Abstract
The burden of chronic obstructive pulmonary disease (COPD) has increased recently in developing countries. On the other hand, structured or non-structured rehabilitation services for COPD patients are not routinely available in these countries. We, therefore, planned this review to re-emphasize the emerging benefits of pulmonary rehabilitation in COPD population. Aim of this review is to stimulate pulmonary physicians in India and other resource-poor areas of the world so that they start using pulmonary rehabilitation or its components more often. The search included standard english literature PubMed citation of relevant original articles, review articles and practice guidelines. The articles and reviews were searched including standard MeSH terms – Rehabilitation (TIAB) and pulmonary disease, chronic obstructive/therapy (MAJOR) and guidelines (TIAB). Available 58 articles in English including 23 reviews from July 2001 to October 2010 were screened for evidence-based benefits regarding respiratory rehabilitation as a whole or its different components. The cross references and current citations relating to primary articles were also included for description. No attempt was done to make a systematic analysis because our purpose was not to derive evidence-based recommendations from database and because sufficient evidence is already available for benefits of selected components of pulmonary rehabilitation in COPD patients. Pulmonary rehabilitation has emerged as an important modality as an adjunct to other therapies in patients of COPD. Limited and more cost-effective protocols are to be developed and executed by healthcare providers, especially in developing countries like India.
KEY WORDS: Chronic obstructive pulmonary disease, guidelines, rehabilitation
INTRODUCTION
How is a Mount Everest winner different from a healthy person of his age with sedentary habits? An Everest winner can manage to climb 30,000-feet high mountain, while a sedentary healthy person may feel difficulty in climbing even a 300-feet high hill. How can one explain such a difference in great performance and capabilities? Capability of higher work performance can be attained by proper conditioning of body by regular practice so that oxygen and body energy are utilized optimally. Can we utilize the performance improvement skills in patients with crippling respiratory diseases such as chronic obstructive pulmonary disease (COPD)? Pulmonary rehabilitation deals with this aspect. Recent evidence-based guidelines have contributed significantly to the clarification of this question.[1,2] In patients with COPD, rehabilitation has been recognized as an established modality of treatment as it can increase functional capacity, leads to improvement in dyspnea and quality of life.[1] The role of rehabilitation in other respiratory disorders is less clearly established; however, further work is in progress. Some of these studies are highly disease specific and fall outside the scope of this review.
With the availability of inhaled and other modern means of therapy, we now have highly effective treatment to reduce the agony of COPD patients to a certain extent. Despite the availability of effective therapy, many patients in developing countries still have to suffer due to ignorance, lack of understanding and faulty perception of the disease. The practical use of rehabilitation in respiratory diseases is virtually non-existent in such countries. Worldwide organized rehabilitation facilities are limited to urban or semi-urban settings. In countries like India where most of the population lives in rural setting, the burden of diseases like COPD is rising.[3] Widespread dissemination of structured rehabilitation services is difficult. To be widely acceptable, pulmonary rehabilitation ought to be applied in a cost-effective and logical manner in such a scenario. Therefore, there is an urgent need of recapitulating basic principles of rehabilitation with respect to respiratory diseases. This review aims to highlight the role of pulmonary rehabilitation in COPD, concentrating mainly on clinical utility of various aspects of pulmonary rehabilitation.
HISTORICAL ASPECTS
As for coronary artery disease patients, rest was considered essential part of the treatment for respiratory patients during the first half of the last century.[4] In 1952, Barach suggested that in chronic respiratory patients, the progressive improvement in ability to walk without dyspnea might be a physiological response similar to a training program in athletes.[5] In 1960s, Petty established a standardized out-patient program of pulmonary rehabilitation.[6] In 1980, the American Thoracic Society acknowledged benefits of pulmonary rehabilitation notably and included exercise conditioning as an important constituent in treatment program. However, during this period, some trials showed no significant benefit.[7,8] The failure to show benefit was probably because these studies looked for effect in only an individual variable related to exercise. After the mid 1980s, important and more comprehensive work in rehabilitative research by Ries et al. and Casaburi et al. established the role of pulmonary rehabilitation for patients with chronic respiratory diseases.[9,10]
In 1999, a group of experts under the auspices of the American Thoracic Society produced a document that reviewed the state of the art management of pulmonary rehabilitation in patients with COPD.[11]
DEFINITION
The definition of pulmonary rehabilitation has been continuously revised over the last many years and the latest one is specified by American College of Chest Physicians (ACCP) and the American Association of Cardiovascular and Pulmonary Rehabilitation (AACPR) as follows: “Pulmonary rehabilitation is an evidence-based, multidisciplinary and comprehensive intervention for patients with chronic lung disorders who are symptomatic and have some disability. Pulmonary rehabilitation is aimed to decrease symptoms, optimize functional state, increase participation, and reduce health-care costs through stabilizing or reversing systemic manifestations of the disease”.[12] To simplify, a symptomatic COPD patient has some compromise in functional state, depending on the stage of the disease which can be rectified by rehabilitation.
THE “EFFECTS“ OR “BENEFITS” OF EXERCISES
Patients with respiratory disease have limitation of their work capacity, mainly because lungs are unable to perform the normal function of either alveolar ventilation or diffusion of the gases across the alveolar-capillary barrier. It causes reduced oxygen supply to the skeletal muscles. The most significant systemic dysfunction in COPD patients is skeletal muscle dysfunction due to anaerobic environment and subsequent lactic acidosis produced inside the muscle. Sedentary lifestyle and some disease-specific factors may also contribute to this dysfunction.[13] Decreased aerobic enzyme activity, increased inflammatory cells, apoptosis and even low number of aerobic fibers (change of type IIa muscle fibers to type IIb fibers) have been shown in muscles of COPD patients.[14]
High-intensity rehabilitation exercises alter the muscle metabolism in a direction that enables a person to tolerate higher magnitude of work without appreciable dyspnea. Peak oxygen consumption (VO2 max) is improved by such training. With rehabilitation, structural changes are also observed such as conversion of type IIb muscle fibers to type IIa fibers, increased number of mitochondria in type I fibers and increased activity of mitochondrial enzymes like citrate synthetase and 3-hydroxyacyl-COA dehydrogenase. It leads to more aerobic metabolism and therefore less lactic acid and less CO2 production for a given level of exercise.[15–17]
Dynamic hyperinflation present in COPD patients is also reduced because exercise conditioning leads to reduced demand on the system and hence lower respiratory rate for a given level of exercise.[17] Additional beneficial effect of rehabilitation is desensitization to dyspnea [Figure 1].
