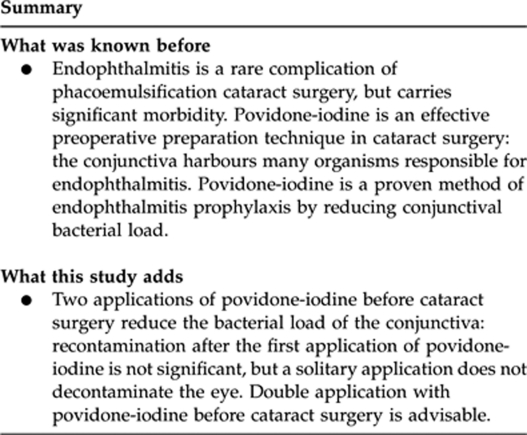
Abstract
Aims
This study assessed the effectiveness of one vs two applications of povidone-iodine in decontaminating the eye before cataract surgery.
Methods
This was a prospective, interventional study of 52 patients having elective unilateral phacoemulsification cataract surgery in a tertiary care centre. Each patient had two applications of povidone-iodine before phacoemulsification cataract surgery, separated by 10 min. Conjunctival swabs were taken before and after each application and cultured in 5% CO2 and anaerobically. Statistical analysis was performed using McNemar's test for correlated proportions.
Results
In all, 15 of 52 (29%) patients had positive cultures before the first application and 21 of 52 (40%) patients had positive cultures after it. This was not statistically significant (P=0.239). A total of 25 of 52 (48%) patients were culture positive before the second application. This was not statistically significantly different from 10 min earlier (P=0.423). Six of 52 (12%) patients were positive after the second application (P<0.001).
Conclusions
We conclude that the initial application of povidone-iodine was not effective in decontaminating the eye. Recontamination did not take place between applications. The difference in the proportion of patients with positive results before and after the second application of povidone-iodine was statistically significant. We infer from this that double application of povidone-iodine before cataract surgery is advisable.
Keywords: phacoemulsification, cataract extraction, povidone–iodine, prophylaxis, antiseptic
Introduction
Ongoing contamination of the conjunctiva from organisms present on the eyelid margin results in organisms being found on the conjunctiva. There is however no colonization of the conjunctiva; hence, it harbours no predominant organisms. Organisms present on the eyelid margin, and in turn the conjunctiva, as a result of contamination, include Diphtheroids, Staphylococcus epidermidis, and Streptococcus species. Neisseriae, Gram-negative bacilli (often Moraxella species), Propionibacterium acnes, viridans streptococci, S. aureus, and fungi may also be present.1, 2, 3
Povidone-iodine has a broad spectrum of microbicidal effects4 against various bacteria, as well as fungi, protozoa, and viruses.5 Polyvinylpyrrolidone has a high affinity for cell membranes and delivers free iodine (I2) to the bacterial cell surface.5 This results in rapid bactericidal effects by action on the cytoplasm and cytoplasmic membrane, after 1 min of skin contact.5, 6
Preoperative application of povidone-iodine to the conjunctiva and periocular skin is an effective surgical preparation technique as it is a proven method of endophthalmitis prophylaxis by reducing the number of organisms present.7, 8
As the primary source of microorganisms causing endophthalmitis is the conjunctiva,3 the effect of povidone-iodine on conjunctival bacterial contamination may have an important influence on potential prophylaxis against endophthalmitis. It was therefore the purpose of this study to assess the incidence of positive preoperative conjunctival cultures following two applications (at the time of periorbital anaesthetic block and in the theatre approximately 10 min later) in comparison with one (at the time of anaesthetic block only) application of 5% povidone-iodine solution to the operative eye.
Ultimately, this enabled a clinical outcome to be determined; whether microbial recontamination occurs after the initial application of povidone-iodine, and thus whether the second application of povidone-iodine (in the theatre) is necessary to reduce the rate of positive preoperative conjunctival cultures. In turn, clinical guidelines for preoperative preparation of the eye before cataract surgery may be established.
