Abstract
Bronchopleural fistulas can occur from a number of causes (infective, traumatic, or neoplastic). Combined esophageal-pleural and bronchopleural fistula is not a common entity and previously has been reported after pneumonectomy. We describe the imaging findings and procedure of endoscopic glue injection in a case of combined esophageal-pleural and bronchopleural fistula after penetrating thoracic trauma. The treatment included esophageal exclusion for esophageal-pleural fistula, followed by endoscopic injection of glue for closure of bronchopleural fistula. The fistulae were completely sealed.
KEY WORDS: Bronchopleural fistula, bronchoscopy, therapy, trauma
INTRODUCTION
Bronchopleural fistula has a large number of etiologic factors (infective, traumatic, or neoplastic) and the even rarer esophageal-pleural fistula also has quite a large number of similar etiologies. Esophageal ruptures usually present with mediastinitis or mediastinal abscess and can rarely present with esophago-pleural fistula without any mediastinal abscess. The diagnosis of esophago-pleural fistula without any mediastinitis is often delayed and difficult. Bronchopleural fistula can be suspected on a plain radiograph and can be detected on CT scans. Small and peripheral fistulae can close spontaneously and often do not need any surgical intervention apart from the intercostals tube drainage. The larger or more proximal fistulae need surgical or endoscopic intervention. We describe the imaging findings and procedure of endoscopic glue injection in a case of combined esophageal-pleural and bronchopleural fistula after penetrating thoracic trauma.
CASE REPORT
A 40-year-old man came to the casualty with a thoracic bullet injury. At presentation, he had loss of power in both the lower limbs and dyspnea. The supine plain radiograph of the chest taken in the casualty revealed a bullet in the left hemithorax and diffuse-increased opacity of the left hemithorax. An axial CT scan of the dorsal spine revealed a fracture of the sixth dorsal vertebra with comminution of fragments and canal compromise (not shown). The bullet was seen to lie in the left pleural cavity and a left-sided pleural effusion was present. The patient was taken for orthopedic procedure including posterior fixation and retrieval of the bullet from the pleural cavity. Following the surgical procedures he was kept in intensive therapy unit where in the post-op days he was detected to have reduced air entry on the left side of the chest. Once oral feeding was started, leakage of food material through the intercostals tube was noted and an esophago-pleural communication was suspected. A contrast-enhanced computed tomography of the thorax was performed after giving oral iodinated nonionic contrast. Axial section of mediastinal window at the level of carina showed left hydropneumothorax and compression collapse of the left lung lower lobe. Orally administered iodinated contrast was seen to accumulate in the left pleural cavity, suggesting an esophago-pleural fistula. The iodinated contrast was seen to follow a long irregular track in the mediastinum communicating the mid-thoracic esophagus to the pleural cavity and running in close proximity to the left main bronchus [Figure 1]. Cervical esophagostomy, cervical esophageal exclusion, and feeding jejunostomy were performed as a therapeutic procedure. In the postoperative period he was detected to have a continued air leak and bronchoscopy was performed with the clinical diagnosis of a bronchopleural fistula. Bronchoscopy revealed a rent in the anterior wall of the left main bronchus (2 mm in diameter) [Figure 2]. Considering the general condition of the patient a bronchoscopic closure of the fistula was planned for. Under general anesthesia, using a 4 Fr angiographic catheter, 0.5 ml of N-butyl-cyanoacrylate glue (NECTACRYL, Dr. Reddy's Laboratories, Hyderabad, India) mixed with 0.5 ml of iodized oil (Lipiodol; Guerbet, Aulnay-sous-Bois, France) was injected in the fistulous tract [Figure 3]. Immediately after closure of fistula, the pneumothorax reduced. Follow-up imaging after 1 month revealed resolution of the hydropneumothorax and only small residual left lower lobe superior segment collapse. The glue was seen in the fistulous track to form a cast. A bronchoscopy done at this point of time revealed granulation tissue lining the mucosal aspect of the fistula, which had sealed. The contrast swallow study was normal and he was started on oral feed; esophagostomy and feeding jejunostomy were closed. The patient was discharged and kept on follow-up. Six-month follow-up imaging revealed complete resolution of the hydropneumothorax [Figure 4] and good expansion of the left lung.
Figure 1.

Axial CECT scan mediastinal window after oral contrast showing a contrast lined mediastinal track connecting the thoracic esophagus and the pleural cavity. The track lies in close relation to the left main bronchus
Figure 2.