Figure 1.
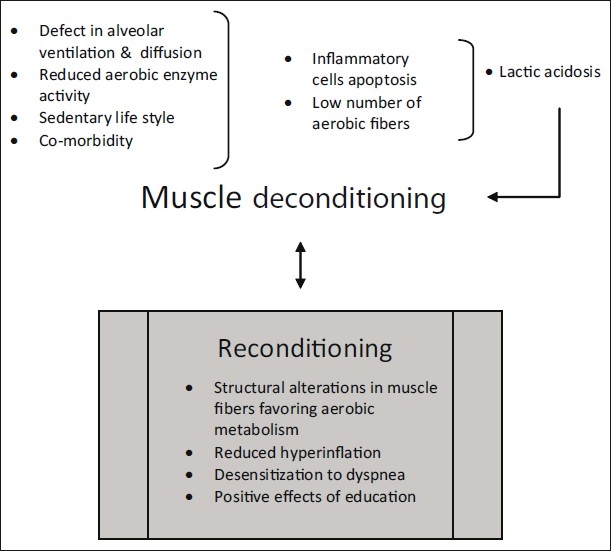
Muscle deconditioning due to chronic respiratory illness can be reversed back to improved muscle physiology by rehabilitation
AIMS OF REHABILITATION
The basic goals of pulmonary rehabilitation are to (1) improve symptoms, (2) restore functional capabilities, and (3) enhance overall quality of life. Thus, an ideal pulmonary rehabilitation program should be structured to bring about specific changes in underlying pathophysiology to improve functional capabilities, leading to symptomatic improvement and reduction in handicap, thereby refining quality of life in a cost-effective and individualized manner.[18] With the help of education, the rehabilitation also aims to relieve fears and anxiety associated with program and lung condition, thereby ensuring long-term commitment to exercise.
TYPES OF PULMONARY REHABILITATION PROGRAMS
Out-patient, in-patient and home-based programs are three basic types of pulmonary rehabilitation. Each patient is prescribed a customized program that is most appropriate for his needs. With out-patient program higher intensity exercises can be achieved, and therefore it gives the best results. Out-patient program is relatively easy since it can be conducted by only a few persons, e.g., a program supervised by physiotherapists.[19] More disabled patients cannot attend out-patient programs regularly, therefore they are advised in-patient programs. People requiring optimization of medical and ventilatory treatment may also be subjected to in-patient pulmonary rehabilitation.[18] Home-based programs are also effective, but can be inferior in efficacy to the out-patient and in-patient programs.[20] Home-based program is used when other programs are not available or when exercise is more important than other aspects of rehabilitation.[21]
EVIDENCE FOR EFFECTIVENESS OF PULMONARY REHABILITATION
Patients with COPD
Various randomized controlled trials (RCTs) have shown the effectiveness of pulmonary rehabilitation for COPD patients.[22–24] Ries and his colleagues studied 119 COPD patients, comparing the effect of a comprehensive pulmonary rehabilitation program and education alone (control group). They showed significant benefits of comprehensive pulmonary rehabilitation in improving exercise performance and important symptoms.[18]
Cochrane meta-analysis examined the effect of 23 randomized trials.[25] It was seen that pulmonary rehabilitation for COPD improves dyspnea and disease-specific quality of life. Functional exercise capacity as assessed by 6-minute walk distance was also increased by 49 m. The benefits were more in severe COPD as compared to mild and moderate disease and effects were maintained for up to 6 months. In these studies, supervised programs provided greater benefit than unsupervised programs. Though lack of blinding and heterogeneity among studies were the limiting factors in these studies, yet results were impressive. Importantly, the Cochrane review concluded that no additional trials are needed to compare pulmonary rehabilitation with conventional community care in patients with COPD. However, they suggested the need of additional studies to determine essential components, duration, intensity and frequency of an ideal rehabilitation program. They also recommended in favor of more homogeneity in reporting of pulmonary rehabilitation studies in future. A few other studies have found reduction in anxiety and depression after pulmonary rehabilitation in patients with COPD.[26–28]
Non-COPD disorders
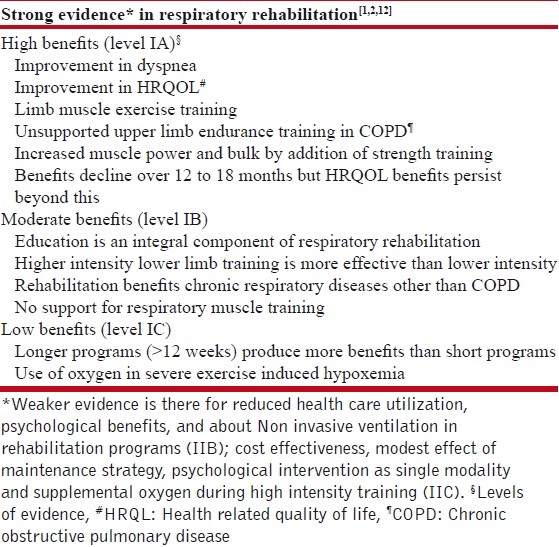
Though the work is limited, yet rehabilitation may seem to be of significant advantage for patients with many non-COPD disorders.[29,30] As long as patients have enough reserve to perform some exercise, it is likely that they can obtain a training benefit. Pulmonary rehabilitation has been used in diseases such as asthma, cystic fibrosis, interstitial lung disease (ILD), obesity-related respiratory disorders, pulmonary hypertension, neuromuscular and chest wall disorders.[1] Studies have shown that pulmonary rehabilitation is important for patients with idiopathic pulmonary fibrosis and ILD.[31,32] An Indian study incorporating 6 weeks of home-based pulmonary rehabilitative program was effective in increasing exercise endurance in patients with ILD.[33] Table 1 summarizes the recommendations based on current evidence.[2,12,34]
Table 1.
