Abstract
Background
Limited health literacy is associated with higher rates of hospitalization. However, the prevalence and etiology of limited health literacy among hospitalized adults and the compensatory strategies used are not known.
Objectives
To determine the prevalence and demographic associations of limited health literacy in hospitalized patients and to identify the perceived etiology and use of any compensatory strategies.
Method
A cross-sectional study was implemented of a consecutive sample of hospitalized adults admitted to the Internal Medicine Hospitalist Service at a 440-bed academic medical center (n = 103) in Vermont. Health literacy was determined using the short form of the Test of Functional Health Literacy in Adults. Demographic data, perceived etiology of difficulties in reading or understanding health information, and use of compensatory strategies were self-reported.
Results
Sixty percent of medical inpatients have limited health literacy. Thirty six percent of patients with limited health literacy attribute this to difficulties with vision. Sixty two percent of all medical inpatients rely on help from a health professional and 23% look to a family member when faced with challenges in reading or understanding health information.
Discussion
The prevalence of limited health literacy is high in hospitalized medical patients. Further study of the timing and methods of communicating information to hospitalized patients is warranted. Assuring that the patient and/or family understand the post-discharge plans will be an important step to improving quality and safety.
Keywords: health literacy, communication, patient teaching
Adequate health literacy skills--“having the ability to obtain, process, understand, and communicate about health-related information needed to make informed health decisions” (Berkman, Davis, & McCormack, 2010, pp. 16)--are necessary in today’s hospital environment. However, communication during hospitalization is less than ideal; patients report difficulty in understanding their diagnoses (Makaryus & Friedman, 2005), treatment options (Kim et al., 2001), discharge medication regimens (Kripalani, Henderson, Jacobson, & Vaccarino, 2008; Maniaci, Heckman, & Dawson, 2008), and posthospital self-care instructions (Flacker, Park, & Sims, 2007).
More than one third of adults in the United States have limited health literacy (Kutner, Greenberg, Jin, & Paulsen, 2006). Individuals with limited health literacy are less knowledgeable about their disease and its management (Fang, Machtinger, Wang, & Schillinger, 2006; Kim et al., 2001; Lindau et al., 2002; Williams, Baker, Parker, & Nurss, 1998) and are less likely to understand prescription instructions (Davis et al., 2006) or to interpret appointment slips correctly (Baker, Parker, Williams, & Clark, 1998). Limited health literacy also is associated with lower patient ratings of physician-patient communication (Kripalani et al., 2010), and higher rates of hospitalization (Baker et al., 1998, Baker, Gazmararian, Williams, et al., 2002) and mortality (Baker et al., 2007; Sudore et al., 2006).
Limited health literacy has been reported in 33–51% of adults in outpatient settings (Gazmararian et al., 1999; Schillinger et al., 2002; Walker, Pepa, & Gerard, 2010; Williams et al., 1998; Wolf et al., 2007) and in 15–50% of adults in emergency departments (Ginde, Clark, Goldstein, & Camargo, 2008; Ginde, Weiner, Pallin, & Camargo, 2008; Olives, Patel, Patel, Hottinger, & Miner, 2010). A lower prevalence rate of 17% has been reported in a study of outpatient adults with diabetes in northern New England (Morris, MacLean & Littenberg, 2006). Only one study was found focusing on hospitalized patients, specifically those with acute coronary syndromes, and 44% were found to have inadequate health literacy (Kripalani et al., 2010). The hospital is a particularly challenging environment with complex and often unfamiliar information conveyed to patients in a typically stressful and compressed time frame.
Health literacy is associated with cognitive status (Waldrop-Valverde, Gould, Kumar & Ownby, 2010; Wilson et al., 2010). Some patients experience a transient change in cognition following major surgery (Ramaiah & Lam, 2009), but the prevalence of this is not known. Recently, Lindquist and colleagues (2011) reported that almost 1/3 of hospitalized adults over 70 years of age without dementia displayed transient cognitive impairment at discharge One measurement of health literacy, the Short-Test of Functional Health Literacy of Adults (S-TOFHLA) is correlated with performance on the Mini-Mental State Examination (Baker, Gazmararian, Sudano, et al., 2002), suggesting that cognitive change influences reading comprehension.
