Abstract
Background
Seborrheic keratoses are the most common skin lesions known to contain small white or yellow structures called milia-like cysts (MLCs). Varied appearances can sometimes make it difficult to differentiate benign lesions from malignant lesions such as melanoma, the deadliest form of skin cancer found in humans.
Objective
The purpose of this study was to determine the statistical occurrence of MLCs in benign vs. malignant lesions.
Methods
A medical student with 10 months experience in examining approximately 1000 dermoscopy images and a dermoscopy-naïve observer analysed contact non-polarized dermoscopy images of 221 malignant melanomas and 175 seborrheic keratoses for presence of MLCs.
Results
The observers found two different types of MLCs present: large ones described as cloudy and smaller ones described as starry. Starry MLCs were found to be prevalent in both seborrheic keratoses and melanomas. Cloudy MLCs, however, were found to have 99.1% specificity for seborrheic keratoses among this group of seborrheic keratoses and melanomas.
Conclusion
Cloudy MLCs can be a useful tool for differentiating between seborrheic keratoses and melanomas. Received: 18 June 2010; Accepted: 27 October 2010
Keywords: melanoma, milia-like Cyst, seborrheic Keratosis
Introduction
Milia-like cysts (MLCs) are dermoscopic structures that have been described as ‘variously sized, white or yellowish, roundish structures’.1 MLCs are ‘seen in certain cutaneous lesions, particularly seborrheic keratoses and congenital melanocytic nevi’.2,3 MLCs have been shown to be useful in distinguishing melanomas from benign lesions.1,4 The purpose of this study was to characterize those MLCs that can best distinguish melanoma from seborrheic keratoses.
Methods
Contact non-polarized dermoscopy images (DermLite Fluid; 3Gen LLC, San Juan Capistrano, CA) of seborrheic keratoses and melanomas were analysed. Two types of MLCs were observed with dermoscopy (Fig. 1). Small MLCs are less than 1/3 mm in diameter. They are the most common type of MLC. They are round and often appear like stars on a misty night, with bright centres and variably sharp borders. We refer to these as ‘starry’ MLCs (Figs 1–3). MLCs greater than 1/3 mm in diameter appear less frequently. These larger MLCs possess a fluffy, cloud-like border and an approximately oval shape that lacks significant irregularities. The discernibly non-circular, approximately oval shape and the fluffy border suggest the description ‘cloudy’ for these MLCs (Figs 1 and 4).
Figure 1.

Seborrheic keratosis with a cloudy MLC and multiple starry MLCs.
Figure 3.
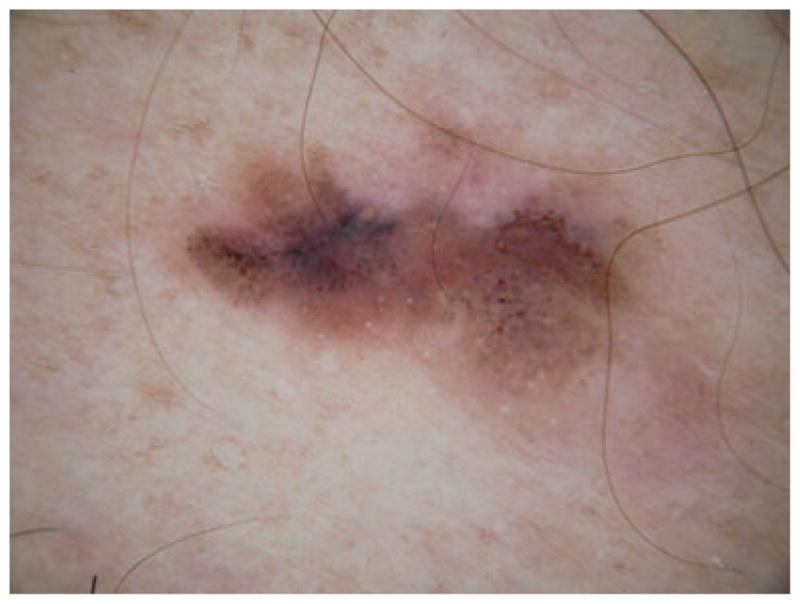
Invasive melanoma 0.63 mm thick with multiple starry MLCs, indicating evolution from a congenital naevus.
