Abstract
Purpose
To compare demographics, severity, and activity of thyroid eye disease (TED) in patients with hyperthyroidism (Hr-TED) vs primary hypothyroidism (Ho-TED).
Patients and Methods
In a cross-sectional study, demographics, complete eye examination, severity score (NOSPECS, total hundred eye score), clinical activity score, and Rundle grading were recorded for patients with TED and different thyroid disorders referred from an endocrinology clinic from 2003 to 2006.
Results
TED was clinically found in 303 patients (303/851, 35.6%). The majority of them (280/303, 92.4%) had Graves' hyperthyroidism and 23 (23/303, 7.5%) had primary hypothyroidism. Mean age, gender, mean severity score, mean activity score, Rundle grade, unilateral presentation of TED, smoking habit, mean duration of eye disease, and mean interval time of thyroid to TED were not significantly different between the two groups (0.06<P<0.9). Mean duration of thyroid disease was significantly (P=0.02) longer in the Hr-TED group (49.6 months) than in the Ho-TED group (22.7 months). Most of the patients in both groups (63.2% of Hr-TED and 73.9% of Ho-TED) developed the eye disease within 18 months before or after the thyroid disease.
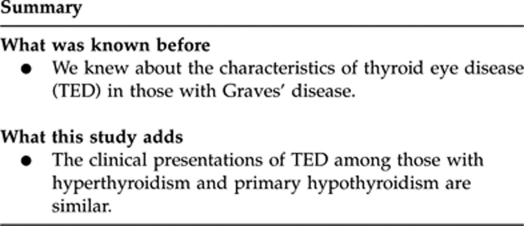
Conclusion
The same demographics, clinical characteristics, and severity and activity scores for Hr-TED and Ho-TED imply that both groups present the same category of eye disease.
Keywords: thyroid eye disease, Graves' ophthalmopathy, orbitopathy, hypothyroidism, hyperthyroidism
Introduction
Thyroid eye disease (TED), also known as Graves' orbitopathy or dysthyroid ophthalmopathy, is an autoimmune infiltrative and inflammatory disorder with numerous characteristic clinical signs and multiple clinical expressions, which reflects uncertainties about its pathogenesis, and that the underlying cause continues to be discovered.1 Patients with TED frequently experience disfigurement and functional disability, including pain, proptosis, eyelid swelling, diplopia, conjunctival chemosis, corneal exposure, and optic neuropathy.2, 3, 4, 5, 6, 7, 8, 9, 10, 11, 12, 13, 14, 15, 16, 17, 18, 19, 20, 21, 22, 23, 24, 25, 26, 27, 28, 29, 30, 31, 32, 33, 34, 35, 36
Clinically significant ophthalmopathy is common and occurs in 50% of hyperthyroid patients (Hr-TED); it reaches up to 90% if a computerized tomography is performed.6 However, most have mild disease with local eye symptoms.
Although, patients with primary hypothyroidism less commonly develop TED (Ho-TED), it is being recognized more as the awareness and diagnostic techniques have improved.8 Ho-TED has been reported with a frequency of 0.2 to 8.6% of patients with TED.1, 4, 9, 10, 26, 27
Whether the clinical manifestations of Hr-TED patients differ from those of Ho-TED patients is not clearly elucidated in the literature. Although Eckstein et al3 compared Ho-TED with Hr-TED and concluded that the former group develops significantly less severe form of TED, others11, 12, 13, 14 reported the same severity as Hr-TED.
We conducted a cross-sectional study on the characteristics of all patients with thyroid disease in our population.2, 15 The aim of this study was to compare demographics and clinical manifestations, especially severity and activity scores, of patients with Hr-TED with Ho-TED. To the best of our knowledge, there was only one recent study2 that systematically compared the clinical characteristics of Hr-TED with Ho-TED. This study is the largest series of such a comparison.