The concept of health literacy is comprehensive and extends beyond the ability to read and understand health information. However, these skills are key components of health literacy and generally required for successful discharge teaching in the hospital setting. Given the amount of information exchanged with patients during an inpatient stay, the importance of providing clear post-hospital care instructions and guidance, and the association of limited health literacy to health outcomes, the purpose of this study was to determine the prevalence and demographic associations of limited health literacy in hospitalized General Medicine patients.
Patients were queried about what makes it hard for them to read and what they typically do when faced with challenges in understanding health information. The specific research questions were: (a) What is the prevalence of limited health literacy in hospitalized medical patients? (b) What explanations do patients give for difficulties reading health information? and (c) What do patients do when they need help reading or understanding health information? The findings will add to understanding of health literacy and provide data to develop and test interventions to improve communicating health information in the hospital.
Method
A cross-sectional survey was conducted of a convenience sample of patients admitted to the Internal Medicine Hospitalist Service at Fletcher Allen Health Care, a 440-bed teaching hospital affiliated with the University of Vermont. Eligible patients were at least 18 years of age, able to provide informed consent, not incarcerated, and not hospitalized for end-of-life care. Common diagnoses included cardiovascular disease, congestive heart failure, pneumonia, cardiac arrhythmias, chronic obstructive lung disease, and skin and subcutaneous infections. The University of Vermont Institutional Review Board approved the study and all patients provided written informed consent.
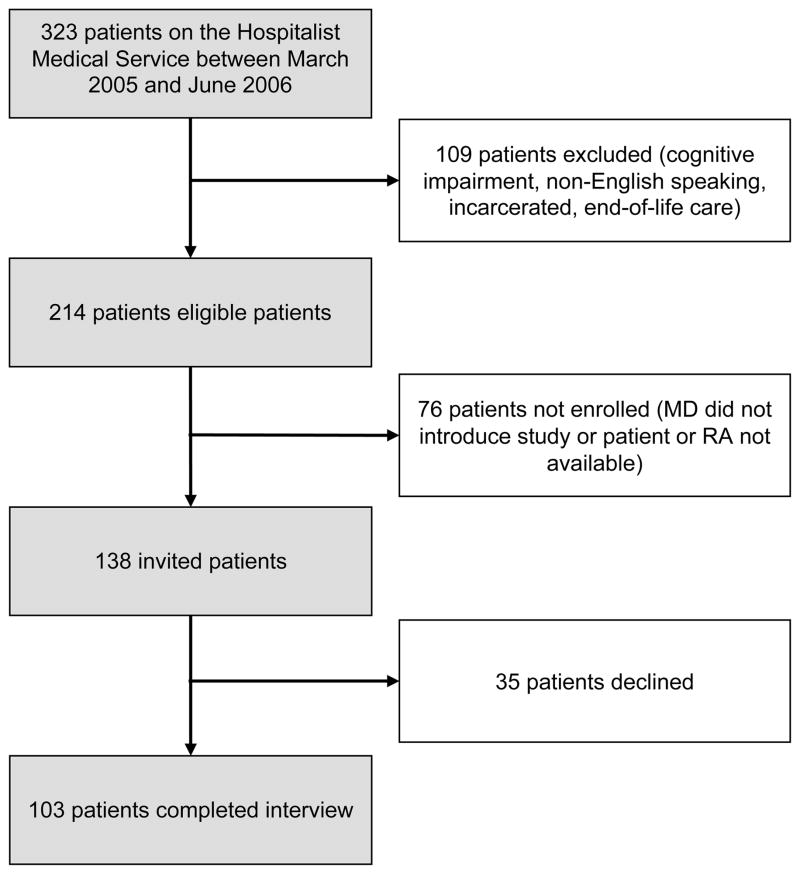
The patient’s attending physician introduced the study and alerted a trained research assistant to those interested in participating. To minimize the contribution of the acute illness to limited health literacy, data were collected within 48 hours of anticipated discharge from the hospital. This also allowed assessment of health literacy close to the time patients are typically given information about postdischarge care and follow-up plans. The research assistant obtained informed consent and collected data from all patients available Monday through Friday during workday hours. Of 247 patients considered, 109 did not meet eligibility criteria and 35 declined to participate (Figure 1).
Figure 1.
Patients were asked if they wore glasses and the research assistant encouraged them to put them on before data collection began. Reading glasses were made available to those with presbyopia. All survey questions and response choices were presented in 18-point font. All surveys, except the Short Test of Functional Health Literacy of Adults (S-TOFHLA), were read aloud to the patient.
