Abstract
Background and Purpose
The elderly population and the prevalence of stroke, dementia, and Parkinson's disease are increasing rapidly in Korea. The aim of this study was to establish the length of stay (LOS) for neurological geriatric diseases, and analyze this parameteraccording to healthcare institutions.
Methods
We used data from the Health Insurance Review and Assessment Service from 2003 to 2007. Nineteen neurological geriatric diseases were classified into four groups: dementia, cerebral hemorrhage, cerebral infarction, and Parkinson's disease. LOS was analyzed according to gender, age, insurance type, disease group, and type of healthcare institution.
Results
The LOS for neurological geriatric diseases lengthened from 5,550,193 days (10.8% of the total National Health Insurance admission days) in 2003 to 14,749,671 days (19.7%) in 2007. The mean LOS was 40.8 days in 2003, and lengthened to 71.2 days in 2007. After stratification by disease group, the mean LOS for long-term-care hospitals lengthened by 1.43 times (from 81.7 to 116.6 days) in the cerebral infarction group, 1.35 times (from 85.6 to 115.2 days) in the cerebral hemorrhage group, and 1.28 times (from 82.7 to 105.7 days) in the Parkinson's disease group.
Conclusions
The LOS for neurological geriatric diseases has lengthened markedly, which isdue to an increasesin the number of hospitalized patients and the mean LOS, which have increased most rapidly in long-term-care hospitals. These results may be useful in developing geriatric health policies.
Keywords: length of stay, geriatric disease, Korea
Introduction
Elderly people aged ≥65 years comprised 7.2% of the Korean population in 2000; this figure had increased to 10.3% in 2008. It is expected that Korea will become an aged society in 2018 and a post-aged society in 2026.1
The incidence of geriatric diseases is rising as the elderly population increases, and the incidence of stroke is thought to be 1,000-2,000 per 100,000 people aged ≥65 years. In the early 2000s, the annual incidence of stroke was reported to be approximately 100,000, and the prevalence was thought to be approximately 400,000.2 Based on a review of medical records, the prevalence of Parkinson's disease was reported to be 27.83 per 100,000 people of all age groups in the early 2000s, and 165.9 per 100,000 people aged ≥60 years.3 The prevalence of dementia was reported to be approximately 8.5% of elderly people (aged ≥65 years) in 2005, corresponding to a total of 360,000 people.4 The number of patients who were hospitalized or received outpatient treatment for 19 geriatric diseases that were covered by the Long-term Care Insurance Law for the Elderly5 increased 1.9-fold from 2002 (n=499,000) to 2008 (n=952,000),6 during which their associated medical expenses increased 3.8-fold, from KRW 581.3 billion to KRW 2,198.3 billion. The proportion of cost related to geriatric diseases in the National Health Insurance (NHI) schemeincreased during this time from 4.25% to 8.33%.
Quantitative aspects of medical resources, such as length of stay (LOS), should be consideredalong with the incidence and prevalence of diseases and associated medical expenses. LOS is an index of the quantity of medical services whose perspective differs from that of medical expenses. That is, the same LOS can result in differences in medical expenses according to disease severity, and the LOS can differ for the same medical expenses, depending on the type of disease. With the recent increase in the number of long-term-care hospitals, it is expected that LOS will lengthen due to a higher prevalence of geriatric diseases. Studies have examined the factors that affect LOS,7 the effects of LOS on healthcare administration,8 and LOS associated with specific diseases9,10 or specific patient classes11 in Korea.
Using the health insurance claim data that were collected during 2003-2007, we calculated the LOS for neurologicalgeriatric diseases in patients aged ≥40 years, and compared the LOS among healthcare institutions.
Methods
Study data
We selected 19 neurological geriatric diseases and related variables, based on the primary disease code among the health insurance claim data for which a review and an assessment were completed by the Health Insurance Review and Assessment Service (HIRA) during the 5-year period from 2003 to 2007. In Korea, the NHI is a social insurance scheme; all Koreans join an insurance scheme as a form of health insurance or public medical aid. All healthcare institutions have been appointed as medical insurance hospitals. After providing treatment for diseases that are covered by the NHI scheme, a hospital will submit an insurance claim to HIRA. Then, following a review and assessment of this claim, HIRA makes a payment to the healthcare institution.