Current evidence favoring various aspects related to rehabilitation
ESSENTIAL COMPONENTS OF PULMONARY REHABILITATION
Team
The program schedule is implemented by a team consisting of a program coordinator and a rehabilitation specialist.[35] The team should meet initially to evaluate patient assessment and develop a coordinated treatment plan [Figure 2]. At the time of discharge of the patient, the team should meet again for planning of discharge and post-program treatment.
Figure 2.
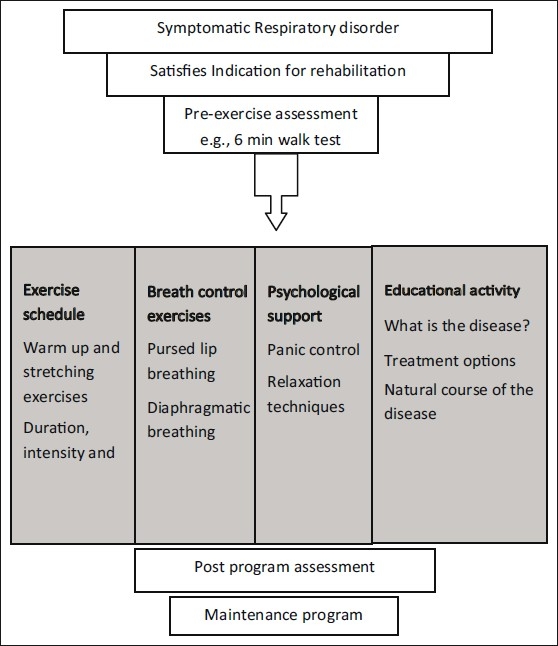
Diagrammatic presentation of various important steps in rehabilitation
Pre-program evaluation (patient selection) – indications and contraindications
Indications
Any patient, who is suffering from long-term symptomatic respiratory illness, is a candidate for pulmonary rehabilitation program. Unfortunately, exercise modality is usually considered to be the last option in management of a respiratory disorder. If the consequences of COPD are to be minimized, patients should be referred early during the course of disease. Following are some of the important indications of pulmonary rehabilitation in general:[18]
Symptomatic respiratory dysfunction
Dyspnea of at least Medical Research Council (MRC) grade III
Sufficiently motivated patient who can take part in intensive program schedule
Preoperative rehabilitation for lung volume reduction surgery or lung transplantation
Evaluation of elective mechanical ventilation or home oxygen
Contraindications
In broad sense, contraindications indicate inability of the patient to follow the rehabilitation program due to any reason. These may include patients having:[18]
Angina pectoris, recent myocardial infarction, severe pulmonary hypertension
Congestive heart failure
Unstable diabetes
Inability to do exercise due to orthopedic or other reasons
Psychiatric illness, dementia
Severe exercise-induced hypoxemia, not correctable with O2 supplementation
Lack of motivation, non-adherence, unwilling to give consent
Active cigarette smoking is considered as a relative contraindication in some countries
Initial evaluation
Initial testing is done to judge the exercise ability of a COPD patient by simple symptom-limited exercise tests. The initial maximal exercise capacity can be better evaluated by dyspnea scores.[36] Usually, Borg 0-10 scale or visual analogue scale is recorded during ECG monitored and supervised baseline incremental exercise test. Baseline 6-minute walk test (6-MWT) is done.[37] Pulmonary function tests including spirometry, lung volume measurement and diffusion capacity for carbon monoxide (DLCO) are performed. Quality of life is most commonly assessed by Saint George Respiratory Questionnaire (SGRQ).
Rehabilitation exercise training
Exercise is the core component of the rehabilitation program.[38]
Lower limb
Lower limb muscle dysfunction is largely responsible for exercise limitation in COPD patients.[39] Exercise training has muscle group specific effect and lower extremity training provides the best physiological gains, according to the present evidence-based guidelines.[1,2,12] It has been seen that reducing the total metabolic demand by using one-legged training may also improve aerobic capacity compared with conventional two-legged training in patients with stable COPD.[40] Lower extremity exercises are usually done by treadmill walking or cycle ergometer. Corridor walk or modified weight lifting may also be considered.
Upper limb
Upper extremity training is also useful as it has been shown to decrease oxygen demand and increase arm muscle capacity at similar work level following pulmonary rehabilitation. Unsupported upper limb exercises including weight lifting are superior to supported exercises like arm ergometry.[12] Upper extremity training is usually done with arm ergometry, arm weight lifting or throwing.
Combined upper and lower limb training
Combined upper limb and lower limb training results in a significant improvement in the exercise performance and health-related quality of life.[41]
The usual schedule may incorporate:
minimum three sessions per week for 4, 6, 8 or 12 weeks;
30 minutes to 1 hour is given to each session of exercise;
intensity/duration of exercise is usually limited by symptom; and
type of exercise can be continuous/intermittent and endurance/strength training.
Exercise training begins at a level which can be tolerated by a patient without discomfort. Subsequently, exercises are increased in graded manner. Duration of exercise is increased first and then the intensity. In COPD patients with less severe disease, activities like walking, bike riding, swimming or golfing may be used. High-intensity exercise, just below 80% of maximum work capacity, is more useful than low-intensity exercise, below 50% maximum work capacity, and strength training is useful in improving muscle mass and strength.[42,43]
Inspiratory muscle training
Present evidence does not support these exercises to be of significant physiological benefits.[12,44] Inspiratory muscle training may be accepted as an adjunct to limb training as better methods of evaluation of respiratory muscle training become available in the future. In a recent meta-analysis, inspiratory muscle endurance training was found to be less useful than respiratory muscle strength training in general. However, in patients with inspiratory muscle weakness, additional inspiratory muscle training led to improvement in exercise performance.[45]
Chest physical therapy techniques
Though chest physical therapy is practiced for centuries, in modern rehabilitation schedules it is used as a combined modality.[2] Chest physical therapy techniques include: a) breath retraining-purse lip breathing, diaphragmatic breathing exercises and b) chest physiotherapy – postural drainage, chest percussion, vibration, and directed cough. In purse lip breathing, patient inhales through nose and then exhales over 4-6 seconds through partly opened lips. It produces a whistling sound. In diaphragmatic breathing, a patient breathes mainly with the help of abdomen. He places dominant hand on upper mid-abdomen and the other hand on the upper chest to have mainly abdominal movements. Patient breathes slowly through nose and exhales through purse lip with a conscious effort to move diaphragm during inspiration to protrude upper abdomen and displace the dominant hand maximally. It facilitates outward movement of abdominal wall and reduces upper chest movement during inspiration. These excursions can be measured during a respiratory cycle.[46] Energy conservation techniques, e.g., while eating or climbing stairs and effective positioning of body may also be suggested during these sessions.