Patients and methods
All patients with different thyroid disorders visited in a referral endocrinology clinic (university hospital) were included from September 2003 to July 2006. Two general practitioners were initially trained to screen the thyroid-disordered patients with regard to any signs and/or symptoms of TED. A special data sheet was completed for each patient. Patients with any symptom and/or sign of a TED were referred to a TED clinic (Rassoul Akram Hospital) for further evaluation.
Diagnosis of thyroid dysfunction16 was based on clinical examination and hormone level and in some cases thyroid gland scan and sonography. Antibody titers were not used for the definition of thyroid gland disease as hypo- vs hyperthyroid. They were checked (when available) to assess the autoimmunity in the setting of thyroid disease. Antibody tests were not available in the beginning but anti-thyroid peroxidase antibody was checked since 2005.
Diagnosis of TED was clinical and made on the basis of thyroid disorder associated with one of the following signs: eyelid retraction and/or lag, proptosis, restrictive myopathy, dysthyroid optic neuropathy, fluctuating eyelid edema and/or erythema, conjunctival chemosis and/or diffuse redness, and caruncular edema. Orbital imaging was requested for all cases with unilateral TED to look for other orbital pathologies and selected bilateral TED to mainly look for the signs of optic neuropathy. Findings on imaging, however, were not considered for the diagnosis of TED. Unilateral TED was considered when there was a clinical diagnosis of TED in one eye but no clinical sign on the other eye. A special TED form was completed for each subject, which included different sections regarding thyroid gland disorder; associated systemic diseases including autoimmune diseases (systemic lupus erythematosus and rheumatoid arthritis), diabetes mellitus, myasthenia gravis, and cardiovascular diseases; history of medications; eye symptoms at presentation of TED; visual function tests including best corrected visual acuity, color vision, and visual field; optic disc; intraocular pressure (IOP) in primary and up-gaze; Hertel exophthalmometry; eyelid examination; ocular motility examination; slit lamp examination; and findings on orbital imaging. The examination ended up recording Mourits' clinical activity score18, NOSPECS19 (total eye score of severity), and Rundle20 categorization of TED.
NOSPECS stands for no TED sign (N), only eyelid sign (O), soft tissue involvement (S), proptosis (P), extraocular motility restriction (E), corneal involvement (C), and sight loss (S). The NOSPECS severity score has six classes (N=0, O=1, S=2, P=3, E=4, C=5, and S=6) and four grades with increasing severity (0, 1, 2, and 3) for each class. This was used to calculate total eye score (TES), which ranged from 0 to 63 (the higher the score, the worse the severity). The score of each class was equal to the number of class multiplying by the number of grade at each class; TES was sum of all the scores in the six classes.
Patients with TED were finally categorized on the basis of Rundle classification in order to ease the classification of different TED status as Rundle A: lid edema/erythema, chemosis, or caruncular edema; Rundle B: eyelid retraction or proptosis±Rundle A; Rundle C: restrictive myopathy±Rundle A and/or B; and Rundle D: optic neuropathy±Rundle A, B, and/or C.
In case of asymmetric severity and/or activity scores, worse eye scores were considered for the management and analysis. Open angle glaucoma (OAG) was defined as more than 21 mm Hg IOPs in primary gaze associated with glaucomatous optic disc and/or visual field defects as diagnosed by a glaucoma subspecialist. The research protocol was approved by Tehran University Eye Research Center Ethics Committee. All patients gave written informed consent.
Data were entered and analyzed with software SPSS (version 16, Chicago, IL, USA). Independent sample t-test was used for comparing the means between the two groups, and χ2-test was used to compare the non-parametric variables in the two groups.
Results
There were 851 patients with hyperthyroidism and primary hypothyroidism. TED was clinically found in 303 patients (303/851, 35.6%). The majority of them (280/303, 92.4%) had Graves' hyperthyroidism and 23 (23/303, 7.5%) had primary hypothyroidism. Mean age was 37.06±14.53 (range: 9–80) years. There were 201 (201/303, 66.3%) women.