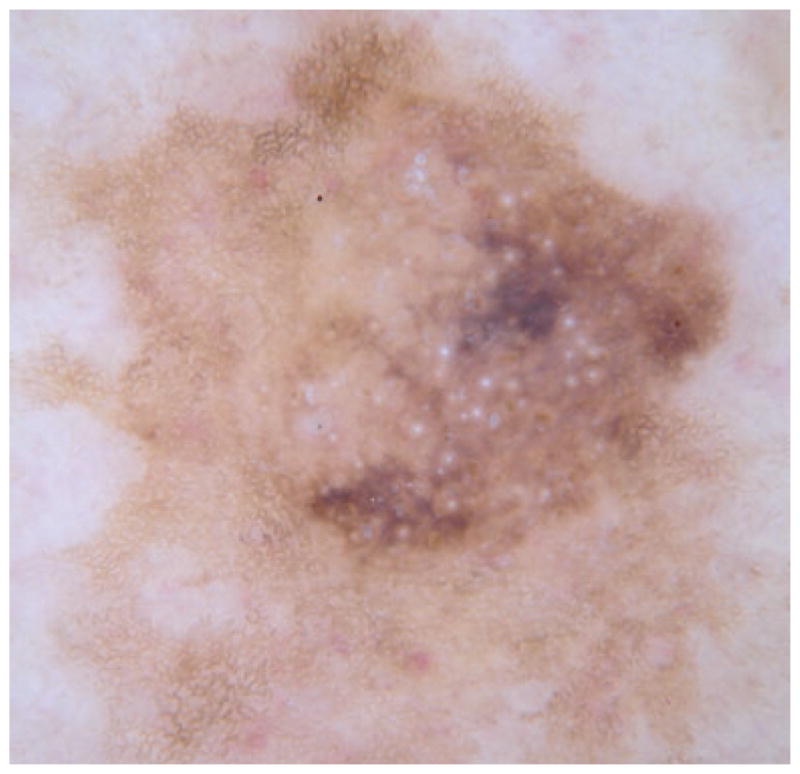
Figure 4.

A lesion that clinically resembled a melanoma (inset); the cloudy MLCs among multiple starry MLCs suggest a seborrheic keratosis, confirmed with histopathology.
In order to determine statistically the likelihood of cloudy and starry MLCs appearing in melanomas vs. seborrheic keratoses, 396 contact non-images were analysed for occurrence of each type of MLC. The images were a convenience sample of lesions obtained from January 2007 to February 2010, per protocol for NIH R44 CA-101639-02A2, approved by Phelps County Regional Medical Center Institutional Review Board. Histopathology results were obtained for all 221 melanomas analysed (128 of which were melanomas in situ) and 113 of the 175 seborrheic keratoses. All seborrheic keratoses not biopsied were determined to be seborrheic keratoses both clinically and dermoscopically.
The assessment of MLCs present in each image was scored as follows: starry MLCs, cloudy and starry MLCs, cloudy MLCs or no MLCs. The possibility of bias entering in the study was recognized. An experienced observer would know the diagnosis of a dermoscopy image in most cases, and this could influence the assignment of the types of MLCs present. A naïve observer, unaware of the project’s hypothesis, with no previous dermoscopy background and therefore no experience in distinguishing melanomas from seborrheic keratoses was trained in recognizing MLCs. Each image was scored independently by the naïve observer (S.K.M) and by a trained observer with knowledge of the different diagnoses (S.M.S).
Small keratin scales, the most problematic competing structures, were distinguished from MLCs by their irregular borders, noise within the area and asymmetry. The irregular borders and the noise were determined as clearly as possible by zooming in on images. The resolution of 1024 × 768 pixels allowed clear differentiation of MLCs from scales. Gel bubbles tend to be more grey or transparent in appearance and generally have a smaller circle within the outer bubble ring. Difficult bubbles more closely resembling MLCs were tested by comparing the image with another type of contact dermoscopy (polarized) image taken the same day. If the area in question was not in the same spot in both images, then it was determined to be a bubble. Tiny pigment network holes5 were differentiated from MLCs by a ring of pigment surrounding lighter skin colouring. For cloudy MLCs, the size was confirmed by analysis of the fully zoomed DermLite fluid images that are 9-mm across. A scale was then calibrated to measure 1/3 mm in relation to the image. For images that had been zoomed out, there was a scale in millimetres on the image. This scale was then used to calibrate 1/3 mm in relation to these images.