Measurements
All patients completed the S-TOFHLA, a measure of health literacy (Baker, Williams, Parker, Gazmararian, & Nurss, 1999). The S-TOFHLA is a 36-item, 7-minute, timed test of reading comprehension as measured by the Cloze procedure, in which a word in a sentence is omitted and must be chosen from a multiple choice list. It uses passages from instructions for preparation for an upper gastrointestinal series and from a Medicaid application. As is customary, results are categorized into inadequate (0–16 correct answers), marginal (17–22 correct answers), and adequate health literacy (23–36 correct answers). Inadequate and marginal health literacy were combined; both groups are referred to as having limited health literacy, referring to all subjects who may need additional support to obtain and comprehend health information. The S-TOFHLA has good internal consistency (Cronbach’s alpha = 0.98 for all items combined) and concurrent validity compared to the longer Test of Functional Health Literacy of Adults (TOFHLA; r = 0.91; Baker et al., 1999).
To identify factors contributing to the challenges of communicating clearly, the research assistant asked each patient “Do any of these problems make it hard for you to read?” The patient was shown a card with the following options which were read aloud as the patient looked at the card: blindness or decreased vision; decreased hearing; primary language other than English; memory problems or dementia, mental, or neurologic problems; emotional or psychiatric problems; not enough schooling to learn to read; and dyslexia or reading disorder. Patients could select more than one of the reasons offered or provide another explanation that was recorded as other.
To assess compensatory strategies, patients were asked, “What would you do if you needed help reading or understanding medical directions or health information?” The question was open-ended, but if they did not respond spontaneously, the research assistant offered the following options to assist the patient in answering the question: ask a family member for help, ask a friend for help, ask a health care professional for help, ask a translator for help, or use a magnifying glass. Other responses were recorded as other with a description of the specific strategy.
After completion of the S-TOFHLA and the two single-item questions, patients were queried about their demographics. Data collected included: sex, age, race, marital status, language spoken in the home, highest level of education, and household income.
Analysis
Proportions and means were used to summarize the data. To compare subgroups, we used Chi-square tests and Cuzick’s nonparametric test for trend across ordered categories (Cuzick, 1985). A p-value of < .05 was required for statistical significance. To assess the demographic correlates of adequate health literacy, income was dichotomized as Less than $30,000 per year or not (including nonrespondents in the low income group), education as High School Graduate or not, and marital status as Currently Married or not. Stepwise backward logistic regression with a threshold of p < .05 was applied to retain independent variables. All analyses were performed using STATA 10.1.
Results
The mean age of the study population was 64 years (SD = 16, range 23–92). Ninety-nine percent of participants used English as their primary language, 91% were White, 61% were female, and 27% had a college education. Over half of the participants reported an annual home income of less than $30,000 (Table 1).
Table 1.
Characteristics of 103 Hospitalized Adults by Literacy Level
| Characteristics | All Subjects | Inadequate Literacy | Marginal Literacy | Adequate Literacy | p* |
|---|---|---|---|---|---|
| Number of subjects, (%) | 103 | 55 (53%) | 9 (9%) | 39 (38%) | |
| S-TOFHLA, range | 0–36 | 0–16 | 17–22 | 23–36 | |
| S-TOFHLA, mean ± SD | 16 ± 14 | 5 ± 6 | 19 ± 2 | 32 ± 4 | |
| Age in years, mean ± SD | 64 ± 16 | 70 ± 14 | 68 ± 10 | 56 ± 16 | < .001 |
| Female, n (%) | 63 (61%) | 35 (64%) | 3 (33%) | 25 (64%) | .96 |
| White race, n (%) | 94 (91%) | 47 (85%) | 9 (100%) | 38 (97%) | .03 |
| Married, n (%) | 44 (43%) | 20 (36%) | 5 (56%) | 19 (49%) | .22 |
| Annual income < $30,000, n (%) | 52 (58%) | 34 (76%) | 5(58%) | 13 (36%) | .004 |
| Education, n (%) | .015 | ||||
| Less than HS graduate | 21 (20%) | 14 (25%) | 4 (44%) | 3 (8%) | |
| High school graduate | 54 (52%) | 30 (55%) | 3 (33%) | 21 (54%) | |
| College graduate | 28 (27%) | 11 (20%) | 2 (22%) | 15 (38%) |
Notes.
p-values calculated by the Cuzick nonparametric test for ordered categories.
