Abstract
Background:
HIV/AIDS pandemic is responsible for the resurgence of TB worldwide, resulting in increased morbidity and mortality. HIV and Mycobacterium tuberculosis have a synergistic interaction; each propagates progression of the other. Coinfection with HIV infection leads to difficulties in both the diagnosis and treatment of tuberculosis, increase risk of death, treatment failure and relapse.
Objective:
The aim of the present study is to study the clinical, radiological profile of pulmonary and extrapulmonary tuberculosis (EPTB) in HIV-seropositive patients and their relationship to CD4 counts.
Materials and Methods:
It was a prospective study conducted over a period of 1 year in the department of medicine, Indira Gandhi Medical College, Shimla. We examined 87 HIV-infected patients with associated tuberculosis recruited from the department of medicine and antiretroviral center and were subjected to thorough clinical examination, X-ray chest, tuberculin testing and sputum examination for AFB and necessary relevant investigations for EPTB.
Results:
Most common affected age group was 31-40 years. EPTB is the commonest form of TB in our study detected in 65 patients. Commonest EPTB was CNS tuberculosis. Disseminated tuberculosis was only found in patient with CD4 count less than 200/cmm. Majority of lymph node TB was diagnosed by fine needle aspiration cytology (FNAC) examination. All patients with AFB-positive lymph node had CD4 count below 200/cum.
Conclusions:
The results of this study provide information regarding the various forms of TB and their presentation in HIV-infected persons. Early diagnosis of tuberculosis and prompt institution of antitubercular treatment (ATT) reduces mortality and morbidity significantly. In resource-poor areas, the diagnosis can be established with cytological/biochemical analysis of fluid, histopathological examination and ZN staining of tissue coupled with radiological features and response to ATT. Therefore, adequate knowledge of the manifestations of tuberculosis in HIV-infected patients is absolutely necessary for optimal management and to reduce mortality and morbidity.
KEY WORDS: AFB smear, CD4 count, extrapulmonary, HIV, pulmonary, tuberculosis
INTRODUCTION
Tuberculosis is the most common human immunodeficiency (HIV) virus-related opportunistic infection in India and caring for patients with both diseases is a major public health challenge. It is estimated that 60-70% of HIV-positive persons will develop tuberculosis in their lifetime.[1] Approximately, 50% of adult Indian population is infected with Mycobacterium tuberculosis, and the spread of HIV infection could lead to a potentially explosive increase in the number of cases of tuberculosis.[1] About 1.8 million new cases of tuberculosis are occurring annually in India, whereas the pool of HIV-infected individual is quite large (~2.5 million). Therefore, there is always a propensity for deadly synergic interactions between HIV and tuberculosis.[2] HIV infections fuels tubercular epidemic in different ways. HIV infection is the most important known risk factor that favors progression to active TB from latent infection by suppressing the immune response against tuberculosis. Exogenous reinfection can also occur as HIV-infected individuals fail to contain new infections. The world health organization (WHO) reported in 2007 that the African region accounted for most HIV-positive tuberculosis cases (79%), followed by the Southeast Asia region (mainly India), which had 11% of total cases. Although the prevalence of HIV infection among patients with tuberculosis ranges from 50% to 80% in many settings in sub- Saharan Africa, in other parts of the world it varies from 2% to 15%.[3] Studies from India have reported HIV seropositivity rates varying from 0.4 to 20.1%.[2] On the other hand, approximately 50% of the HIV-infected people in India are coinfected with M. tuberculosis and approximately 200,000 of these coinfected persons will develop active TB each year in association with HIV infection.[4] Unlike other opportunistic infections, tuberculosis can occur at any stage of HIV disease, and its manifestations depend largely on the degree of immunosuppression. Twenty-five to 65% of HIV-infected persons have been reported to have active TB of one organ or the other in developing countries.[2] Despite the burden of HIV, the epidemiology of tuberculosis in India is being primarily driven by the non-HIV TB-infected pool. Effective implementation of ongoing Revised National TB Control Programme is expected to markedly change the number of new TB cases occurring at any level of HIV prevalence in the country.[5] The aim of the present study is to record the clinical, radiological profile of pulmonary and extrapulmonary tuberculosis (EPTB) in HIV-seropositive persons.