Materials and methods
In this prospective interventional study, all consenting patients having phacoemulsification cataract surgery at the Queen Elizabeth Hospital from 28 April to 23 May 2008 were enrolled. In addition, six patients having phacoemulsification cataract surgery at Stirling Private Hospital were enrolled, as preoperative preparation at this centre is the same as at the aforementioned hospital and surgery was performed by one of the surgeons also operating at the Queen Elizabeth Hospital. The exclusion criteria used were as follows: allergy to povidone-iodine, active ocular infection, and antibiotic therapy during the preceding 3 weeks. Nine surgeons performed the operations.
Results from 54 eyes of 54 patients were evaluated during the study period. In all, 52 of 54 patients had four specimens analysed, while two patients had three specimens analysed as a result of defective plates. One patient had a defective plate before the first application of povidone–iodine and one patient had a defective plate before the second application of povidone–iodine. All results from these two patients were subsequently excluded from the study.
At the time of the periorbital anaesthetic block (administered in preoperative room) as well as in the theatre approximately 10 min later, all patients received liberal application of povidone-iodine 5% solution via sterile swab and forceps to the conjunctival sac, lashes, and periocular skin of the operative eye. The block was administered either via skin or via conjunctiva and was administered in a clean, but not in a sterile manner.
Povidone-iodine application at the time of the periorbital anaesthetic block was of 2 min duration, and was left to dry. A conjunctival swab (for culture) was taken just before this povidone-iodine application, and again after 2 min of contact between povidone-iodine and the operative eye. This was carried out by drawing a Dacron culture swab along the inferior palpebral and bulbar conjunctiva, ensuring no contact was made with the eyelashes or skin. The contents of each swab specimen was emulsified in 1 ml of sterile normal saline from which a blood and chocolate agar plate were aseptically inoculated with 100 μl of saline suspension. Agar plates were inoculated in the theatre within 15 min of swabbing the conjunctiva. Within 3 h of inoculation, the blood agar plate was incubated anaerobically at 35 °C and the chocolate agar plate was incubated in 5% CO2 at 35 °C. All plates were incubated for 3 days.
Conjunctival swabs for culture (in an identical manner as above) were taken just before the second application of povidone-iodine (in the theatre, just before draping). Immediately after collection of these swabs, povidone-iodine was applied in the aforementioned manner, and conjunctival swabs were taken after 2 min. These swab specimens were plated within 15 min and subsequently incubated as above.
Following 3 days of incubation, each specimen was analysed by the same laboratory scientist. All plates were examined macroscopically for the presence or absence of bacterial colonies. Two plates had been incubated (one anaerobically and the other in 5% CO2) from each of the four time points at which swabs were taken (before and after both povidone-iodine applications, that is, at the time of periorbital block and in the theatre just before draping). Thus, the mean of these two colony counts (5% CO2 and anaerobic) was used to give the count at each time point. As each culture plate was inoculated with 100 μl of suspension, the number of counted colonies was multiplied by 10 to give colony-forming units per ml (CFU/ml). As a consequence of this, the limits of the quantitative results (CFU/ml) are 10 CFU/ml, with a culture-negative result being presented as <10 CFU/ml. When colonies were present, basic bacteriology identification tests such as Gram stain, catalase, oxidase, and S. aureus latex agglutination test were used to identify any bacteria present to a genus level and when possible to a species level. The data yielded were dichotomized to organism positive or organism negative and statistical analysis performed using McNemar's test for correlated proportions. Statistical analysis was performed using PASW Statistics 18 (SPSS Inc., 2009, Chicago, IL, USA).
We certify that all applicable institutional and governmental regulations concerning the ethical use of human volunteers were followed during this research.