Limited and individualized protocols
It can be seen from above that not only more complex standard protocols but also individual components are effective. Individual protocols can be developed by chest physicians in collaboration with physical therapy experts considering practical utility and cost-effectiveness. All one needs to do is to make best use of available evidence. One can issue charts similar to diet charts given to diabetic patients with different caloric requirements. Practical tips on the difficulties related to exercise in COPD and their solution may be included in these charts.
On-call physiotherapy
On-call physical therapy means providing respiratory physical therapy as required by the patient out of business hours. According to a recent study by Babu et al., it can lead to a significant increase in pulmonary function parameter, 6-MWT distance and sustained maximal inspiration.[47]
Psychosocial assessment and intervention
Anxiety and depression are common in chronic lung disorders and can contribute to significant morbidity and mortality.[48] These co-morbidities complicate the course of the disorder, leading to a compromised functional and social life which further culminates into de-conditioning. Psychosocial interventions for these patients include disability evaluation, vocational counseling and continued education of patient and family. In addition to the studies mentioned above, many others have shown that pulmonary rehabilitation improves anxiety and depression associated with COPD.[27,49]
Nutritional interventions
Resting energy expenditure is higher in COPD patients with weight loss, which is due to an increased resistive load imposed on respiratory muscles. Other probable pathophysiologic mechanisms that result in weight loss in COPD patients include systemic inflammation, tissue hypoxia, medications, inadequate dietary intake and catabolic/anabolic ratios.[50] Weight loss in COPD patients is also associated with more severe lung function impairment. Undernourishment probably leads to deleterious consequences in these patients due to decreased respiratory muscle mass and muscle strength, decreased ventilatory response to hypoxia, decreased cell-mediated immunity and poor wound healing. COPD patients in India are significantly malnourished probably because of the underlying malnutrition.
Outcome assessment
One of the most important aspects of pulmonary rehabilitation is assessment of benefits of the program [Figure 3]. Quality of life, dyspnea and functional parameters can be assessed on various scales.[51,52] The assessment can be real time (during program) or recall assessment (after completion of program).
Figure 3.
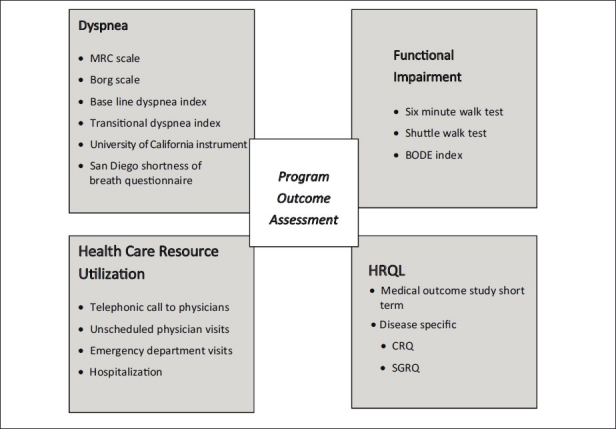
Program can be assessed usually with parameters like dyspnea scales, walk tests, health care resource utilization measures and quality of life parameter evaluation
Quality of life: It can be assessed by different types of questionnaire-based instruments. These include SGRQ, Chronic Respiratory Disease Questionnaire (CRDQ) and Medical Outcome Study Short Form-36 (MOS SF-36) scales. Very commonly used SGRQ is self-administered, contains 50 items, and takes 10-15 minutes to complete. There are three separate scales based on symptoms, activity and impact on daily life.
Dyspnea
It can also be assessed with various scales such as Borg scale, MRC scale, baseline dyspnea index, transitional dyspnea index, University of California instrument and San Diego shortness of breath questionnaire. Among them, Borg scale and MRC dyspnea scale are more commonly used tools[53,54] [Table 2]. Borg scale is a 10-point scale which represents entire range of severity of dyspnea. The patient is asked to select a point on this scale that corresponds to his perception of dyspnea. A change of 1 cm is believed to be the minimal clinically important difference. The MRC dyspnea scale is a set of five statements about dyspnea. The subject is asked to select the statement that most closely applies to the situation. Both scales are easy to use and quick to perform and are capable of detecting long- and short-term changes.
Table 2.
Measurements of breathlessness in exercise
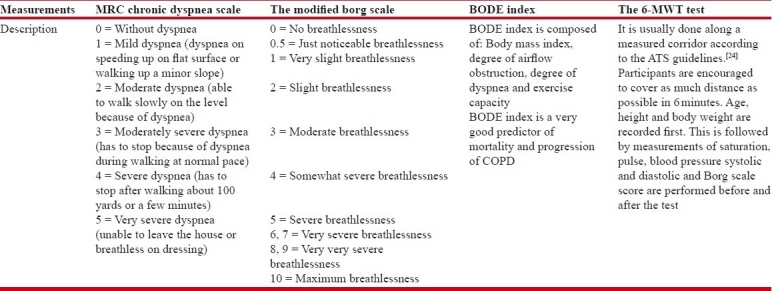
Functional assessment
It can be done with 6-MWT, shuttle walk test or BODE (Body mass index, Obstruction, Dyspnea, Exercise capacity) index[37,55] [Table 2]. Among a variety of field tests, the most widely used is the 6-MWT. It is a supervised measurement of the distance a patient can walk on the level surface in 6 minutes. Reference values are 576 m for healthy male subjects and 494 m for healthy female subjects. The distances for patients with COPD are generally less but are variable. The threshold of clinically significant change, as a result of rehabilitation program, has been reported to be 54 m for groups and 86 m for an individual patient.