MATERIALS AND METHODS
It was a prospective study, done over a period of 1 year (from 1st June, 2008 to 31st May, 2009) in the department of Medicine at Indira Gandhi Medical College (I.G.M.C), Shimla. All HIV-infected patients admitted to I.G.M.C. Hospital, Shimla and on follow-up at antiretroviral treatment (ART) center were evaluated. Informed consent was taken and patients were assessed clinically. Relevant investigations were undertaken to establish the diagnosis of tuberculosis and other opportunistic infections. HIV infection was diagnosed using three antigenically different rapid kits as per the national HIV testing policy (ELISA/Rapid/Simple) and CD4 cell counts were determined by flow-cytometry technique using Facs Count machine with Facscount™ reagents (Becton Dickinson, USA). ART was started for eligible patients and was guided by baseline and 6-monthly CD4 counts in accordance with the national ART guidelines.[6]
Following investigations were done to establish the diagnosis of tuberculosis:
Ziehl-Neelsen (Z.N) of acid fast bacilli (AFB) from given specimen or culture if indicated.
Histopathological demonstration of typical caseous granulomatous reaction.
Suggestive clinical profile and empirical response to antitubercular therapy (ATT).
Radiological features suggestive of tubercular lesions.
Pleural/ascitic fluid analysis showing evidence of lymphocytic exudative effusion and CSF showing lymphocytic pleocytosis with hypoglycorrhachia (low CSF glucose).
RESULTS
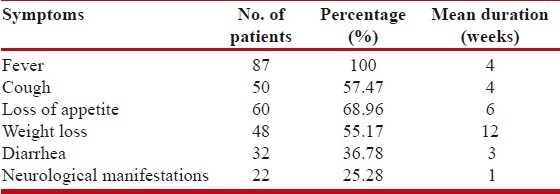
HIV infection is the strongest of all known risk factors for the development of tuberculosis. Of the 87 patients included in our study, males were affected more than females (65.51% males and 34.48% females). The most common affected age group in our study was 31-40 years and mean age of the patients was 34.94 year (range 22-56 years). Unprotected heterosexual contact with professional sex workers was found as the most common mode of HIV transmission. None of the patients had history of intravenous drug abuse and blood transfusion. Most common affected professional group was drivers and majority of affected females were housewives. Fever, weight loss and cough were the commonest symptoms on presentation [Table 1]. Clinical features of neurological involvement were present in 22 (25.28%) patients with mean duration of 1 week prior to diagnosis. Majority of patients with neurological complaints presented with headache and altered sensorium. Beside tuberculosis, commonest opportunistic infection was oral candidiasis. Anemia was detected in 40 patients (45.97%) and ESR was raised in 56 (64.36%) patients.
Table 1.
Showing common symptoms in 87 patients
Chest X-ray was done in all the 87 patients and pulmonary infiltrates was the commonest finding [Table 2]. Ultrasonography abdomen was done in all patients and spleenomegaly was demonstrated in 14 patients. Majority of patients with spleenomegaly had hypoechoic lesions in spleen.
Table 2.
Showing chest X-ray findings

Computed tomography scan (CT scan) of head was done in three patients and all of them had radiological features suggestive of meningitis. Two of the patients also developed hydrocephalous. Magnetic resonance imaging (MRI) of brain done in four patients revealed infarcts and features of meningitis in two patients. Two patients had evidence of CNS tuberculoma and one had hydrocephalous along with CNS tuberculoma.
CD4 count was done in all the patients. Forty-three (49.42%) of them had CD4 cell count ≤ 100 cells/μl and 71 (81.60%) had CD4 cell count ≤ 200 cells/μl and 16 had CD4 count >200 cells/μl. Mean CD4 cell count was 123 cells/μl (in males 119 cells/μl and in females 129 cells/μl).