Measures and variables
LOS is the total sum of days of hospital stay per year. LOS was compared based on variables such as gender, age, insurance type, disease group, and type of healthcare institution. Considering the characteristics of geriatric diseases, the study population was divided into two age groups: 40-64 years and ≥65 years. The types of insurance were classified into health insurance, public medical aid, and others. Using the International Classification of Diseases codes, 19 neurological geriatric diseases were classified into four groups: cerebral infarction, cerebral hemorrhage, Parkinson's disease, and dementia. The following codes (for neurological geriatric diseases) were assigned to the cerebral infarction group: I63 (cerebral infarction), I64 (stroke, not specified as hemorrhage or infarction), I65 (occlusion and stenosis of precerebral arteries, not resulting in cerebral infarction), I66 (occlusion and stenosis of cerebral arteries, not resulting in cerebral infarction), I67 (other cerebrovascular disease), I68 (cerebrovascular disorders in diseases classified elsewhere), and I69 (sequelae of cerebrovascular disease). The following were classified into the cerebral hemorrhage group: I60 (subarachnoid hemorrhage), I61 (intracerebral hemorrhage), and I62 (other nontraumatic intracranial hemorrhage). The dementia group comprised F00 (dementia in Alzheimer's disease), F01 (vascular dementia), F02 (dementia in other disease classified elsewhere), F03 (unspecified dementia), and G30 (Alzheimer's disease), and the Parkinson's disease group comprised G20 (Parkinson's disease), G21 (secondary Parkinsonism), G22 (Parkinsonism in diseases classified elsewhere), and G23 (other degenerative diseases of the basal ganglia).
Healthcare institutions were classified into six groups: tertiary hospitals, general hospitals, hospitals, long-term-care hospitals, private clinics, and public health centers.
Data analysis
Statistical analyses were performed using SAS software (version 9.1). The mean, standard deviation, median, 25th percentile (Q1), and 75th percentile (Q3) were calculated. The parameters associated with LOS were compared using the t-test and ANOVA, with the level of statistical significance set at p<0.05.
Poisson regression with a generalized estimating equation- and a log link was used to assess the relationship between predictors and LOS. This method accounts for the potential correlation of repeated admissions for the same patient; we assumed that the correlation from multiple admissions was exchangeable. Standard errors were adjusted for patient clustering with the robust sandwich estimator.
Results
Comparison of LOS according to NHI and geriatric disease
In patients aged ≥40 years, LOS due to neurological geriatric diseases was found to total 5,550,193 days in 2003, which accounted for 10.8% of LOS in the total NHI admission days. In 2007 it was found to be 14,749,671 days, accounting for 19.7% of LOS in the total NHI admission days.
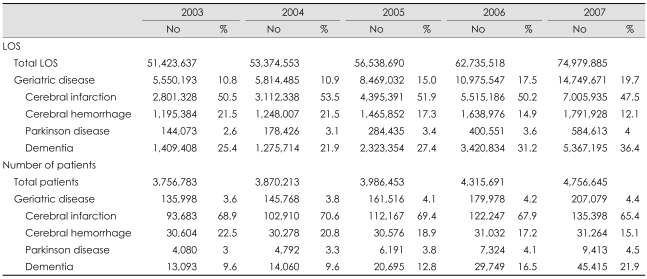
In 2003 and 2007, LOS was longest in the cerebral infarction group. This was followed by the dementia, cerebral hemorrhage, and Parkinson's disease groups. For geriatric diseases, LOS was prolonged from 25.4% in 2003 to 36.4% in 2007 in the dementia group, and from 2.6% in 2003 to 4.0% in 2007 in the Parkinson's disease group. However, in the cerebral infarction and cerebral hemorrhage groups LOS was shortened from 50.5% and 21.5% to 47.5% and 12.1%, respectively (Table 1).