Mean age in Hr-TED was 37.13 (SD=14.6) years and in Ho-TED was 36.6 (SD=14.2; P=0.81) years. Male/female ratio was 1:1.85 in the Hr-TED and 1:2.8 in Ho-TED group (P=0.38). Among patients with Hr-TED, 15.3% (42/274) had associated systemic diseases, including cardiovascular disease (29), autoimmune diseases (9), diabetes mellitus (8), and myasthenia gravis (1). There were one patient with systemic lupus erythematosus and one with cardiovascular disease in the Ho-TED group (2/23, 8.6%). OAG was found in just one patient with Ho-TED (1/23, 4.3%) and 17 (17/274, 6%) with Hr-TED (P=0.8). Mean duration of thyroid disease was significantly (P=0.02) longer in the Hr-TED group (49.6 months) than in the Ho-TED group (22.7 months). However, mean time interval from thyroid disease to the eye disease was not significantly different (Table 1). Most of the patients in both groups developed the eye disease within 18 months before and after the thyroid disease (Table 1).
Table 1. Statistical analysis of different variables in 303 patients with TED; 23 with Ho-TED; and 280 with Hr-TED.
| Hr-TED | Ho-TED | P-value | |
|---|---|---|---|
| Age group (years) | |||
| ≤35 | 132 (47.1%) | 11 (47.8%) | 0.5 |
| >35 | 148 (52.8%) | 12 (52.1%) | |
| Gender | |||
| Female | 183 (65.3%) | 18 (78.2%) | 0.3 |
| Male | 97 (34.7%) | 5 (21.8%) | |
| Duration of treated thyroid disease in months (SD) | 49.6 (68) | 22.7 (26.7) | 0.02 |
| Duration of eye disease in months (SD) | 21 (47.1) | 11.6 (16.9) | 0.1 |
| Mean time interval from thyroid disease to TED (SD) | 28.5 (53.6) | 11 (22.9) | 0.1 |
| Number of TED patients presented before and or after thyroid disease | |||
| More than 18 months before thyroid disease | 2 (0.7%) | 0 (0) | 0.5 |
| 18 months before or after thyroid disease | 177 (63.2%) | 17 (73.9%) | |
| More than 18 months after thyroid disease | 101 (36%) | 6 (26.1%) | |
| Positive family history of thyroid disease | 156 (55.7%) | 17 (73.9%) | 0.06 |
| Smoker | |||
| No | 169 (60.3%) | 14 (60.8%) | 0.3 |
| Active | 53 (18.9%) | 2 (8.6%) | |
| Passive | 58 (20.7%) | 7 (30.4%) | |
| Open angle glaucoma | 17 (6%) | 1 (4.3%) | 0.5 |
| Laterality | |||
| Bilateral | 250 (89.2%) | 21 (91.3%) | 0.5 |
| Unilateral | 30 (10.7%) | 2 (8.6%) | |
| Rundle's grade | |||
| A | 57 (20.3%) | 6 (26.1%) | 0.5 |
| B | 152 (54.2%) | 14 (60.8%) | |
| C | 54 (19.2%) | 2 (8.6%) | |
| D | 17 (6%) | 1 (4.3%) | |
| Mean hundred total eye score (SD) | 6.8 (5.9) | 5.5 (7.1) | 0.3 |
| Mean clinical activity score (SD) | 1.6 (1.5) | 1.4 (1.5) | 0.5 |
| Active state of TED | 66 (22.7%) | 5 (21.7%) | 0.5 |
Abbreviations: Ho-TED, hypothyroid eye disease; Hr-TED, hyperthyroid eye disease; TED, thyroid eye disease.
Gender, family history (first and second degrees) of thyroid disorders, age group, laterality, duration of TED, and smoking habit were not significantly different between the two groups (Table 1). Activity and severity of TED and Rundle classification also did not show any significant difference between Hr- vs Ho-TED (Table 1).