Maintenance program
Rehabilitation programs are usually not associated with sustained benefits beyond 12 months. Therefore, a maintenance program is required to sustain the benefits of a successful rehabilitation program. It is important to note here that cycle ergometers or treadmills are expensive items and are not routinely available especially in rural settings, therefore, simple walk test e.g., timed walk test or corridor walking can be incorporated into exercise schedules. Ideal time to enroll a patient for full pulmonary rehabilitation is shortly after hospitalization for a COPD exacerbation.[56,57]
ANCILLARY THERAPY
These therapies are the measures commonly used for the treatment of the respiratory disease and are of considerable help during a rehabilitation program. Bronchodilators, oxygen, and non-invasive ventilation (NIV) have been used successfully in rehabilitation programs.
Bronchodilators
Bronchodilators have been shown to have beneficial effects like reduced dyspnea, increased endurance, improved quality of life and reduced exacerbation frequency in patients with respiratory disease on rehabilitation.[58,59] Additionally, they reduce the resistive work of breathing by increasing airway diameter, thereby decreasing dyspnea. Another important benefit of bronchodilators is that they also reduce the elastic work of breathing by decreasing static and dynamic hyperinflation.[60,61] Bronchodilator therapy may allow patients with COPD to do exercise training at higher intensities or at higher anaerobic threshold, and therefore increases the likelihood of a substantial benefit in exercise performance.[62,63]
Oxygen
Use of oxygen during rehabilitation has been shown to help an individual to undergo higher intensity of exercise training.[64,65] Oxygen may be supplied continuously or on demand basis, according to the need of individual patient. Although the acute effect of oxygen administration on increasing exercise capacity has been demonstrated in the laboratory, studies showing the superiority of supplemental oxygen to room air use during exercise training in pulmonary rehabilitation have given mixed results.[66–69] It remains to be determined whether supplemental oxygen will become an established option as an exercise enhancer for non-hypoxemic patients with COPD in the respiratory rehabilitation.
Other ancillary therapies
NIV, ventilation feedback, neuromuscular stimulation and helium-hyperoxia are some of the adjunctive therapies.[70–73]
CONCLUSION
Effective pulmonary rehabilitation incorporates exercise schedules and patient education comprehensively to encompass treatment and other aspects needed to make any individual patient recover gradually from the deterioration of the condition and to remain in a fully functional state as far as possible. Looking at the increasing burden of COPD patients in developing countries, there is an urgent need of advocacy of pulmonary rehabilitation in complete management of this disease. The evidence-based approach, applied in a practical manner, suitable to individual, community or geographic region will definitely help to reduce morbidity associated with chronic respiratory diseases like COPD.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Nici L, Donner C, Wouters E, Zuwallack R, Ambrosino N, Bourbeau J, et al. American Thoracic Society/European Respiratory Society statement on pulmonary rehabilitation. Am J Respir Crit Care Med. 2006;173:1390–413. doi: 10.1164/rccm.200508-1211ST. [DOI] [PubMed] [Google Scholar]
- 2.Global strategy for the diagnosis, management and prevention of chronic obstructive pulmonary disease (Updated 2009) [Last accessed on 2011 Aug 11]. Available from: www.goldcopd.org .
- 3.Parekh KR, Adusumilli PS, Patterson GA. Lung transplantation in India: A possible treatment option. Natl Med J India. 2008;21:228–33. [PubMed] [Google Scholar]
- 4.Casaburi R. A brief history of pulmonary rehabilitation. Respir Care. 2008;53:1185–9. [PubMed] [Google Scholar]
- 5.Barach AL, Bickerman HA, Beck G. Advances in the treatment of non-tuberculous pulmonary disease. Bull N Y Acad Med. 1952;28:353–84. [PMC free article] [PubMed] [Google Scholar]
- 6.Petty TL, Nett LM, Finigan MM, Brink GA, Corsello PR. A comprehensive care program for chronic airway obstruction. Methods and preliminary evaluation of symptomatic and functional improvement. Ann Intern Med. 1969;70:1109–20. doi: 10.7326/0003-4819-70-6-1109. [DOI] [PubMed] [Google Scholar]
- 7.Haber P. Exercise training fails to increase skeletal muscle enzymes in patients with chronic obstructive pulmonary disease (letter) Am Rev Respir Dis. 1981;124:347. doi: 10.1164/arrd.1981.123.3.256. [DOI] [PubMed] [Google Scholar]
- 8.Belman MJ. Exercise in chronic obstructive pulmonary disease. Clin Chest Med. 1986;7:585–97. [PubMed] [Google Scholar]
- 9.Ries AL, Archibald CJ. Endurance exercise training at maximal targets in patients with chronic obstructive pulmonary disease. J Cardiopulm Rehabil. 1987;7:594–605. [Google Scholar]
- 10.Casaburi R, Wasserman K. Exercise training in pulmonary rehabilitation. N Engl J Med. 1986;314:1509–11. doi: 10.1056/NEJM198606053142310. [DOI] [PubMed] [Google Scholar]