Results
The two observers disagreed on 10.9% of the images, but were able to reduce the disagreement on all but approximately 5%. In differentiating between borderline MLCs that included smaller cloudy and larger starry MLCs, a more controlled approach was taken using a scale and displaying all the images on the same computer screen. The remaining differing assessments were arbitrated by an experienced dermoscopist (W.V.S). After complete consensus was achieved by the two observers and a dermatologist, the odds ratio, sensitivity and specificity were calculated for both starry and cloudy MLCs.6 For starry MLCs, our analysis showed an odds ratio of 8.0 (4.7–13.7) with a 90.5% sensitivity and 45.7% specificity for a diagnosis of seborrheic keratosis vs. all melanomas. An odds ratio of 27.4 (7.2–104.4) with 20.0% sensitivity and 99.1% specificity was obtained for seborrheic keratoses having a cloudy MLC vs. melanomas. Odds ratios, usually denoting the odds of a malignant diagnosis for a given sign, are given here as the odds of a benign diagnosis for the given sign.
Discussion
Due to incomplete separation of malignant from benign lesions, especially for the more common starry MLCs, one model for discriminating amelanotic and hypomelanotic melanomas developed by Menzies et al includes the number of MLCs – when there are three or more MLCs present, the model uses this feature to predict a benign lesion.4 No size distinction was given for MLCs in the three-or-greater model.4 If there is no discrimination by size and tiny (starry) MLCs are considered equivalent to large (cloudy) MLCs, melanomas with a congenital naevus precursor (Fig. 3) will be counted benign. The Menzies study included only amelanotic/hypomelanotic melanomas and did not separate starry and cloudy MLCs, therefore findings of that study are not strictly comparable to our findings.
The most difficult objective in the study was separating MLCs from competing structures such as small areas of keratin scale, bubbles from the contact dermoscopy fluid interface and tiny pigment network holes, which may resemble starry MLCs.5 The techniques outlined in Methods allowed discrimination of these structures.
In our experience, cloudy MLCs are rarely seen in melanomas, as only two of 221 melanomas had cloudy MLCs. Cloudy MLCs appear to be more useful than starry MLCs as a ‘benign sign’. However, as cloudy MLCs were not found to be pathognomonic, other factors present in the clinical and dermoscopy presentation should always be considered alongside the cloudy MLC sign.
Figure 2.
Seborrheic keratosis with multiple starry MLCs.
Acknowledgments
Rhett Drugge, MD and Lindall Perry, MD supplied images used in the statistical analysis.
Funding support
This publication was made possible by Grant Number SBIR R44 CA-101639-02A2 of the National Institutes of Health (NIH).
Footnotes
Conflict of interest
None reported.
References
- 1.Argenziano G, Soyer HP, Chimenti S, et al. Dermoscopy of pigmented skin lesions: results of a consensus meeting via the internet. J Am Acad Dermatol. 2003;48:679–693. doi: 10.1067/mjd.2003.281. [DOI] [PubMed] [Google Scholar]
- 2.Changchien L, Dusza SW, Agero AL, et al. 1. Age- and site-specific variation in the dermoscopic patterns of congenital melanocytic nevi: an aid to accurate classification and assessment of melanocytic nevi. 1. Arch Dermatol. 2007;143:1007–1014. doi: 10.1001/archderm.143.8.1007. [DOI] [PubMed] [Google Scholar]
- 3.Berk DR, Bayliss SJ. Milia: a review and classification. J Am Acad Dermatol. 2008;59:1050–1063. doi: 10.1016/j.jaad.2008.07.034. [DOI] [PubMed] [Google Scholar]
- 4.Menzies SW, Kreusch J, Byth K, et al. Dermoscopic evaluation of amelanotic and hypomelanotic melanoma. Arch Dermatol. 2008;144:1120–1127. doi: 10.1001/archderm.144.9.1120. [DOI] [PubMed] [Google Scholar]
- 5.Burroni M, Nami N, Rubegni P. Like milia-like cysts. Skin Res Technol. 2009;15:250–251. doi: 10.1111/j.1600-0846.2009.00349.x. [DOI] [PubMed] [Google Scholar]
- 6.Pezzullo John C. [last accessed 6 June 2010];2-way contingency table analysis. 2010 Available at: http://statpages.org/ctab2x2.html.