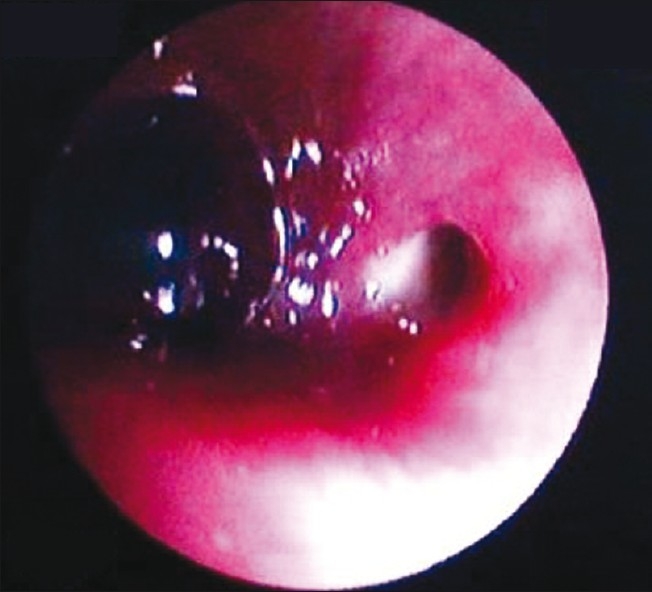
Bronchoscopic image at the level of carina showing the fistulous opening in the left main bronchus
Figure 3.
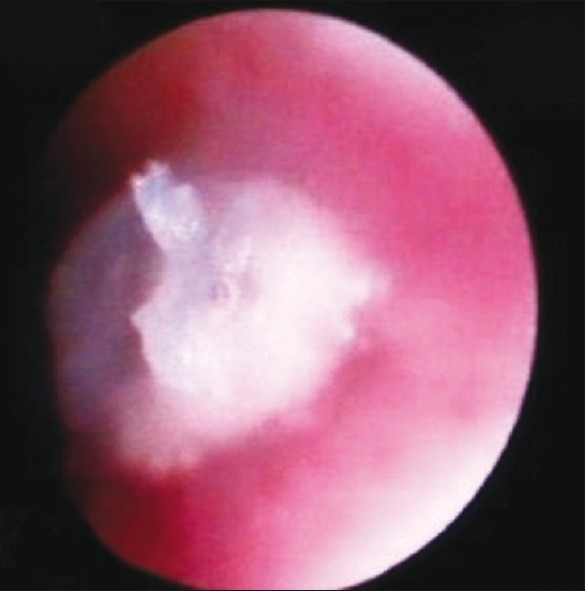
Bronchoscopic image showing the appearance of the tract after injection of the glue, the glue cast is seen to project into the bronchial lumen as a glistening white material
Figure 4.
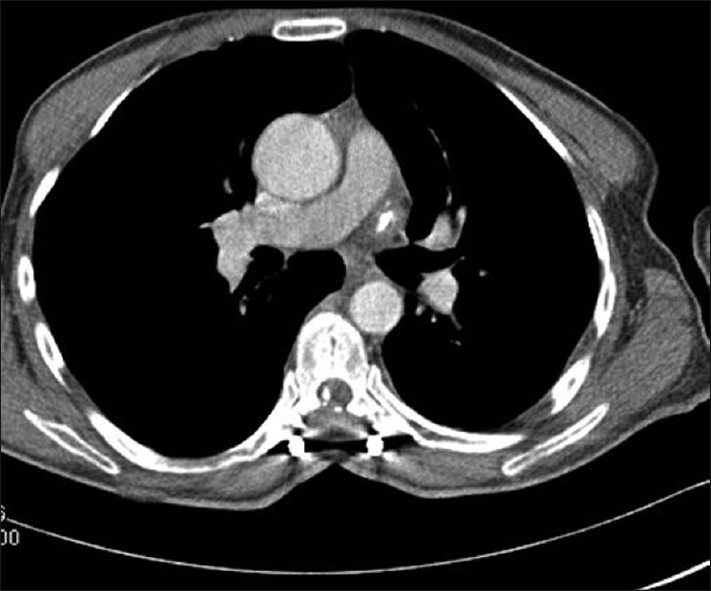
Axial CECT scan mediastinal window 6 months after glue injection revealed dense glue cast in the mediastinal fistulous track. There is complete expansion of the left lung and no hydropneumothorax
DISCUSSION
Bronchopleural fistula can arise as a result of infective etiology (rupture of a lung abscess, tuberculosis or fungal infection), traumatic (iatrogenic in the form of lung biopsy or chest tube insertion or accidental), by invasion by a malignancy or after pneumonectomy.[1] Bronchopleural fistula has an incidence of 2% in cases of lung resection and in up to 10% cases after pneumonectomy.[2] Esophageal-pleural fistula can occur as a result of iatrogenic trauma (following endoscopy), barotraumas, following empyema thoracis, in esophageal malignancies, tuberculosis.[3] The esophagus is closely related to the left pleura at the thoracic inlet,to the right pleural space below the level of the azygos arch, At the level of gastroesophageal junction, the esophagus is closely related to both the pleural surfaces. The possibility of a direct fistula and mediastinitis depends on the location of esophageal injury and also the amount of mediastinal fat.[4] CT is the usual investigative modality. Simultaneous esophago pleural and bronchopleural fistulae is a rare occurrence. To our knowledge, only one case has been reported in the English literature where the fistulae developed after pneumonectomy.[5] None has been described as a sequelae of trauma. The simultaneous presence of esophageal and bronchopleural fistula in our case was due to a long tract created by the path of the bullet in the mediastinum injuring the esophagus as well as the wall of the left main bronchus. The tract was well delineated by the CECT scan after oral contrast.