- 11.Pulmonary rehabilitation 1999. American Thoracic Society. Am J Respir Crit Care Med. 1999;159:1666–82. doi: 10.1164/ajrccm.159.5.ats2-99. [DOI] [PubMed] [Google Scholar]
- 12.Ries AL, Bauldoff GS, Carlin BW, Casaburi R, Emery CF, Mahler DA, et al. Pulmonary rehabilitation: Joint ACCP/AACVPR evidence based clinical practice guidelines. Chest. 2007;131(5 Suppl):4S–42S. doi: 10.1378/chest.06-2418. [DOI] [PubMed] [Google Scholar]
- 13.Casaburi R, Zuwallack R. Pulmonary rehabilitation for management of chronic obstructive pulmonary disease. N Engl J Med. 2009;360:1329–35. doi: 10.1056/NEJMct0804632. [DOI] [PubMed] [Google Scholar]
- 14.Agustí AG, Sauleda J, Miralles C, Gomez C, Togores B, Sala E, et al. Skeletal muscle apoptosis and weight loss in chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2002;166:485–9. doi: 10.1164/rccm.2108013. [DOI] [PubMed] [Google Scholar]
- 15.Casaburi R. Physiologacal responses to training. Clin Chest Med. 1994;15:215–27. [PubMed] [Google Scholar]
- 16.Ries AL. The importance of exercise in pulmonary rehabilitation. Clin Chest Med. 1994;15:327–37. [PubMed] [Google Scholar]
- 17.Porszasz J, Emtner M, Goto S, Somfay A, Whipp BJ, Casaburi R, et al. Exercise training decreases ventilatory requirements and exercise induced hyperinflation at sub-maximal intensities in patients with COPD. Chest. 2005;128:2025–34. doi: 10.1378/chest.128.4.2025. [DOI] [PubMed] [Google Scholar]
- 18.Hill NS. Pulmonary rehabilitation. Proc Am Thorac Soc. 2006;3:66–74. doi: 10.1513/pats.200511-121JH. [DOI] [PubMed] [Google Scholar]
- 19.Hui KP, Hewitt AB. A simple pulmonary rehabilitation program improves health outcomes and reduces hospital utilization in patients with COPD. Chest. 2003;124:94–7. doi: 10.1378/chest.124.1.94. [DOI] [PubMed] [Google Scholar]
- 20.Puente-Maestu L, Sanz ML, Sanz P, Cubillo JM, Mayol J, Casaburi R. Comparison of effects of supervised versus self monitored training programmes in patients with chronic obstructive pulmonary disease. Eur Respir J. 2000;15:517–25. doi: 10.1034/j.1399-3003.2000.15.15.x. [DOI] [PubMed] [Google Scholar]
- 21.Pande A, Singhal P, Kumar R, Gaur SN. Effect of home-based pulmonary rehabilitation programme on disability in patients with chronic obstructive pulmonary disease. Indian J Chest Dis Allied Sci. 2005;47:217–19. [PubMed] [Google Scholar]
- 22.Wedzicha JA, Bestall JC, Garrod R, Garnham R, Paul EA, Jones PW. Randomized controlled trial of pulmonary rehabilitation in severe chronic obstructive pulmonary disease patients, stratified with the MRC dyspnoea scale. Eur Respir J. 1998;12:363–9. doi: 10.1183/09031936.98.12020363. [DOI] [PubMed] [Google Scholar]
- 23.Güell R, Casan P, Belda J, Sangenis M, Morante F, Guyatt GH, et al. Long-term effects of outpatient rehabilitation of COPD: A randomized trial. Chest. 2000;117:976–83. doi: 10.1378/chest.117.4.976. [DOI] [PubMed] [Google Scholar]
- 24.Troosters T, Gosselink R, Decmer M. Short- and long-term effects of outpatient rehabilitation in patients with COPD: A randomized trial. Am J Med. 2000;109:207–12. doi: 10.1016/s0002-9343(00)00472-1. [DOI] [PubMed] [Google Scholar]
- 25.Lacasse Y, Brosseau L, Milne S, Martin S, Wong E, Guyatt GH, et al. Pulmonary rehabilitation for chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2002;(3):CD003793. doi: 10.1002/14651858.CD003793. [DOI] [PubMed] [Google Scholar]
- 26.Ries AL, Kaplan RM, Limberg TM, Prewitt LM. Effects of pulmonary rehabilitation on physiologic and psychosocial outcomes in patients with chronic obstructive pulmonary disease. Ann Intern Med. 1995;122:823–32. doi: 10.7326/0003-4819-122-11-199506010-00003. [DOI] [PubMed] [Google Scholar]
- 27.Guell R, Resqueti V, Sangenis M, Morante F, Martorell B, Casan P, et al. Impact of pulmonary rehabilitation on psychosocial morbidity in patients with severe COPD. Chest. 2006;129:899–904. doi: 10.1378/chest.129.4.899. [DOI] [PubMed] [Google Scholar]
- 28.Godoy RF, Teixeira PJ, Becker Júnior B, Michelli M, Godoy DV. Long-term repercussions of a pulmonary rehabilitation program on the indices of anxiety, depression, quality of life and physical performance in patients with COPD. J Bras Pneumol. 2009;35:129–36. doi: 10.1590/s1806-37132009000200005. [DOI] [PubMed] [Google Scholar]
- 29.Swigris JJ, Fairclough DL, Morrison M, Make B, Kozora E, Brown KK, et al. Beneficial effects of pulmonary rehabilitation in idiopathic pulmonary fibrosis. Respir Care. 2011;56:783–9. doi: 10.4187/respcare.00939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Markovitz GH, Cooper CB. Rehabilitation in non-COPD: Mechanisms of exercise limitation and pulmonary rehabilitation for patients with pulmonary fibrosis/restrictive lung disease. Chron Respir Dis. 2010;7:47–60. doi: 10.1177/1479972309348654. [DOI] [PubMed] [Google Scholar]
- 31.Ware LB. Clinical year in review I: Interstitial lung disease, pulmonary vascular disease, pulmonary infections, and cardiopulmonary exercise testing and pulmonary rehabilitation. Proc Am Thorac Soc. 2009;6:487–93. doi: 10.1513/pats.200907-057TT. [DOI] [PubMed] [Google Scholar]
- 32.Ferreira A, Garvey C, Connors GL, Hilling L, Rigler J, Farrell S, et al. Pulmonary rehabilitation in interstitial lung disease. Benefits and predictors of response. Chest. 2009;135:442–7. doi: 10.1378/chest.08-1458. [DOI] [PubMed] [Google Scholar]