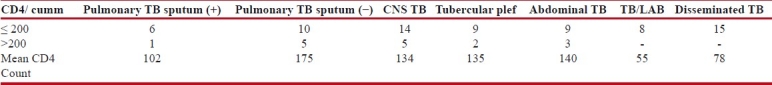
Pulmonary tuberculosis (PTB) was diagnosed in 37 patients and EPTB was reported in 65 patients. Fifteen patients had disseminated tuberculosis and all of them had CD4 count below 200/cumm. Majority of patients with pulmonary and EPTB had CD4 count below 200/cumm (81.08% and 86.15% respectively). Sputum smear-positive pulmonary tuberculosis was reported in 31.81% patients. Majority of them had CD4 count below 200 cells/cmm. Sputum smear-negative tuberculosis was diagnosed on the basis of clinical symptomatology, chest X-ray findings, raised ESR and response to antitubercular chemotherapy.
Commonest form of EPTB in our study was CNS tuberculosis detected in 22 (33.84%) patients followed by abdominal tuberculosis in 17 (26.15%) patients. Tubercular lymphadenopathy and pleural effusion were reported in 21.53% and 18.46% patients, respectively. Commonest form of EPTB in female patients was abdominal tuberculosis and in male patients was CNS tuberculosis. Tubercular meningitis was the commonest manifestation of CNS tuberculosis noticed in 20 (90.90%) patients. Two patients had radiological evidence of CNS tuberculoma. Three patients had vasculitic infarct and hydrocephalous. Three patients with CNS tuberculosis also had disseminated tuberculosis. One patient had craniospinal meningitis. Seventeen patients with CNS tuberculosis had CD4 count below 200/cumm. Mean CD4 cell count in patients with CNS tuberculosis was 134 cells/cumm.
Analysis of cerebrospinal fluid showed pleocytosis (mean white cell count 204/cmm with mean lymphocyte percentage of 65.61%), hypoglycorrhachia (mean glucose level, 33.14 mg/dl) and mean protein level of 187 mg/dl. All patients with meningitis were immediately started on ATT along with steroids after cryptococcal meningitis being ruled out by India ink staining. There were only two (9.09%) deaths during hospital stay.
Seventeen patients (26.15%) in our study had abdominal tuberculosis. Commonest form of abdominal tuberculosis was tubercular lymphadenopathy followed by spleenic tuberculosis and ascites, respectively. Imaging studies by USG and CT scan abdomen, analysis of ascitic fluid and response to ATT were the criteria used for diagnosis of abdominal tuberculosis. Fourteen patients with abdominal tuberculosis had CD4 count below 200/cumm. Ten out of 11 patients with hypoechoic lesions in spleen on USG had CD4 count below 200 cells/μl. Mean CD4 cell count of patients with abdominal tuberculosis was 140 cells/cumm. Peripheral lymphadenopathy was present in 20 patients and abdominal lymphadenopathy in 14 patients. Axillary lymphadenopathy was the commonest lymph node involvement present in 16 patients followed by cervical lymphadenopathy in 12 patients. Six had generalized lymphadenopathy. Fourteen patients had tubercular lymphadenopathy which was diagnosed on the basis on fine needle aspiration cytology (FNAC) and lymph node biopsy. Ziehl-Neelson staining for AFB was positive in eight out of 14 patients (57.14%) with lymph node tuberculosis. Rest of the patients were diagnosed on the basis of granulomatous lymphadenitis and response to ATT. Majority (85.71%) of lymph node tuberculosis was diagnosed by FNAC. Thirteen out of 14 patients with tubercular lymphadenopathy had CD4 count below 200/cumm. All the patients with AFB-positive lymph node had CD4 count below 200/cum.
DISTRIBUTION OF ISOLATED PTB AND EPTB
Table 3 depicts the distribution of isolated pulmonary and EPTB. All patients with disseminated tuberculosis had CD4 cell count less than 200/cumm. This observation is statistically significant (P-value <0.042).