Table 1.
Comparison of LOS and numbers of patient according to National health insurance and geriatric disease from 2003 to 2007
LOS: length of stay.
LOS for neurological geriatric diseases
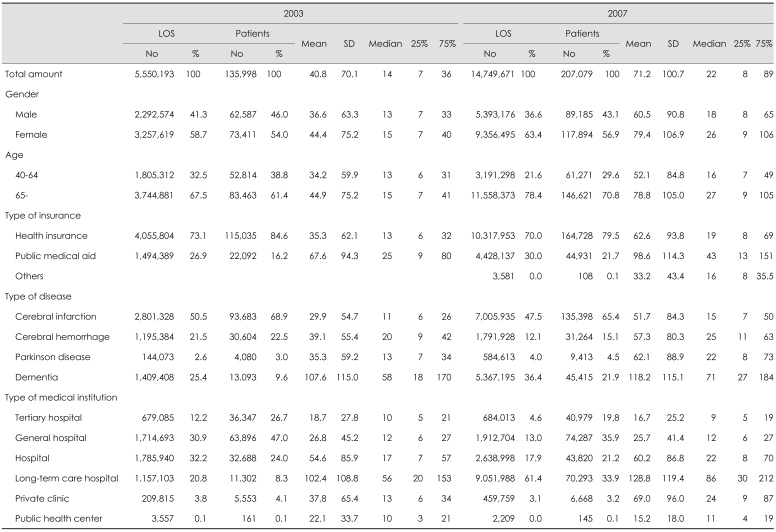
The parameters associated with LOS are compared in Table 2. In 2003, the mean LOS due to geriatric diseases was 40.8 days (median: 14 days). In 2007, it was 71.2 days (median: 22 days). That is, the mean and median LOSs had lengthened by 1.75 and 1.57 times, respectively (p<0.01).
Table 2.
Comparison of LOS and numbers of patient according to the related-parameters in 2003 and 2007
LOS: length of stay.
In 2007, the mean LOS for female patients was 79.4 days (median: 26 days). This was significantly longer than the 60.5 days (median: 18 days) for male patients (p<0.01). In both groups, the mean and median LOSs were longer in 2007 than in 2003. In 2007, the mean LOS in patients aged ≥65 years was 78.8 days (median: 27 days). This was significantly longer than the 52.1 days (median: 16 days) for patients aged 40-64 years (p<0.01). In both groups, the mean and median LOSs were longer in 2007 than in 2003.
In 2007, the mean LOS in the dementia group was 118.2 days (median: 71 days), and this was the longest among the groups. This was followed by the Parkinson's disease group (mean: 62.1 days; median: 22 days), cerebral hemorrhage group (mean: 57.3 days; median: 25 days), and cerebral infarction group (mean: 51.7 days; median: 15 days). In 2003, the mean LOS was longest in the dementia group, followed in order by the cerebral hemorrhage, Parkinson's disease, and cerebral infarction groups. The mean and median LOSs in these four groups were longer in 2007 than in 2003.
In 2007, the mean LOS in long-term-care hospitals was 128 days (median: 86 days), and this was the longest among the groups. This was followed in order by private clinics (mean: 69 days; median: 24 days), tertiary hospitals (mean: 16.7 days; median: 9 days), and general hospitals (mean: 25.7 days; median: 12 days). Compared with 2003, the mean LOS was longer in the long-term-care hospitals and private clinics, but shorter in the tertiary hospitals, general hospitals, hospitals, and public healthcare centers.