- 33.Gupta K, Kumar R, Gaur SN. Effect of a domiciliary pulmonary rehabilitation programme on disability in patients with interstitial lung diseases. Indian J Chest Dis Allied Sci. 2007;49:213–17. [Google Scholar]
- 34.Ries AL. Pulmonary Rehabilitation: Summary of an evidence-based guideline. Respir Care. 2008;53:1203–7. [PubMed] [Google Scholar]
- 35.Nici L, Limberg T, Hilling L, Garvey C, Normandin EA, Reardon J, et al. Clinical competency guidelines for pulmonary rehabilitation professionals: American association of cardiovascular and pulmonary rehabilitation position statement. J Cardiopulm Rehabil Prev. 2007;27:355–8. doi: 10.1097/01.HCR.0000300261.62021.1b. [DOI] [PubMed] [Google Scholar]
- 36.Horowitz MB, Littenberg B, Mahler DA. Dyspnea ratings for prescribing exercise intensity in patients with COPD. Chest. 1996;109:1169–75. doi: 10.1378/chest.109.5.1169. [DOI] [PubMed] [Google Scholar]
- 37.ATS Committee on Proficiency Standards for Clinical Pulmonary Function Laboratories. ATS statement: Guidelines for the six-minute walk test. Am J Respir Crit Care Med. 2002;166:111–7. doi: 10.1164/ajrccm.166.1.at1102. [DOI] [PubMed] [Google Scholar]
- 38.Ries AL, Squier HC. The team concept in pulmonary rehabilitation. In: Fishman A, editor. Pulmonary rehabilitation. New York: Marcel Dekker; 1996. pp. 55–65. [Google Scholar]
- 39.Debigaré R, Maltais F. The major limitation to exercise performance in COPD is lower limb muscle dysfunction. J Appl Physiol. 2008;105:751–3. doi: 10.1152/japplphysiol.90336.2008a. [DOI] [PubMed] [Google Scholar]
- 40.Dolmage TE, Goldstein RS. Effects of one-legged exercise training of patients with COPD. Chest. 2008;133:370–6. doi: 10.1378/chest.07-1423. [DOI] [PubMed] [Google Scholar]
- 41.Subin, Rao V, Prem V, Sahoo Effect of upper limb, lower limb and combined training on health-related quality of life in COPD. Lung India. 2010;27:4–7. doi: 10.4103/0970-2113.59260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Maltais F, Hersfield ES, Stubbing D, Wijkstra P, Hatzoglou A, Loveridge B, et al. Exercise training in patients with COPD. In: Bourbeau J, editor. Chronic obstructive pumonary disease. London: BC Dekker Halminton; 2002. pp. 55–65. [Google Scholar]
- 43.Bernard S, Whittom F, Leblanc P, Jobin J, Belleau R, Bérubé C, et al. Aerobic and strength training in patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 1999;159:896–901. doi: 10.1164/ajrccm.159.3.9807034. [DOI] [PubMed] [Google Scholar]
- 44.Berry MJ, Adair NE, Sevensky KS, Quinby A, Lever HM. Inspiratory muscle training and whole-body reconditioning in chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 1996;153:1812–6. doi: 10.1164/ajrccm.153.6.8665039. [DOI] [PubMed] [Google Scholar]
- 45.Gosselink R, De Vos J, van den Heuvel SP, Segers J, Decramer M, Kwakkel G. Impact of inspiratory muscle training in patients with COPD: What is the evidence? Eur Respir J. 2011;37:416–25. doi: 10.1183/09031936.00031810. [DOI] [PubMed] [Google Scholar]
- 46.Dechman G, Wilson CR. Evidence underlying breathing retraining in people with stable chronic obstructive pulmonary disease. Phys Ther. 2004;84:1189–97. [PubMed] [Google Scholar]
- 47.Babu AS, Noone MS, Haneef M, Samuel P. The effects of ‘on-call/out of hours’ physical therapy in acute exacerbations of chronic obstructive pulmonary disease: A randomized controlled trial. Clin Rehabil. 2010;24:802–9. doi: 10.1177/0269215510367558. [DOI] [PubMed] [Google Scholar]
- 48.de Voogd JN, Wempe JB, Koëter GH, Postema K, van Sonderen E, Ranchor AV, et al. Depressive symptoms as predictors of mortality in Patients with COPD. Chest. 2009;135:619–25. doi: 10.1378/chest.08-0078. [DOI] [PubMed] [Google Scholar]
- 49.Kozora E, Tran ZV, Make B. Neurobehavioral improvement after brief rehabilitation in patients with chronic obstructive pulmonary disease. J Cardiopulm Rehabil. 2002;22:426–30. doi: 10.1097/00008483-200211000-00008. [DOI] [PubMed] [Google Scholar]
- 50.Debigaré R, Marquis K, Côté CH, Tremblay RR, Michaud A, LeBlanc P, et al. Catabolic/Anabolic balance and muscle wasting in patients with COPD. Chest. 2003;124:83–9. doi: 10.1378/chest.124.1.83. [DOI] [PubMed] [Google Scholar]
- 51.Soicher J, Dutton T, Bourbeau J. Program evaluation and outcome assessment. In: Bourbeau J, editor. Chronic obstructive pulmonary disease. London: BC Dekker Halminton; 2002. pp. 339–65. [Google Scholar]
- 52.Gross NJ. Chronic obstructive pulmonary disease outcome measurements: What's important? What's useful? Proc Am Thorac Soc. 2005;2:267–71. doi: 10.1513/pats.200504-036SR. [DOI] [PubMed] [Google Scholar]
- 53.Manali ED, Lyberopoulos P, Triantafillidou C, Kolilekas LF, Sotiropoulou C, Milic-Emili J, et al. MRC chronic dyspnea scale: Relationships with cardiopulmonary exercise testing and 6-minute walk test in idiopathic pulmonary fibrosis patients: A prospective study. BMC Pulm Med. 2010;10:32. doi: 10.1186/1471-2466-10-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Mador MJ, Rodis A, Magalang UJ. Reproducibility of Borg scale measurements of dyspnea during exercise in patients with COPD. Chest. 1995;107:1590–7. doi: 10.1378/chest.107.6.1590. [DOI] [PubMed] [Google Scholar]