The mean S-TOFLA score was 16 (range = 0 to 36; SD = 14). Sixty percent (CI = 50–70%) had inadequate (n = 55) or marginal health literacy (n = 7). Only 40% (n = 41) of patients had adequate health literacy. The patients in the lowest literacy group were significantly older (p < .001), less educated (p = .015), with lower earnings (p < .001), and less often White (p = .03; Table 1). There were no significant differences in their sex, marital status, primary language, reasons given for reading problems, or the compensatory strategies reported. In multiple logistic regression, health literacy was associated significantly with age, education, income and sex, but not marital status or race (Table 2).
Table 2.
Association of Demographic Characteristics with Adequate Health Literacy in 103 Patients by Multiple Logistic Regression
| Characteristic | Odds Ratio | SE | 95% CI | p |
|---|---|---|---|---|
| Age (years) | 0.93 | 0.02 | 0.89 – 0.97 | < .001 |
| High School Graduate | 4.81 | 3.68 | 1.08 – 21.5 | .04 |
| Income <$30K | 0.18 | 0.10 | 0.06 – 0.53 | .002 |
| Female Sex | 3.71 | 2.30 | 1.10 – 12.50 | .03 |
Notes. Because race and marital status were not associated significantly with adequate health literacy in the multiple regression, they were eliminated according to the stepwise procedure.
When queried about why, in general, patients thought they had difficulty reading or understanding health information, the most common explanation selected was decreased vision (33% of all subjects) followed by decreased hearing (7%). Six percent of the patients noted that their difficulty with reading was related to memory problems, mental conditions, neurologic problems, or lack of education. The reasons given did not differ by health literacy (Table 3). The majority of patients (62%) reported that they would seek assistance from a healthcare professional if they were to have difficulty reading or understanding written health information (Table 3). Twenty three percent would rely on family members. Strategies to deal with challenging written health information did not differ by health literacy.
Table 3.
Causes of and Compensatory Strategies for Difficulty Reading Among 103 Inpatients
| Characteristics | All Subjects | Inadequate Literacy | Marginal Literacy | Adequate Literacy | p* |
|---|---|---|---|---|---|
| Reasons given for difficulty reading, n (%) | |||||
| Blindness/low vision | 34 (33%) | 21 (38%) | 2 (22%) | 11 (28%) | .30 |
| Decreased hearing | 7 (7%) | 5 (9%) | 0 (0) | 2 (5%) | .42 |
| English not first language | 4 (4%) | 4 (7%) | 0 (0) | 0 (0) | .07 |
| Memory | 6 (6%) | 3 (6%) | 0 (0) | 3 (8%) | .70 |
| Mental/neurological | 6 (6%) | 4 (7%) | 1 (11%) | 1 (3%) | .35 |
| Emotional/Psychiatric | 4 (4%) | 1 (2%) | 0 (0) | 3 (8%) | .16 |
| Not enough schooling | 6 (6%) | 4 (8%) | 1 (11%) | 1 (3%) | .34 |
| Dyslexia/reading disorder | 3 (3%) | 2 (4%) | 0 (0) | 1 (3%) | .73 |
| Strategies used to assist with reading or understanding health information, n (%) | .91† | ||||
| Ask health professional | 63 (62%) | 34 (63%) | 5 (56%) | 24 (62%) | |
| Ask family member | 23 (23%) | 11 (20%) | 2 (22%) | 10 (26%) | |
| Ask friend | 5 (5%) | 3 (6%) | 0 (0) | 2 (5%) | |
| Use translator | 1 (1%) | 1 (2%) | 0 (0) | 0 (0) | |
| Other | 10 (10%) | 5 (9%) | 2 (22%) | 3 (8%) | |
Notes.
p-values calculated by the Cuzick nonparametric test for ordered categories (27), except as indicated.
Chi-square test
Discussion
The demographic characteristics of the patients reflect the population of Vermont (United States Census, 2010). This population differs from many other studies on health literacy as it is more educated and less racially and ethnically diverse. Given that this population was generally well-educated and comprised of native English speakers, it was not expected that 60% of the subjects would have limited health literacy. The prevalence is higher than the 33–51% reported in outpatient studies (Gazmararian et al., 1999; Schillinger et al., 2002; Williams et al., 1998; Wolf et al., 2007) and strikingly higher than the 17% prevalence reported in outpatients with diabetes in the same region (Morris, MacLean, & Littenberg, 2006).
