berman M. The ectopic ovary: a case report and review of the literature. Arch Pathol Lab Med 1991;115:233-5. [PubMed]
- 13.Lauchlan S. The secondary mullerian system. Surg Obstet Gynecol 1972;27:133-46. [DOI] [PubMed]
- 14.Lee YS, The M. Histogenesis of true splenic cysts: a histological and immunohistochemical study. Ann Acad Med Singapore 1993;22:372-76. [PubMed]
- 15.Konishi E, Nakashima Y, Iwaski T. Immunohistochemical analysis of retroperitoneal mullerian cyst. Hum Pathol 2003;34:194-7. [DOI] [PubMed]