Discussion
Ho-TED was first reported by Wyse et al21 in 1968. Since then other reports3, 4, 8, 9, 10, 11, 12, 13, 22, 23, 24 on Ho-TED modified the concept of hyperthyroidism being an essential component of TED. Different explanations have been proposed on occurrence of Ho-TED. One was that hyperthyroidism and hypothyroidism might occur in one patient, but at different times, because of the possibility of spontaneous transition.22 Change of blocking antibodies into stimulating antibodies would be another explanation.22 Starrenburg-Razenberg et al11 hypothesized that different concentrations of blocking and stimulating antibodies attack the thyroid cell simultaneously, which might cause hypothyroidism or hyperthyroidism. Christy and More8 suggested that the pathogenesis of Ho-TED is similar to that of euthyroid TED, the difference being one of more extensive intrinsic thyroid cell abnormality in the former than in the latter. In spite of several reports on Ho-TED in the last 50 years, this disease is not very well known in the textbooks, which might have led to an underestimation.11 We did a cross-sectional study on all the patients with thyroid disorders and found that 7.5% of our series of patients with TED had hypothyroidism as background thyroid disease. Some have reported the hypothyroid and euthyroid TED together in up to 20% of patient with TED.25 However, hypothyroidism as primary thyroid dysfunction associated with TED was reported from 0.2 to 8.6% of patients with TED, most of them had autoimmune type of hypothyroidism (Hashimoto's thyroiditis).1, 3, 4, 9, 10, 26, 27 Although autoantibodies were not checked for all the patients because of unavailability, our endocrinologists believed that Hashimoto's thyroiditis was the main cause of hypothyroidism in this series. Our result of 7.5% Ho-TED is more than what has previously been reported. This may be because of the resource of this study population (a tertiary referral endocrinology center), a wider definition of TED in this study, some unknown genetic differences, or environmental changes in this population.
The present study showed no significant difference between Ho-TED and Hr-TED regarding the activity and severity of TED. Eckstein et al3 compared 143 Hr-TED, 28 euthyroid TED, and 11 Ho-TED and concluded that Ho-TED and euthyroid TED were similar and developed significantly less severe and less active TED than Hr-TED. However, severe TED and dysthyroid optic neuropathy have been observed in patients with hypothyroidism.11, 12, 13, 26 It has been reported that that euthyroid TED and Ho-TED develop more asymmetric TED than Hr-TED.3 Unilateral TED was found in 10.7% of Hr-TED and 8.6% of Ho-TED (P=0.5). We recently showed that there is no significant difference between unilateral vs bilateral TED regarding the demographics, type of thyroid disease, associated findings, and severity and activity of TED.15 Our data indicated that patients with U-TED belonged to the same population as those with bilateral eye disease.15
Similar to Eckstein et al,3 we found no significant difference with regard to the age, gender, and smoking habit between Hr-TED vs Ho-TED (Table 1). Manji et al28 have also stated that the presence of ophthalmopathy in both hyperthyroid and hypothyroid patients (Hashimoto thyroiditis) was not independently associated with gender. The mean age of presentation in our study was 37.06 years, which is lower than other studies.29, 30, 31 This may reflect the generally younger population of the region of this study or ethnic difference.
OAG in 5.9% (18/303) of TED in this study was comparable to the previously published reports on the link between TED and glaucoma. Prevalence of OAG in patients with TED varied from 0.8 to 13.5% in different studies.32, 33, 34, 35 Genetic dissimilarity and different stages of TED in these studies may be attributed to different prevalence of OAG in patients with TED.