There are a few possible explanations for the high prevalence of limited health literacy in hospitalized patients. First, patients with low health literacy are more likely to be admitted to the hospital than those with adequate health literacy (Baker et al., 1998; Baker, Gazmararian, Williams et al., 2002). Second, the transient change in cognition that some adults experience while hospitalized may influence their health literacy. Regardless, these patients’ ability to read was limited and presents a challenge if using print material to provide information or instructions.
The most common explanation offered by patients as to why they have difficulty reading health information was decreased vision. This may be due to age-related vision changes, organic disease, or medications. Patients might also report visual problems to mask their embarrassment at not reading well.
Health literacy may be a dynamic state that fluctuates with contextual factors such as the patient’s health status and physical environment as well as their individual experiences. It may be that the high prevalence of limited health literacy among this group of hospitalized patients reflects transient changes in cognition, vision, or fatigue and that health literacy may improve after discharge or as the underlying reasons for admission improve. If health literacy is lower during hospitalization, the timing and method of transmitting critical information to patients and their families need to be examined. Assessing health literacy in the immediate postdischarge period would provide additional data about the possible dynamic nature of health literacy and, if found to improve, prompt rethinking of the timing of discharge teaching.
Patients’ reliance on healthcare professionals, family, and friends to assist in understanding health information reinforces the need to reconsider existing methods of communicating information to patients. If health literacy is typically lower during hospitalization, identifying the responsible patient- and process-related factors may allow the development of additional effective interventions, which may impact quality and cost of health care.
This study has several limitations. The study population was better educated than populations previously described; if anything this would bias the results to higher health literacy. Despite this, surprisingly low health literacy was found. Although the sample size is relatively small, the small p-values indicate that statistical power is not a major deficiency. Because of the small proportion of non-English-speaking subjects, the results cannot be generalized to those populations. Patients were enrolled only when research staff were available and therefore some eligible patients were missed, particularly those with brief stays who may have been less ill. The attending physician was relied upon to exclude patients with significant cognitive impairment; however, cognitive status was not measured objectively. Also, patients were relied on for self-report regarding their need for glasses and visual acuity was not verified before administering the S-TOFHLA. Although the S-TOFHLA does not measure all of the domains of health literacy, it has been shown to predict knowledge, behaviors, and outcomes (Baker et al., 2007; Fang et al., 2006; Schillinger et al., 2002). The attempt to examine factors contributing to difficulties reading and understanding health information and to identify compensatory strategies was limited to patient self-report. Finally, this was a cross-sectional survey that did not allow the observation of literacy over time, measurement of incident outcomes, or the assignment of cause and effect.
The prevalence of marginal and inadequate health literacy is high in hospitalized medical patients. Developing communication strategies that are effective regardless of the patient’s current state of health literacy may improve recidivism and long-term outcomes.
Acknowledgments
This work was funded, in part, by grants DK68380 and DK61167 from the National Institutes of Health.
Contributor Information
Nancy S. Morris, University of Massachusetts Medical School, Graduate School of Nursing, Worcester, Massachusetts.
Steven Grant, University of Vermont College of Medicine and Associate Director of the Primary Care Internal Medicine Hospitalist Service, Fletcher Allen Health Care, Burlington, Vermont.
Allen Repp, University of Vermont College of Medicine and Director of the Primary Care Internal Medicine Hospitalist Service, Fletcher Allen Health Care, Burlington, Vermont.
Charles MacLean, University of Vermont College of Medicine and Associate Dean for Primary Care, Burlington, Vermont.
Benjamin Littenberg, University of Vermont Henry and Carleen Tufo Professor College of Medicine and Professor Nursing and Health Sciences, Burlington, Vermont.