LOS in healthcare institutions stratified by geriatric disease subgroup
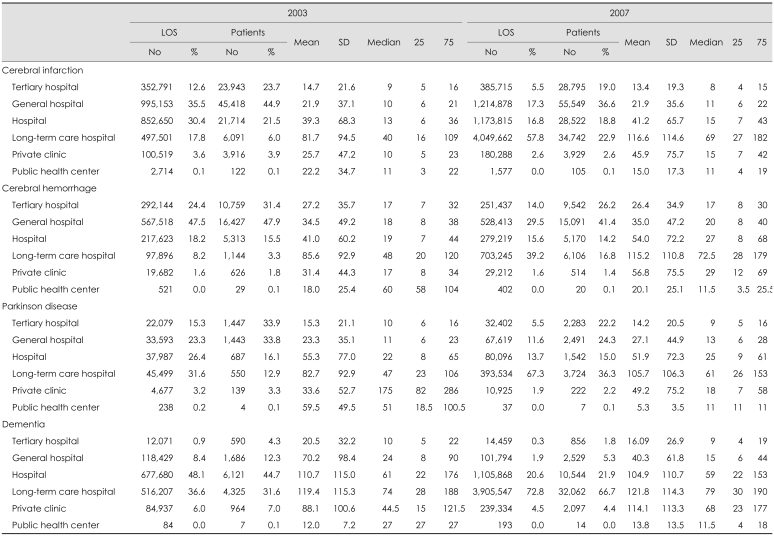
The LOS in each type of healthcare institution after stratification by disease group is given in Table 3. In 2003, the primary healthcare institutions for the treatment of the four disease groups included the tertiary hospitals, general hospitals, and hospitals, which accounted for 57-80% of the total LOS. However, in 2007 that proportion decreased to 30-60%, and that forlong-term-care hospitals was 39.2-72.8%.
Table 3.
Comparison of LOS and numbers of patient according to healthcare institutions, stratified by geriatric disease subgroup in 2003 and 2007
LOS: length of stay.
Compared with 2003, the mean LOS in each type of healthcare institution was similar or slightly longer in the tertiary hospitals, general hospitals, and hospitals in the cerebral infarction, cerebral hemorrhage, and Parkinson's disease groups in 2007. However, in the long-term-care hospitals the mean LOS was longer, by 1.43 times (81.7-116.6 days), 1.35 times (85.6-115.2 days), and 1.28 times (82.7-105.7 days), respectively. In private clinics, it was longer by 1.79 times (25.7-45.9 days), 1.81 times (31.4-56.8 days), and 1.46 times (33.6-49.2 days), respectively. In the dementia group, the mean LOS was 1.30-fold longer (88.1-114.1 days) only in the private clinics.
Application of a poisson regression model to LOS
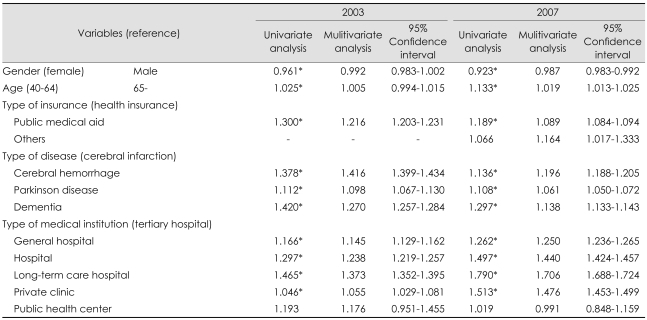
The results of univariate and multivariate Poisson regression analysis presented as the relative risk (RR) are given in Table 4. The RR of males (compared with females) in 2007 was 0.987 and was significantly lower than 1 (0.992) in 2003; an RR of 65 and more (compared with 40-64) in 2007 was 1.019, and was significantly higher than 1 (1.005) in 2003.
Table 4.
Application of a poisson regression model on LOS in 2003 and 2007
*p<0.001.
LOS: length of stay.
The RRs of public medical aid (compared with health insurance), cerebral hemorrhage, Parkinson's disease, and dementia (compared with cerebral infarction) in 2007 were 1.089, 1.196, 1.061, and 1.138, respectively, which were lower than those recorded for 2003. However, the RRs of general hospitals, hospitals, long-term-care hospitals, and private clinics (compared with tertiary hospitals) in 2007 were 1.250, 1.440, 1.706, and 1.476, respectively, and were higher than those recorded for 2003.