Similar to others,28 we found a positive family history of different thyroid disorders in 55.7% of Hr-TED and 73.9% of Ho-TED, implying an underlying genetic predisposition in both groups. Genetic predisposition is a major etiological factor in the development of Graves' ophthalmopathy.36 It is likely that genetic predisposition is necessary for the development of Hr-TED and that environmental factors possibly control whether a genetically predisposed subject progresses to a clinically overt disease.36
In conclusion, this is the largest study of comparing Hr-TED with Ho-TED. We found the same demographics, clinical characteristics, and severity and activity scores for Hr-TED and Ho-TED, implying that both groups present the same category of eye disease.
Limitations of this study are unavailability of antibody tests (unable to differentiate Hashimoto's thyroiditis from other primary hypothyroidism), low number of patients in the Ho-TED group for analysis (low power to draw a definite conclusion), self-reported nature of duration of diseases and family history, and design of cross-sectional study (neglecting transition between different thyroid disorders in time). A multicentre cohort study with a larger sample size would clarify differences and similarities between Hr-TED vs Ho-TED.
The authors declare no conflict of interest.
Footnotes
This study was financially supported by Eye Research Center, Rassoul Akram Hospital, Tehran University of Medical Sciences, Tehran, Iran.
This study was presented in the annual meeting of European Society of Ophthalmic Plastic and Reconstructive Surgery, Munich, September 2010.
References
- Marcocci C, Bartalena L, Bogazzi F, Panicucci M, Pinchera A. Studies on the occurrence of ophthalmopathy in Graves' disease. Acta Endocrinol. 1989;120:473–478. doi: 10.1530/acta.0.1200473. [DOI] [PubMed] [Google Scholar]
- Kashkouli MB, Heidari I, Pakdel F, Jam S, Honarbakhsh Y, Mirarmandehi B. Change in quality of life after medical and surgical treatment of Graves' ophthalmopathy. Middle East Afr J Ophthalmol. 2011;18:42–48. doi: 10.4103/0974-9233.75884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eckstein A, Loesch C, Glowacka D, Schott M, Mann K, Esser J, et al. Eythyroid and primarily hypothyroid patients develop milder and significantly more asymmetric Graves' ophthalmopathy. Br J Ophthalmol. 2009;93:1052. doi: 10.1136/bjo.2007.137265. [DOI] [PubMed] [Google Scholar]
- Khoo DH, Eng PH, Ho SC, Tai ES, Morgenthaler NG, Seah LL, et al. Graves' ophthalmopathy in the absence of elevated free thyroxin and triidothyronine levels: prevalence, natural history and thyrotropin receptor antibody levels. Thyroid. 2000;10:1093–1100. doi: 10.1089/thy.2000.10.1093. [DOI] [PubMed] [Google Scholar]
- Wiersinga WM, Smit T, Vander Gaag R, Koornneef L. Temporal relationship between onset of Graves' ophthalmopathy and onset of thyroid Graves' disease. J Endocrinal Invest. 1988;11:615–619. doi: 10.1007/BF03350193. [DOI] [PubMed] [Google Scholar]
- Jameson Jl, Weetman AP.Disorders of the thyroid glandIn: Fauci, Braunwald et al (eds).Harrisons' Principle of Internal Medicine17th ed. Mc Graw-Hill: New York; 200823–32. [Google Scholar]