Results
In all, 15 of 52 (29%) patients had positive cultures before the first application of povidone-iodine, and 21 of 52 (40%) had positive cultures after it (Table 1). This was not statistically significant (P=0.239). A total of 25 of 52 (48%) patients had positive cultures before the second application of povidone-iodine, which was not statistically significant when compared with 10 min earlier after the first application of povidone-iodine (P=0.423) (Table 2). Following the second application of povidone-iodine, 6 of 52 (12%) patients had positive cultures. The difference in proportion of positive results before and after the second application of povidone-iodine was statistically significant (P<0.001) (Table 3). The difference in positive cultures from before the first application of povidone-iodine compared with after the second application of povidone-iodine was statistically significant (P=0.027) (Table 4).
Table 1. Conjunctival cultures—organism positive and negative—before first application and after first application of povidone-iodine.
| Positive culture after 1st application of povidone- iodine | Negative culture after 1st application of povidone- iodine | Row total | |
|---|---|---|---|
| Positive culture before 1st application of povidone-iodine | 9 | 6 | 15 |
| Negative culture before 1st application of povidone-iodine | 12 | 25 | 37 |
| Column total | 21 | 31 | 52 |
P-value=0.239.
Table 2. Conjunctival cultures—organism positive and negative—after first application and before second application of povidone-iodine.
| Positive culture before 2nd application of povidone-iodine | Negative culture before 2nd application of povidone-iodine | Row total | |
|---|---|---|---|
| Positive culture after 1st application of povidone-iodine | 16 | 5 | 21 |
| Negative culture after 1st application of povidone-iodine | 9 | 22 | 31 |
| Column total | 25 | 27 | 52 |
P-value=0.423.
Table 3. Conjunctival cultures—organism positive and negative—before second application and after second application of povidone-iodine.
| Positive culture after 2nd application of povidone-iodine | Negative culture after 2nd application of povidone-iodine | Row total | |
|---|---|---|---|
| Positive culture before 2nd application of povidone-iodine | 4 | 21 | 25 |
| Negative culture before 2nd application of povidone-iodine | 2 | 25 | 27 |
| Column total | 6 | 46 | 52 |
P-value <0.001.
Table 4. Conjunctival cultures—organism positive and negative—before first application and after second application of povidone-iodine.
| Positive culture after 2nd application of povidone-iodine | Negative culture after 2nd application of povidone-iodine | Row total | |
|---|---|---|---|
| Positive culture before 1st application of povidone-iodine | 4 | 11 | 15 |
| Negative culture before 1st application of povidone-iodine | 2 | 35 | 37 |
| Column total | 6 | 46 | 52 |
P-value=0.027.
Catalase testing (using hydrogen peroxide) and/or coagulase testing (latex agglutination test) was used to identify streptococcal and staphylococcal species in some cases. Two specimens underwent Gram staining and microscopic examination to identify Gram-positive bacilli resembling diphtheroids. The remaining specimens were examined macroscopically only. Colonies were counted in all specimens. Coagulase-negative staphylococci were the most commonly cultured organisms (Table 5).
Table 5. Number of positive cultures (no.), percentage positive (%) and mean CFU for each organism isolated before and after each application of povidone-iodine (n=total number of eyes tested).