Discussion
The findings of this study show that the mean LOS due to geriatric diseases has lengthened every year from 2003 to 2007, although with some variability. In both 2003 and 2007 there were more female patients than male patients, and the mean LOS was longer for female than for male patients. As time has elapsed the intergroup difference has increased. In contrast, according to a community-based study of the factors that affect the use of medical services, and other studies in low-income and general populations, the mean LOS was significantly shorter for female than for male patients.12,13 This difference might be because the present study enrolled only geriatric cases. It was thus expected that the number of female patients with geriatric diseases would increase.
Compared with 2003, the mean LOS and number of patients aged ≥65 years had increasedin 2007, by 3.11 times and 1.77 times, respectively. These results suggest that the number of patients with geriatric diseases and the use of medical services have increased due to the increased number of elderly people. Moreover, the mean LOS and number of patients increased by 1.84 and 1.18 times, respectively, in the 40-64 years age group. These results suggest that preventive measures should be taken against geriatric diseases before the age of 40 years.
While public medical aid accounted for 30.5% and 20.4% of the mean LOS and the number of patients with geriatric diseases, respectively, in 2007, only 3.7% of the NHI scheme was covered by public medical aid.14 This indicates that public medical aid patients commonly have geriatric diseases and they frequently use medical services. People who are covered by public medical aid or Industrial Accident Compensation Insurance are less burdened by paying their own medical expenses than are those who are covered by health insurance.15 Thus, the former group, when in need of hospitalization, tend to receive continuous assistance from healthcare professionals, even though their treatment has been completed, and they might be subjected to long-term hospitalization. In addition, improvements in access to medical services in the public medical aid group might also contribute to the increased use of medical services.
The LOS and the number of patients in the cerebral infarction group were highest in 2003 and 2007 among the four disease groups. This was followed by the dementia group. However, the LOS and the number of patients in the dementia group had increased by 3.8 and 3.5 times, respectively, and were the highest during the same period. It was determined that these marked increases resulted from increased interest in dementia on a nationwide scale and implementation of active measures against it.16 In total, 118 public health centers have implemented measures for the early detection of dementia. It is also planned that this implementation will be extended to a total of 253 public health centers in 2010.
The most striking feature of the comparison between the healthcare institutions was that LOS was markedly longer in the long-term-care hospitals and private clinics than in the tertiary hospitals, general hospitals, and hospitals. Compared with 2003, the mean LOS was similar to or slightly shorter in the tertiary hospitals, general hospitals, and hospitals in 2007. However, the mean LOS was lengthened by 1.26 times in the long-term-care hospitals and 1.3 times in the private clinics.
Those who are subject to hospitalization in long-term-care hospitals include patients with geriatric and chronic diseases and those who are recovering following surgical treatment or trauma.17 With the increased number of elderly people, the incidence of diseases associated with cognitive impairment (Parkinson's disease and dementia) and chronic diseases (cerebral hemorrhage and cerebral infarction)- for which continuous management is necessary-has increased. The purpose of long-term-care hospitals is to maintain the daily lives of patients by introducing active rehabilitation for recovery and maintenance of function after acute treatment.18,19 The results of the present study show that there has been an increase in the number of patients who require medical services at long-term-care hospitals; namely, those with cognitive impairment and chronic diseases. In response to these demands, the number of long-term-care hospitals has increased from 68 (8,355 beds) in 2003 to 571 (66,727 beds) in 2007.20
Once a management system has been established for the subacute, rehabilitation, and chronic phases after acute medical treatment, and this is followed by role-sharing between the medical services and care services, the objectives of long-term-care hospitals can be realized.21 The present study shows that there is role-sharing between hospitals and higher-level institutions that are responsible for the treatment of acute cases, and long-term-care hospitals or private clinics that are responsible for the treatment of subacute or later cases. However, 25% of long-term-care hospitals are not equipped with an appropriate level of medical personnel, and a single physician works at 21% of long-term-care hospitals.22 This hinders the ability of long-term-care hospitals to achieve their goals. Despite the underprivileged environment at some long-term-care hospitals, the number of patients hospitalized therein and the lengthened LOS indicate that the demands of customers (patients or their caregivers) are on care rather than medical services per se.