- Dolman PJ, Rootman J. VISA classification for Graves orbitopathy. Ophthalmic Plast Reconstr Surg. 2006;22:319–324. doi: 10.1097/01.iop.0000235499.34867.85. [DOI] [PubMed] [Google Scholar]
- Chirsty JH, Morse RS. Hypothyroid Graves' disease. AM J Med. 1977;62:291–296. doi: 10.1016/0002-9343(77)90325-4. [DOI] [PubMed] [Google Scholar]
- Bartley GB, Fatourechi V, Kadrmas EF, Jacobsen SJ, Ilstrup DM, Garrity JA, et al. Clinical features of Graves' ophthamopathy in an incidence cohort. Am J Ophthalmol. 1996;121:284–290. doi: 10.1016/s0002-9394(14)70276-4. [DOI] [PubMed] [Google Scholar]
- Prummel MF, Barker A, Wiersinga WM. Multicenter study on the characteristics and treatment strategies of patients with Graves' ophthalmopathy: the first European Group on Graves' ophthalmopathy experience. Eur J Endocrinol. 2003;148:491–495. doi: 10.1530/eje.0.1480491. [DOI] [PubMed] [Google Scholar]
- Starrenburg AJ, Cabezas M, Gan IM, Njo TL, Rietveld AP, Elte JW. Four patients with hypothyroid Graves' disease. Neth J Med. 2010;68 4:178–180. [PubMed] [Google Scholar]
- Campos-Pavon J, Mencia-Guitierrez E, Gutierrez-Diaz E. Malignant exophthalmos in hyperthyroidism with a hypothyroid crisis. Arch Soc Esp Oftalmol. 2006;81:721–724. doi: 10.4321/s0365-66912006001200010. [DOI] [PubMed] [Google Scholar]
- Macia-Bobes C, Ronzon-Fernandez A. Dysthyroid ophthalmopathy associated hypothyroidism. Arch Soc Esp Oftalmol. 2007;82:765–767. doi: 10.4321/s0365-66912007001200010. [DOI] [PubMed] [Google Scholar]
- Brownlie BE, Newton OA, Singh SP. Ophthalmopathy associated with primary hypothyroidism. Acta Endocrinol (Copenh) 1975;79:691–699. doi: 10.1530/acta.0.0790691. [DOI] [PubMed] [Google Scholar]
- Kashkouli MB, Kaghazkanani R, Heidari I, Ketabi N, Jam S, Azarnia SH, et al. Bilateral versus unilateral thyroid eye disease Indian J Ophthalmol 2011. in press). [DOI] [PMC free article] [PubMed]
- Baskin HJ, Cobin RH, Duick DS, Gharib H, Guttler RB, Kaplan MM, et al. American association of clinical endocrinologists medical guidelines for clinical practice for the evaluation and treatment of hyperthyroidism and hypothyroidism. Endocr Pract. 2002;8:457–469. [PubMed] [Google Scholar]
- Gorman CA. Temporal relationship between onset of Graves' ophthalmopathy and diagnosis of thyrotoxicosis. Mayo Clin Proc. 1983;58:515–519. [PubMed] [Google Scholar]
- Mourits MP, Koornneef L, Wiersinga WM, Prummel MF, Berghout A, van der Gaag R. Clinical criteria for assessment of disease activity in Graves' ophthalmopathy: a novel approach. Br J Ophthalmol. 1989;73 (8:639–644. doi: 10.1136/bjo.73.8.639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Werner SC. Modification of the classification of the eye changes of Graves' disease: recommendations of the Ad Hoc Committee of the American Thyroid association. J Clin Endocrinol Metab. 1977;44:203–204. doi: 10.1210/jcem-44-1-203. [DOI] [PubMed] [Google Scholar]
- Rundle FF. Management of exophthalmos and related ocular changes in Graves' disease. Metabolism. 1957;6:36–48. [PubMed] [Google Scholar]
- Wyse EP, McConahey WM, Woolner LB, Scholtz DA, Kearns TP. Ophthalmopathy without hyperthyroidism in patients with histologic Hashimoto's thyroiditis. J Clin Endocrinol Metab. 1968;28:1623–1629. doi: 10.1210/jcem-28-11-1623. [DOI] [PubMed] [Google Scholar]