Table 3.
Showing distribution of pulmonary and extrapulmonary tuberculosis
DISCUSSION
Recently, HIV estimate for India has been revised to less than half; however, most of this drop is not due to an actual decrease in HIV burden but due to availability of more reliable population-based data.[7,8] Tuberculosis is the most common opportunistic infection in HIV-positive persons and may develop at any stage of the disease. Maximum patients in our study were in the age group of 31-40 years (68.96%) and majority (65.61%) were males. Commonest profession in males was drivers and all affected females were housewives. Unprotected heterosexual sex was the commonest mode of transmission. Other Indian studies also showed unprotected heterosexual sex as the commonest mode of transmission.[9,10] Commonest finding noted in chest radiography was pulmonary infiltrates. Other features are pleural effusion, cavity, military shadows and fibrotic changes. Twenty-one (63.63%) patients had abnormality in upper zone and 12 patients (36.36%) had lower and mid-zone involvement. It was similar to observation by Zuber Ahmed et al.[11] Isolated pulmonary tuberculosis was found in 25.28% patients and EPTB in 57.47% patients. Fifteen patients (17.24%) had disseminated tuberculosis. Other studies also reported higher prevalence of EPTB of 53-63% of total tuberculosis cases in HIV-infected patients, and was seen more frequently in severely immunocompromised HIV patients.[12,13] All the patients with disseminated tuberculosis had CD4 count below 200/cumm. Overall 71 out of 80 (81.60%), seven patients with all form of tuberculosis had CD4 count below 200/cumm. This study showed that the prevalence of tuberculosis, both pulmonary and EPTB, in HIV-infected patients is significantly higher with majority having CD4 cell count <200/cmm. Commonest form of EPTB in our study group was CNS tuberculosis diagnosed in 22 (33.84%) patients followed by abdominal tuberculosis in 17 (26.15%), peripheral tubercular lymphadenitis in 14 (21.53%) and pleural effusion in 12 (18.46%) patients.
Brig S K Sharma et al in a study EPTB in HIV-positive patients noted lymph node involvement as the most common EPTB site followed by spleen.[14] The difference in our study could be because of adequate inclusion of hospitalized immunocompromised patients. Many of our patients were admitted with meningoencephalitis, pleural effusion, organomegaly and on investigations found to be immunocompromised. Hence our study is more representative as it has both in hospital and community based data. Fourteen patients in our study group had tubercular lymphadenitis which was diagnosed on basis on FNAC and lymph node biopsy. ZN staining for AFB was positive in eight out of 14 (57.14%) patients with lymph node tuberculosis. FNAC was diagnostic in 12 out of 14 (85.71%) patients. All the patients with AFB-positive lymph node had CD4 count below 200/cum. The diagnostic role of FNAC and AFB smear examination has also been reported by Artenstein et al and fine needle aspiration is more reliable in patients with HIV infection because of the higher mycobacterial burden, and should be the initial diagnostic procedure in these patients.[15]
CONCLUSIONS
HIV infection most commonly affects the younger economically productive section of the society. It is more common in professionals practicing high risk sexual behavior. Tubercular coinfection is common in HIV infected and more so with falling CD4 cell level. The salient features of our study were higher prevalence of EPTB in HIV-infected patients unlike many other Indian studies. Commonest EPTB was CNS tuberculosis unlike most other Indian studies where either lymphnode or pleura were the commonest site of involvement. In hospital mortality in patients of CNS tuberculosis was lower in our study perhaps due to high index of suspicion, prompt diagnosis and early institution of treatment. Disseminated tuberculosis was only found in patient with CD4 count less than 200/cmm. There is a definite role of FNAC in diagnosis of tubercular lymphadenitis in HIV-positive patients.