| Organism |
Before 1st application of povidone-iodine |
After 1st application of povidone-iodine |
Before 2nd application of povidone-iodine |
After 2nd application of povidone-iodine | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | No. | % | CFU | n | No. | % | CFU | n | No. | % | CFU | n | No. | % | CFU | |
| Coagulase-negative Staphylococci | 52 | 12 | 23 | 18 | 52 | 21 | 38 | 29 | 52 | 23 | 44 | 27 | 52 | 5 | 10 | 15 |
| S. aureus | 52 | 1 | 2 | 10 | 52 | 2 | 4 | 30 | 52 | 2 | 4 | 20 | 52 | 0 | 0 | <10 |
| Diphtheroids | 52 | 2 | 4 | 180 | 52 | 1 | 2 | 10 | 52 | 1 | 2 | 10 | 52 | 0 | 0 | <10 |
| Viridans Streptococci | 52 | 1 | 2 | 2400 | 52 | 0 | 0 | <10 | 52 | 2 | 4 | 335 | 52 | 1 | 2 | 30 |
| Pseudomonas sp. | 52 | 1 | 2 | 240 | 52 | 1 | 2 | 1690 | 52 | 1 | 2 | 4690 | 52 | 0 | 0 | <10 |
| β-Haemolytic Streptococci | 52 | 0 | 0 | <10 | 52 | 1 | 2 | 10 | 52 | 0 | 0 | <10 | 52 | 0 | 0 | <10 |
| Fungus | 52 | 0 | 0 | <10 | 52 | 0 | 0 | <10 | 52 | 1 | 2 | 10 | 52 | 0 | 0 | <10 |
Abbreviation: CFU, colony-forming units.
Discussion
A significant reduction (positive cultures in 25 of 52 eyes was reduced to 6 of 52 eyes; P<0.001) in bacterial contamination of the conjunctival surface is seen only after double application of povidone-iodine. The first application failed to cause any significant reduction.
Endophthalmitis is usually caused by exogenous infection, which in up to 60% of cases results from direct inoculation as a complication of intraocular surgery.9 Despite this, endophthalmitis is a rare complication of intraocular surgery, with an estimated incidence of 0.07–0.13% following cataract surgery.3 A 10-year retrospective study of acute-onset (within 6 weeks of intraocular surgery) endophthalmitis at one institution elicited an overall incidence of 0.093% following intraocular surgical procedures.10 Povidone-iodine is cheap, has a broad spectrum of microbicidal effects, and has either no or negligible toxicity.11 Probably for these reasons, it has previously been evaluated as a component of preoperative preparation of the eye before cataract surgery. However, based on the nature of preoperative preparation, recontamination of the eye is possible. This study evaluates the importance of double application of povidone-iodine.
S. epidermidis, S. aureus, and Streptococcus species are the organisms most frequently cultured, although Gram-negative bacilli (for example, Serratia spp., Proteus spp., and Pseudomonas spp.) are also culprits.1 Propionibacterium acnes and fungi can also cause acute-onset infections; however, they more frequently cause delayed-onset endophthalmitis.1 The primary source of microorganisms causing postoperative bacterial endophthalmitis appears to be the eyelid margin and in turn the conjunctiva.3
A prospective study of the incidence of bacterial contamination of the anterior chamber after phacoemulsification cataract surgery utilized two applications of povidone-iodine (10%) preoperatively. The reduction in bacterial load (postoperatively compared to preoperatively) was significant (P<0.001).3
In a study of 30 patients undergoing ophthalmic surgery, there was a statistically significant decrease in the number of colonies and species in eyes receiving povidone-iodine (P-values of <0.05 and <0.01 for colonies and species, respectively), contrary to untreated eyes (not statistically significant).7
A systematic literature review of prophylactic methods against bacterial endophthalmitis by Ciulla, Starr, and Masket gave different interventions an evidence rating (based on 88 peer-reviewed papers from 1966 to 2000) and hence a clinical recommendation. This review focused on assessment of the effect of prophylactic interventions on endophthalmitis incidence rather than on intraocular or surface flora.12 Preoperative povidone-iodine was considered moderately important to clinical outcome (level B clinical rating).12 All other prophylactic methods (postoperative subconjunctival antibiotics, preoperative lash trimming, preoperative saline irrigation, preoperative topical antibiotics, antibiotic irrigation, and intraoperative heparin) were considered not to be definitely related to clinical outcome (level C clinical rating).12 The review concluded that preoperative conjunctival application of povidone-iodine significantly reduces the relative risk of postoperative endophthalmitis.12, 13
A multicentre study of endophthalmitis prophylaxis by the European Society of Cataract and Refractive Surgeons prospectively evaluated the prophylactic effect of intracameral cefuroxime injection at the time of phacoemulsification cataract surgery. The study of 13 698 patients was terminated early and unmasked because the beneficial effect of cefuroxime was notably significant.14 Intracameral cefuroxime significantly reduced the total risk of endophthalmitis, as well as proven infective endophthalmitis (P-values of 0.002 and 0.008, respectively).14 The effect of intracameral antibiotics was not assessed in this study.