- 55.Celli BR, Cote CG, Marin JM, Casanova C, Montes de Oca M, Mendez RA, et al. The body-mass index, airflow obstruction, dyspnea, and exercise capacity index in chronic obstructive pulmonary disease. N Engl J Med. 2004;350:1005–12. doi: 10.1056/NEJMoa021322. [DOI] [PubMed] [Google Scholar]
- 56.Raskin J, Spiegler P, McCusker C, ZuWallack R, Bernstein M, Busby J, et al. The effect of pulmonary rehabilitation on healthcare utilization in chronic obstructive pulmonary disease: The Northeast pulmonary rehabilitation consortium. J Cardiopulm Rehabil. 2006;26:231–6. doi: 10.1097/00008483-200607000-00006. [DOI] [PubMed] [Google Scholar]
- 57.Puhan MA, Scharplatz M, Troosters T, Steurer J. Respiratory rehabilitation after acute exacerbation of COPD may reduce risk for readmission and mortality: A systematic review. Respir Res. 2005;6:54. doi: 10.1186/1465-9921-6-54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.O’Donnell DE, Voduc N, Fitzpatrick M, Webb KA. Effect of salmeterol on the ventilatory response to exercise in COPD. Eur Respir J. 2004;24:86–94. doi: 10.1183/09031936.04.00072703. [DOI] [PubMed] [Google Scholar]
- 59.Maltais F, Hamilton A, Marciniuk D, Hernandez P, Sciurba FC, Richter K, et al. Improvements in symptom-limited exercise performance over 8 h with once-daily tiotropium in patients with COPD. Chest. 2005;128:1168–78. doi: 10.1378/chest.128.3.1168. [DOI] [PubMed] [Google Scholar]
- 60.O’Donnell DE, Lam M, Webb KA. Measurement of symptoms, lung hyperinflation, and endurance during exercise in chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 1998;158:1557–65. doi: 10.1164/ajrccm.158.5.9804004. [DOI] [PubMed] [Google Scholar]
- 61.O’Donnell DE, Lam M, Webb KA. Spirometric correlates of improvement in exercise performance after anticholinergic therapy in chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 1999;160:542–9. doi: 10.1164/ajrccm.160.2.9901038. [DOI] [PubMed] [Google Scholar]
- 62.Casaburi R, Kukafka D, Cooper CB, Witek TJ, Jr, Kesten S. Improvement in exercise tolerance with the combination of tiotropium and pulmonary rehabilitation in patients with COPD. Chest. 2005;127:809–17. doi: 10.1378/chest.127.3.809. [DOI] [PubMed] [Google Scholar]
- 63.Saey D, Debigare R, LeBlanc P, Mador MJ, Cote CH, Jobin J, et al. Contractile leg fatigue after cycle exercise: A factor limiting exercise in patients with COPD. Am J Respir Crit Care Med. 2003;168:425–30. doi: 10.1164/rccm.200208-856OC. [DOI] [PubMed] [Google Scholar]
- 64.Garrod R, Wedzicha J. Pulmonary rehabilitation: A multidisciplinary intervention. In: Pryor JA, editor. Physiotherapy for respiratory and cardiac problems. Edinburgh: Churchill Livingstone; 2001. pp. 471–91. [Google Scholar]
- 65.Fujimoto K, Matsuzawa Y, Yamaguchi S, Koizumi T, Kubo K. Benefits of oxygen on exercise performance and pulmonary hemodynamics in patients with COPD with mild hypoxemia. Chest. 2002;122:457–63. doi: 10.1378/chest.122.2.457. [DOI] [PubMed] [Google Scholar]
- 66.Emtner M, Porszasz J, Burns M, Somfay A, Casaburi R. Benefits of supplemental oxygen in exercise training in nonhypoxemic chronic obstructive pulmonary disease patients. Am J Respir Crit Care Med. 2003;168:1034–42. doi: 10.1164/rccm.200212-1525OC. [DOI] [PubMed] [Google Scholar]
- 67.Rooyackers JM, Dekhuijzen PN, Van Herwaarden CL, Folgering HT. Training with supplemental oxygen in patients with COPD and hypoxemia at peak exercise. Eur Respir J. 1997;10:1278–84. doi: 10.1183/09031936.97.10061278. [DOI] [PubMed] [Google Scholar]
- 68.Garrod R, Paul EA, Wedzicha JA. Supplemental oxygen during pulmonary rehabilitation in patients with COPD with exercise hypoxaemia. Thorax. 2000;55:539–3. doi: 10.1136/thorax.55.7.539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Wadell K, Henriksson-Larsen K, Lundgren R. Physical training with and without oxygen in patients with chronic obstructive pulmonary disease and exercise-induced hypoxaemia. J Rehabil Med. 2001;33:200–5. doi: 10.1080/165019701750419581. [DOI] [PubMed] [Google Scholar]
- 70.Zuwallack R. The nonpharmacologic treatment of chronic obstructive pulmonary disease advances in our understanding of pulmonary rehabilitation. Proc Am Thorac Soc. 2007;4:549–53. doi: 10.1513/pats.200701-015FM. [DOI] [PubMed] [Google Scholar]
- 71.Vivodtzev I, Pépin JL, Vottero G, Mayer V, Porsin B, Lévy P, et al. Improvement in quadriceps strength and dyspnea in daily tasks after 1 month of electrical stimulation in severely deconditioned and malnourished COPD. Chest. 2006;129:1540–8. doi: 10.1378/chest.129.6.1540. [DOI] [PubMed] [Google Scholar]
- 72.Eves ND, Sandmeyer LC, Wong EY, Jones LW, MacDonald GF, Ford GT, et al. Helium-Hyperoxia. A novel intervention to improve the benefits of pulmonary rehabilitation for patients with COPD. Chest. 2009;135:609–18. doi: 10.1378/chest.08-1517. [DOI] [PubMed] [Google Scholar]
- 73.Marciniuk DD, Butcher SJ, Reid JK, MacDonald GF, Eves ND, Clemens R, et al. The effects of helium-hyperoxia on 6-min walking distance in COPD: A randomized, controlled trial. Chest. 2007;131:1659–65. doi: 10.1378/chest.06-2514. [DOI] [PubMed] [Google Scholar]