References
- Baker DW, Gazmararian JA, Sudano J, Patterson M, Parker RM, Williams MV. Health literacy and performance on the Mini-Mental State Examination. Aging & Mental Health. 2002;6:22–29. doi: 10.1080/13607860120101121. [DOI] [PubMed] [Google Scholar]
- Baker DW, Gazmararian JA, Williams MW, Scott T, Parker RM, Green D, …Peel J. Functional health literacy and the risk of hospital admission among Medicare managed enrollees. American Journal of Public Health. 2002;92:1278–1283. doi: 10.2105/ajph.92.8.1278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baker DW, Parker RM, Williams MV, Clark WS. Health literacy and the risk of hospital admission. Journal of General Internal Medicine. 1998;13:791–798. doi: 10.1046/j1525-1497.1998.00242.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baker DW, Williams MV, Parker RM, Gazmararian JA, Nurss J. Development of a brief test to measure functional health literacy. Patient Education and Counseling. 1999;38:33–42. doi: 10.1016/S0738-399(98)00116-5. [DOI] [PubMed] [Google Scholar]
- Baker DW, Wolf MS, Feinglass J, Thompson JA, Gazmararian JA, Huang J. Health literacy and mortality among elderly persons. Archives of Internal Medicine. 2007;167:1503–1509. doi: 10.1001/archinte.167.14.1503. [DOI] [PubMed] [Google Scholar]
- Berkman ND, Davis TC, McCormack L. Health literacy: What is it? Journal of Health Communication. 2010;15(Suppl 2):9–19. doi: 10.1080/10810730.2010.499985. [DOI] [PubMed] [Google Scholar]
- Cuzick JA. A Wilcoxon-type test for trend. Statistics in Medicine. 1985;4:87–90. doi: 10.1002/sim.4780040112. [DOI] [PubMed] [Google Scholar]
- Davis TC, Wolf MS, Bass PF, 3rd, Middlebrooks M, Kennen E, Baker DW, Parker RM. Low literacy impairs comprehension of prescription drug warning labels. Journal of General Internal Medicine. 2006;21:847–851. doi: 10.1111/j.1525-1497.2006.00529.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fang MC, Machtinger EL, Wang F, Schillinger D. Health literacy and anticoagulation-related outcomes among patients taking warfarin. Journal of General Internal Medicine. 2006;21:841–846. doi: 10.1111/j.1525-1497.2006.00537.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flacker J, Park W, Sims A. Hospital discharge information and older patients: Do they get what they need? Journal of Hospital Medicine. 2007;2:291–296. doi: 10.1002/jhm.166. [DOI] [PubMed] [Google Scholar]
- Gazmararian JA, Baker DW, Williams MV, Parker RM, Scott TL, Green DC, …Koplan JP. Health literacy among Medicare enrollees in a managed care organization. JAMA. 1999;281:545–551. doi: 10.001/jama.281.6.545. [DOI] [PubMed] [Google Scholar]
- Ginde AA, Clark S, Goldstein JN, Camargo CA., Jr Demographic disparities in numeracy among emergency department patients: Evidence from two multicenter studies. Patient Education and Counseling. 2008;72:350–356. doi: 10.1016/j.pec.2008.03.012. [DOI] [PubMed] [Google Scholar]
- Ginde AA, Weiner SG, Pallin DJ, Camargo CA., Jr Multicenter study of limited health literacy in emergency department patients. Academic Emergency Medicine. 2008;15:577–580. doi: 10.2222/j.1553-2712.2008.00116.x. [DOI] [PubMed] [Google Scholar]
- Kim SP, Knight SJ, Tomori C, Collella KM, Schoor RA, Shih L, …Bennett CL. Health literacy and shared decision making for prostate cancer patients with low socioeconomic status. Cancer Investigation. 2001;19:684–691. doi: 10.1081/cnv-100106143. [DOI] [PubMed] [Google Scholar]
- Kripalani S, Henderson LE, Jacobson TA, Vaccarino V. Medication use among inner-city patients after hospital discharge: patient reported barriers and solutions. Mayo Clinic Proceedings. 2008;83:529–535. doi: 10.4065/83.5.529. [DOI] [PubMed] [Google Scholar]
- Kripalani S, Jacobson TA, Mugalla IC, Cawthon CR, Niesner KJ, Vaccarino V. Health literacy and the quality of physician-patient communication during hospitalization. Journal of Hospital Medicine. 2010;5:269–275. doi: 10.1002/jhm.667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kutner M, Greenberg E, Jin Y, Paulsen C. The Health Literacy of America’s Adults: Results From the 2003 National Assessment of Adult Literacy (NCES 2006–483) U.S. Department of Education; Washington, DC: National Center for Education Statistics; 2006. Retrieved from http://nces.ed.gov/pubs2006/2006483.pdf. [Google Scholar]