More studies on LOS due to geriatric diseases have been conducted in overseas countries compared with Korea. In an Australian study of patients aged ≥65 years, the mean LOS was 20.6 days among those with dementia, compared with 9.6 days among other patients.23 In a study from Thailand, the mean LOS for acute stroke patients was 7 days, and the most influential factor for LOS was stroke severity at admission.24 According to a study from the United States regarding patient burden with medical expenses for the treatment of Parkinson's disease, the mean LOS was 5.3 days.25 Due to differences in medical systems, the status of geriatric disease, and access to medical institutions between countries, a simple comparison of LOS would not be useful. However, the present study has revealed that LOS in tertiary and general hospitals is longer in Korea than in other countries.
This study was based on medical insurance claims data. Special attention should thus be paid to the interpretation of this study because there are basic limitations in using such data. First, it is possible that diagnoses on claims data can be overestimated. That is, disease codes for dementia might be included in patients with mild cognitive impairment or those for stroke might be included for brain magnetic resonance imaging evaluation. Second, the diagnostic accuracy might vary with the physicians' clinical experience and diagnostic instruments. Third, the current study dealt only with the primary disease codes. It is thus likely that some data were missing because they were not claimed as the primary disease codes. However, because this study was conducted exclusively using the primary disease codes, it is highly likely that major reasons for hospitalization were the geriatric diseases in question. Furthermore, because this study examined LOS data that were collected from all healthcare institutions, it would be appropriate to compare the LOS based on spatiotemporal changes due to geriatric diseases. That is, this study could overcome the limitations due to the validity of data collected through a patient survey or LOS studies conducted at some healthcare institutions, or those due to the generalization of study results.
This study showed that the LOS due to geriatric diseases has lengthened markedly due to the increased number of hospitalized patients and mean LOS. With regard to the healthcare institutions, the number of patients and mean LOS were particularly markedly increased in long-term-care hospitals. At this time, consideration should be given to examining whether long-term-care hospitals are increasing their size while being faithful to their own purposes, and providing medical treatment and care for appropriate patients, or whether they are increasing their size, being simple service providers responding to an increased demand.
Acknowledgements
This work was supported by Konkuk University in 2010.
Footnotes
The authors have no financial conflicts of interest.
References
- 1.Korea National Statistical Office. Population Projections for Korea. Seoul: Korean National Statistical Office; 2006. pp. 1–56. [Google Scholar]
- 2.Rha JH. Stroke epidemiology 2007 update. Korean J Stroke. 2008;10:1–4. [Google Scholar]
- 3.Jeong HK, Kim YH, Lee JS, Sung JH, Lee SE, Kim JW, et al. Nationwide survey on the prevalence of Parkinson's Disease in Korea. Rep Natl Ins Health. 2007;44:442–445. [Google Scholar]
- 4.Seoul National University Hospital. Nationwide study on the Prevalence of Dementia in Korean Elders. Seoul: Division of Senior Policy, Ministry for Health, Welfare and Family Affairs (MIHWAF); 2009. pp. 122–138. [Google Scholar]
- 5.Enforcement Ordinance of the Long-Term Care Insurance Law for the Elderly. [cited 2010 Oct 10]. Available from: http://likms.assembly.go.kr/law/jsp/main.jsp.