In an open-label non-randomized parallel trial, Speaker and Menikoff15 concluded that povidone-iodine has efficacy in decreasing the incidence of postoperative endophthalmitis. This was compared with a silver protein solution when administered in different operating suites.15 Furthermore, a reduction in the incidence of culture-positive endophthalmitis in one suite following the introduction of povidone-iodine was also demonstrated.15
A retrospective study of 19 269 cataract extractions with lens implantation yielded a reduction in the incidence of culture-positive endophthalmitis following the introduction of povidone-iodine.8 The incidence was 0.08% of 4740 cases without povidone-iodine, and 0.03% of 14 529 cases with povidone-iodine.8
This prospective observational study demonstrates that a high number of patients (15 of 52 patients or 29%) had positive cultures before the first application of povidone-iodine and that the initial application of povidone-iodine was not effective in reducing this. There was an increase in the proportion of patients who were culture positive from before the peribulbar block to immediately after completion of the peribulbar block (21 of 52 patients or 40%). This apparent increase was not statistically significant, implying that the increased numbers of contaminated eyes represent persistence of contamination not recontamination. However, recontamination was possible as a result of a non-sterile environment. For many ophthalmology procedures, the anaesthetic block is not given in a sterile, laminar flow theatre. There was no statistically significant recontamination following this; however, a notable proportion of patients (25 of 52 patients or 48%) remained culture positive before the second application of povidone-iodine in the theatre. After the second application of povidone-iodine, only six patients (12%) were culture positive. In comparison with positive conjunctival cultures just before the second application of povidone-iodine, this was statistically significant (P<0.001). This highlights that double application of povidone-iodine reduced the incidence of positive conjunctival cultures and thus the potential for endophthalmitis following cataract surgery.
There are a number of weaknesses in this study that should be recognized. Nine different ophthalmologists performed the procedures resulting in subtle differences in preoperative procedure: some ophthalmologists administered the peribulbar anaesthetic block within the conjunctiva, while some injected through the skin external to the conjunctiva. Variable anatomy may also have led to sampling differences. Ultimately, how much povidone-iodine reaches the conjunctival sac may vary.
In one patient, the periorbital anaesthetic block was administered in the theatre rather than in the preoperative room, resulting in a shorter time between samples as well as the potential for less contamination. In another patient, the second sample was taken 45 min after the periorbital anaesthetic block owing to the presence of a retrobulbar haematoma. Again there may have been an augmented likelihood of contamination before the next sample.
We conclude that the initial application of povidone-iodine was not effective and that recontamination did not take place between applications. The difference in proportion with positive results before and after the second application of povidone-iodine was statistically significant in this observational study. We infer from this that double application of povidone-iodine before cataract surgery is advisable.
Acknowledgments
We thank Dr Neil Gehling for technical support. This study was supported by funding from the Department of Ophthalmology at The Queen Elizabeth Hospital, Woodville South, South Australia, Australia.
The authors declare no conflict of interest.
Footnotes
The abstract was presented as a ‘Rapid Fire' presentation at the 40th Annual Scientific Congress of the Royal Australian and New Zealand College of Ophthalmologists on Monday 24 November 2008.