- Lindau ST, Tomori C, Lyons T, Langseth L, Bennett CL, Garcia P. The association of health literacy with cervical cancer prevention knowledge and health behaviors in a multiethnic cohort of women. American Journal of Obstetrics and Gynecology. 2002;186:938–943. doi: 10.1067/mob.2002.122091. doi: 10-1067/mob.2002.122091. [DOI] [PubMed] [Google Scholar]
- Lindquist LA, Go L, Fleisher J, Jain N, Baker D. Improvement in cognition following hospital discharge of community dwelling seniors. J Gen Intern Med. 2011;26(7):765–770. doi: 10.1007/s11606-011-1681-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Makaryus AN, Friedman EA. Patients’ understanding of their treatment plans and diagnosis at discharge. Mayo Clinic Proceedings. 2005;80:991–994. doi: 10.4065/80.8.991. [DOI] [PubMed] [Google Scholar]
- Maniaci MJ, Heckman MG, Dawson NL. Functional health literacy and understanding of medications at discharge. Mayo Clinic Proceedings. 2008;83:554–558. doi: 10.4065/83.5.554. [DOI] [PubMed] [Google Scholar]
- Morris NS, MacLean CD, Littenberg B. Literacy and health outcomes: A cross-sectional study in 1002 adults with diabetes. BMC Family Practice. 2006;7:49. doi: 10.1186/1471-2296/7/49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olives T, Patel R, Patel S, Hottinger J, Miner JR. Health literacy of adults presenting to an urban ED. The American Journal of Emergency Medicine. 2010 doi: 10.1016/j.ajem.2010.03.031. Advance online publication. [DOI] [PubMed] [Google Scholar]
- Ramaiah R, Lam AM. Postoperative cognitive dysfunction in the elderly. Anesthesiol Clin. 2009;27(3):485–496. doi: 10.1016/j.anclin.2009.07.011. [DOI] [PubMed] [Google Scholar]
- Schillinger D, Grumbach K, Piette J, Wang F, Osmond D, Daher C, …Bindman AB. Association of health literacy with diabetes outcomes. JAMA. 2002;288:475–482. doi: 10.1001/jama.288.4.475. [DOI] [PubMed] [Google Scholar]
- Sudore RL, Yaffe K, Satterfield S, Harris TB, Mehta KM, Simonsick EM, …Schillinger D. Limited literacy and mortality in the elderly: The health, aging, and body composition study. Journal of General Internal Medicine. 2006;21:806–812. doi: 10.1111/j.1525-1497.2006.00539.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- United States Census. Profile of general demographic characteristics: 2000. 2010 Retrieved from http://censtats.census.gov/data/VT/04050.pdf.
- Waldrop-Valverde D, Jones DL, Gould F, Kumar M, Ownby RL. Neurocognition, health-relted reading literacy, and numeracy in medication management for HIV infection. AIDS Patient Care STDS. 2010;24(8):477–484. doi: 10.1089/apc.2009.0300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walker J, Pepa C, Gerard PS. Assessing the health literacy levels of patients using selected hospital services. Clinical Nurse Specialist. 2010;24:31–37. doi: 10.1097/NUR.0b013e3181c4abd0. [DOI] [PubMed] [Google Scholar]
- Williams MV, Baker DW, Parker RM, Nurss JR. Relationship of functional health literacy to patients’ knowledge of their chronic disease: A study of patients with hypertension and diabetes. Archives of Internal Medicine. 1998;158:166–172. doi: 10.1001/archinte.158.2.166. [DOI] [PubMed] [Google Scholar]
- Wilson WAH, Wolf MS, Curtis IM, Clayman ML, Cameron KA, VomEigen K, Makoul G. Literacy, cognitive ability, and the retention of health-related information about colorectal cancer screening. Jounral of Health Communication. 2010;15:116–125. doi: 10.1080/10810730.2010.499984. [DOI] [PubMed] [Google Scholar]
- Wolf MS, Williams MV, Parker RM, Parikh NS, Nowlan AW, Baker DW. Patients’ shame and attitudes toward discussing the results of literacy screening. Journal of Health Communication. 2007;12:721–732. doi: 10.1080/108107307001672173. [DOI] [PubMed] [Google Scholar]