Early diagnosis of tuberculosis and prompt institution of ATT reduces mortality and morbidity significantly. In resource poor areas, the diagnosis can be established with cytological/biochemical analysis of fluid, histopathological examination and ZN staining of tissue coupled with radiological features and response to ATT. Therefore, adequate knowledge of the manifestations of tuberculosis in HIV-infected patients is absolutely necessary for optimal management and to reduce mortality and morbidity.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Swaminathan S, Ramachandran R, Bhaskar R, Ramanathan U, Prabhakar R, Datta M, et al. Development of tuberculosis in HIV infected individuals in India. Int J Tuberc Lung Dis. 2000;4:839–44. [PubMed] [Google Scholar]
- 2.Sharma SK, Mohan A, Kadhiravan T. HIV-TB co-infection: Epidemiology,diagnosis and management. Indian J Med Res. 2005;121:550–67. [PubMed] [Google Scholar]
- 3.World Health Organization (WHO) Global tuberculosis control: Surveillance, planning, financing-WHO report 2009. Chapter1, Epidemiology. Document WHO/HTM/TB/2009.411. [Last cited on 2009]. Available from: http://www.who.int/tb/publications/global_report/2009/en .
- 4.Khatri GR, Frieden TR. Controlling tuberculosis in India. N Engl J Med. 2002;347:1420–5. doi: 10.1056/NEJMsa020098. [DOI] [PubMed] [Google Scholar]
- 5.Central TB Division. TB India 2007; RNTCP status report. Central TB Division. New Delhi: Directorate General of Health Services, Ministry of Health and Family Welfare, Government of India; 2007. p. 10. [Google Scholar]
- 6.National AIDS Control Organization. New Delhi: Ministry of Health and Family Welfare, Government of India; 2007. May, National AIDS Control Organization. Anti retroviral therapy guidelines for HIV infected adult and adolescents including post exposure prophylaxis; pp. 7–8. (18-24). [Google Scholar]
- 7.Dandona L, Dandona R. Drop of HIV estimates for India to less than half. Lancet. 2007;370:1811–3. doi: 10.1016/S0140-6736(07)61756-5. [DOI] [PubMed] [Google Scholar]
- 8.Cohen J. India slashes estimate of HIV-infected people. Science. 2007;317:179–81. doi: 10.1126/science.317.5835.179. [DOI] [PubMed] [Google Scholar]
- 9.Adhikari AK. Clinical spectrum of patients of HIV/AIDS. J Assoc Physicians India. 2003;51:1258. [Google Scholar]
- 10.Kumarasamy N, Solomon S, Jayaker Paul SA, Venilla R, Amalraj RE. Spectrum of opportunistic infections among AIDS patients in Tamilnadu. India. Int J AIDS. 1995;6:447–9. doi: 10.1177/095646249500600615. [DOI] [PubMed] [Google Scholar]
- 11.Mohd S, Zuber A. Manifestations of tuberculosis in HIV infected patients. J Indian Acad Clin Med. 2005;6:302–5. [Google Scholar]
- 12.Perronne C, Zahraoui M, Leport C, Salmon D, Pangon B, Bricaire F, et al. Tuberculosis in patients infected with the human immunodeficiency virus. Presse Med. 1988;17:1479–83. [PubMed] [Google Scholar]
- 13.Jones BE, Young SM, Antoniskis D, Davidson PT, Kramer F, Barner PF. Relationship of the manifestations of tuberculosis to CD4 cell counts in patients with human immunodeficiency virus infection. Am Rev Respir Dis. 1993;148:1292–7. doi: 10.1164/ajrccm/148.5.1292. [DOI] [PubMed] [Google Scholar]
- 14.Sharma SK, Deoskar RB, Rajan KE, Barthwal MS. Extra pulmonary tuberculosis in HIV infection. Med J Armed Forces India. 2005;61:340–41. doi: 10.1016/S0377-1237(05)80059-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Artenstein AW, Kim JH, Williams WJ, Chung RC. Isolated peripheral tuberculous lymphadenitis in adults: Current clinical and diagnostic issues. Clin Infect Dis. 1995;20:876–82. doi: 10.1093/clinids/20.4.876. [DOI] [PubMed] [Google Scholar]