- 6.National Health Insurance Corporation. Trend of treatment for geriatric diseases from 2002 to 2008. Seoul: National Health Insurance Corporation (NHIC); 2009. [Google Scholar]
- 7.Yu SH, Oh DK, Kim YH. The determinants of length of stay in a university hospital. Yonsei Med J. 1983;24:38–45. doi: 10.3349/ymj.1983.24.1.38. [DOI] [PubMed] [Google Scholar]
- 8.Lee HJ, Kim YH, Lee EP, Kim SW, Jeoung BH. An analysis on the effectiveness of hospital revenues per bed by shortening length of stay. Korean J Hosp Manage. 1998;3:100–120. [Google Scholar]
- 9.Suh TW. Length of stay of psychiatric inpatients by sociodemographic and clinical characteristics, and type of facilities. J Korean Neuropsychiatr Assoc. 2002;41:1174–1184. [Google Scholar]
- 10.Lee YM, Kim JH, Lee HY, Jeong YK, Lim KY, Lee JH, et al. Length of stay in the mental health facilities in Korea. J Korean Neuropsychiatr Assoc. 1998;37:83–94. [Google Scholar]
- 11.Kim SJ, Yu SH, Oh HJ. Factors associated with length of stay in elderly inpatients in a general hospital in Seoul. Korean J Hosp Manage. 2007;12:25–42. [Google Scholar]
- 12.Lee H, Lee T, Jeon B, Jung Y. Factors related to health care utilization in the poor and the general populations. Korean J Health Econ Policy. 2009;15:79–106. [Google Scholar]
- 13.Kim SB, Kang PS. Utilization rate of medical facility and its related factors in Taegu. Korean J Prev Med. 1989;22:29–44. [Google Scholar]
- 14.National Health Insurance Corporation. 2007 National Health Insurance Statistical Yearbook. Seoul, South Korea: National Health Insurance Corporation, Health Insurance Review & Assessment Service; 2008. [Google Scholar]
- 15.Kang HK. A study on hospital life of long term admitted patients in orthopedic surgery. Seoul: 1982. Master's thesis of Seoul National University. [Google Scholar]
- 16.Heo JH, Kim H, Bae HJ, Lee K, Bae MH, Lee JB. Trend in treatment of dementia by benefit cost status based on Health Insurance Review & Assessment Service (HIRA)'s Data from 2003 to 2007. Dement Neurocognitive Disord. 2010;9:29–35. [Google Scholar]
- 17.Korean Neurological Association. Role and future of neurology in geriatric medicine. Seoul: Korean Neurological Association; 2009. pp. 9–26. [Google Scholar]
- 18.Park IS, Kim SK. Korean elderly long-term care insurance system and long-term care hospital. J Korean Geriatr Soc. 2008;12:68–73. [Google Scholar]
- 19.Kim DH, Jang HJ, Jang JS, Cho KH. The perspectives on development of Korean quality measurement tools for geriatric hospitals. J Korean Geriatr Soc. 2008;12:191–200. [Google Scholar]
- 20.National Health Insurance Corporation. 2008 National Health Insurance Statistical Yearbook. Seoul, South Korea: National Health Insurance Corporation, Health Insurance Review & Assessment Service; 2009. [Google Scholar]
- 21.Sohn MK, Cho KH, Kim BO, Han SM. Discharge destinations after acute rehabilitation care. J Korean Acad Rehabil Med. 2003;27:269–274. [Google Scholar]
- 22.Park IS, Kim SK. Korean elderly long-term care insurance system and long-term care hospital. J Korean Geriatr Soc. 2008;12:68–73. [Google Scholar]
- 23.King B, Jones C, Brand C. Relationship between dementia and length of stay of general medical patients admitted to acute care. Australas J Ageing. 2006;25:20–23. [Google Scholar]
- 24.Chang KC, Tseng MC, Weng HH, Lin YH, Liou CW, Tan TY. Prediction of length of stay of first-ever ischemic stroke. Stroke. 2002;33:2670–2674. doi: 10.1161/01.str.0000034396.68980.39. [DOI] [PubMed] [Google Scholar]
- 25.O'Brien JA, Ward A, Michels SL, Tzivelekis S, Brandt NJ. Economic burden associated with Parkinson disease. Drug Benefit Trends. 2009;21:179–190. [Google Scholar]