- McDermott MT, Kidd GS, Dodson LE, Hofeldt FD. Case report: hyperthyroidism following hypothyroidism. Am J Med Sci. 1986;291:194–198. doi: 10.1097/00000441-198603000-00011. [DOI] [PubMed] [Google Scholar]
- Taylor T, Czarnowski C. Asymmetric ophthalmopathy in a hypothyroid patient. Can Fam Physician. 2007;53:635–638. [PMC free article] [PubMed] [Google Scholar]
- Cronin CC, Higgins TM, Murphy D, Ferriss JB. Concomitant Graves' disease and Hashimoto's thyroiditis, presenting as primary hypothyroidism. Ir Med J. 1996;89:141–142. [PubMed] [Google Scholar]
- Clauser L, Galie M, Sarti E, Dallera V. Rationale of treatment in Graves' ophthalmopathy. Plast Reconstr Surg. 2001;108:1880–1894. doi: 10.1097/00006534-200112000-00006. [DOI] [PubMed] [Google Scholar]
- Rajput R, Dhingra A, Kumar K, Sen J. Infiltrative ophthalmopathy and hypothyroidism: a rare clinical manifestation of a common disease. Postgrad Med J. 2009;85:40–42. doi: 10.1136/pgmj.2008.071704. [DOI] [PubMed] [Google Scholar]
- Tari AS, Rajabi MT, Hamzedust K, Tabatabaie SZ. Clinical features of Graves' ophthalmopathy in Iran. Int J Ophthalmol. 2007;7:322–326. [Google Scholar]
- Manji J D, Carr-Smith K, Boelaert A, Allahabadia M, Armitage VK, Chatterjee JH., et al., Pearce B. Phenotype influences of age, gender, smoking, and family history on autoimmune thyroid disease. J Clin Endocrinol Metab. 2006;91:4873–4880. doi: 10.1210/jc.2006-1402. [DOI] [PubMed] [Google Scholar]
- Wiersinga WM, Smit T, Van der Graag R, Mourits M, Korneef L. Clinical presentation of Graves' ophthalmopathy. Ophthalmic Res. 1989;21:73–82. doi: 10.1159/000266782. [DOI] [PubMed] [Google Scholar]
- Bartley GB. The epidemiologic characteristics and clinical course of ophthalmopathy associated with autoimmune thyroid disease in Olmsted County, Minnesota. Trans Am Ophthalmol Soc. 1994;92:477–588. [PMC free article] [PubMed] [Google Scholar]
- Kendler DL, Lippa J, Rootman J. The initial clinical characteristics of Graves' orbitopathy vary with age and sex. Arch Ophthalmol. 1993;111:197–201. doi: 10.1001/archopht.1993.01090020051022. [DOI] [PubMed] [Google Scholar]
- Behrouzi Z, Rabei HM, Azizi F, Daftarian N, Mehrabi Y, Ardeshiri M, et al. Prevalence of open-angle glaucoma, glaucoma suspect and ocular hypertension in thyroid-related immune orbitopathy. J Glaucoma. 2007;163:58–62. doi: 10.1097/IJG.0b013e31802e644b. [DOI] [PubMed] [Google Scholar]
- Cockerham KP, Pal C, Jani P, Wolter A, Kennerdell JS. The prevalence and implications of ocular hypertension and glaucoma in thyroid-associated orbitopathy. Ophthalmology. 1997;104:914–917. doi: 10.1016/s0161-6420(97)30207-3. [DOI] [PubMed] [Google Scholar]
- Otsuka K, Nakamura Y. Open-angle glaucoma associated with Grave's disease. Am J Ophthalmol. 2000;129:613–617. doi: 10.1016/s0002-9394(99)00473-0. [DOI] [PubMed] [Google Scholar]
- Kalmann R, Mourits MP. Prevalence and management of elevated intraocular pressure in patients with Grave's orbitopathy. Br J Ophthalmol. 1998;82:745–757. doi: 10.1136/bjo.82.7.754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brix TH, Kyvik KO, Christensen K, Hegedus L. Evidence for a major role of heredity in Graves' disease: a population-based study of two Danish twin cohorts. J Clin Endocrinol Metab. 2001;86:930–934. doi: 10.1210/jcem.86.2.7242. [DOI] [PubMed] [Google Scholar]