References
- Kresloff MS, Castellarin AA, Zarbin MA. Endophthalmitis. Surv Ophthal. 1998;43 (3:193–224. doi: 10.1016/s0039-6257(98)00036-8. [DOI] [PubMed] [Google Scholar]
- Brooks GF, Butel JS, Morse SA.Jawetz, Melnick, and Adelberg's Medical Microbiology22nd edn.McGraw-Hill: New York; 2001176–179. [Google Scholar]
- Leong JK, Shah R, McCluskey PJ, Benn RA, Taylor RF. Bacterial contamination of the anterior chamber during phacoemulsification cataract surgery. J Cataract Refract Surg. 2002;28:826–833. doi: 10.1016/s0886-3350(01)01160-9. [DOI] [PubMed] [Google Scholar]
- Reimer K, Wichelhaus TA, Schafer V, Rudolph P, Kramer A, Wutzler P, et al. Antimicrobial effectiveness of povidone-iodine and consequences for new application areas. Dermatology. 2002;204 (Suppl 1:114–120. doi: 10.1159/000057738. [DOI] [PubMed] [Google Scholar]
- Zamora JL. Chemical and microbiologic characteristics and toxicity of povidone-iodine solutions. Am J Surg. 1986;151:400–406. doi: 10.1016/0002-9610(86)90477-0. [DOI] [PubMed] [Google Scholar]
- Saggers BA, Stewart GT. Polyvinyl-pyrrolidone-iodine: an assessment of antibacterial activity. J Hyg. 1964;62:509–518. doi: 10.1017/s0022172400040225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Apt L, Isenberg S, Yoshimori R, Paez JH. Chemical preparation of the eye in ophthalmic surgery: III. Effect of povidone-iodine on the conjunctiva. Arch Ophthalmol. 1984;102:728–729. doi: 10.1001/archopht.1984.01040030584025. [DOI] [PubMed] [Google Scholar]
- Bohigian GM. A study of the incidence of culture-positive endophthalmitis after cataract surgery in an ambulatory care center. Ophthalmic Surg Lasers. 1999;30 (4:295–298. [PubMed] [Google Scholar]
- Peters JR, Egan DJ, Peak DA.EndophthalmitisAvailable from URL: http://www.emedicine.com/emerg/topic880.htm . (11 July 2006).
- Aaberg TM, Jr, Flynn HW, Jr, Schiffman J, Newton J. Nosocomial acute-onset postoperative endophthalmitis survey. Ophthalmology. 1998;105:1004–1010. doi: 10.1016/S0161-6420(98)96000-6. [DOI] [PubMed] [Google Scholar]
- de Kaspar HM, Chang RT, Singh K, Egbert PR, Blumenkranz MS, Ta CN. Prospective randomized comparison of 2 different methods of 5% povidone-iodine applications for anterior segment intraocular surgery. Arch Ophthalmol. 2005;123:161–165. doi: 10.1001/archopht.123.2.161. [DOI] [PubMed] [Google Scholar]
- Ciulla TA, Starr MB, Masket S. Bacterial endophthalmitis prophylaxis for cataract surgery: an evidence-based update. Ophthalmology. 2002;109 (1:13–24. doi: 10.1016/s0161-6420(01)00899-5. [DOI] [PubMed] [Google Scholar]
- Schmitz S, Dick HB, Krummenauer F, Pfeiffer N. Endophthalmitis in cataract surgery: results of a German survey. Ophthalmology. 1999;106 (10:1869–1877. doi: 10.1016/S0161-6420(99)90395-0. [DOI] [PubMed] [Google Scholar]
- Barry P, Seal DV, Gettinby G, Lees F, Peterson M, Revie CW. ESCRS study of prophylaxis of postoperative endophthalmitis after cataract surgery. J Cataract Refract Surg. 2006;32:407–410. doi: 10.1016/j.jcrs.2006.02.021. [DOI] [PubMed] [Google Scholar]
- Speaker MG, Menikoff JA. Prophylaxis of endophthalmitis with topical povidone-iodine. Ophthalmology. 1991;98:1769–1775. doi: 10.1016/s0161-6420(91)32052-9. [DOI] [PubMed] [Google Scholar]