A chest radiograph can be a useful screening modality for a bronchopleural fistula; however, CT can demonstrate the site of fistula and can aid in surgical treatment by delineating the relation with the major airways.[5] Bronchoscopy helps delineating the extent of fistula. Traumatic bronchopleural fistulae (in penetrating trauma) if small and distal, can be managed conservatively with intercostal tube drainage. Those that do not resolve spontaneously can be treated via thoracoscopy using stapling devices and newer techniques such as intrapleural and intrabronchial administration of fibrin glue.[5] Blunt chest trauma usually results in main airway injury and does not lead to a pleural involvement. The surgical procedure for a large proximal fistula includes vascularized flap repair (muscle, omentum, diaphragm, or pericardium).
Endoscopic closure of a bronchopleural fistula has been attempted using a variety of materials[1] including fibrin, autologous blood clots,[6] doxycycline,[6] detachable balloons,[7] silicon rubber plugs, glue,[8,9] and metallic coils.[10] In 1977, Hartmann and Rausch[8] reported closure of a postoperative peripheral fistula after two bronchoscopic applications of methylcyanoacrylate. Harald et al.[9] occluded bronchopleural fistulas in two patients using tissue glue. Jain et al.[1] described an endobronchial closure of a chronic bronchopleural cutaneous fistula with glue and metallic coils delivered through angiography catheters under fluoroscopic guidance; performed under topical anesthesia.
Glue acts in two ways in the closure of fistula. Glue solidification of glue takes around 10 seconds when it comes in contact with the mucosa. Initially the glue closes the fistula by mechanical sealing; which is followed by inflammatory reaction and fibrosis which causes scarring and permanent fistula closure.[10] In our case the glue injected in the tract formed a cast soon after the injection and sealed the fistula immediately; evident by the immediate reduction of pneumothorax. In the course of time granulation tissue followed by fibrous tissue formed and the redundant part of glue cast lying within the bronchial lumen was shed off. Fibrosis and scarring of the track helped seal the mucosal opening of the fistula.
In conclusion, combined esophageal-pleural and bronchopleural fistula following penetrating trauma is a rare entity and the treatment included two-step approach; first closure of the esophageal fistula by esophageal exclusion followed by endoscopic injection of glue for closure of bronchopleural fistula. Endoscopic closure of fistula saved the patient from the morbidity associated from another thoracic surgery.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Jain R, Baijal SS, Phadke RV, Pandey CK, Saraswat VA. Endobronchial closure of a bronchopleural cutaneous fistula using angiography catheters. AJR Am J Roentgenol. 2000;175:1646–8. doi: 10.2214/ajr.175.6.1751646. [DOI] [PubMed] [Google Scholar]
- 2.Khan JH, Rahman SB, McEihinney DB, Harmon AL, Anthony JP, Hall TS, et al. Management strategies for complex bronchopleural fistula. Asian Cardiovasc Thorac Ann. 2000;8:78–84. [Google Scholar]
- 3.Giménez A, Franquet T, Erasmus JJ, Martínez S, Estrada P. Thoracic complications of Esophageal Disorders. Radio Graphics. 2002;22:S247–58. doi: 10.1148/radiographics.22.suppl_1.g02oc18s247. [DOI] [PubMed] [Google Scholar]
- 4.Wechsler RJ, Steiner RM, Goodman LR, Teplick SK, Mapp E, Laufer I. Iatrogenic esophageal-pleural fistula: Subtlety of diagnosis in the absence of mediastinitis. Radiology. 1982;144:239–43. doi: 10.1148/radiology.144.2.7089274. [DOI] [PubMed] [Google Scholar]
- 5.Trigui W, Le Pimpec-Barthes F, Shaker W, Lang-Lazdunski L, Riquet M. Simultaneous Bronchopleural and Esophagopleural Fistulas After Pneumonectomy. Ann Thorac Surg. 2002;74:923–4. doi: 10.1016/s0003-4975(02)03673-1. [DOI] [PubMed] [Google Scholar]
- 6.Lan RS, Lee CH, Tsai YH, Wang WJ, Chang CH. Fiberoptic bronchial blockade in a small bronchopleural fistula. Chest. 1987;92:944–6. doi: 10.1378/chest.92.5.944. [DOI] [PubMed] [Google Scholar]
- 7.Ellis JH, Sequeira FW, Weber TR, Eigen H, Fitzgerald JF. Balloon catheter occlusion of bronchopleural fistulae. AJR Am J Roentgenol. 1982;138:157–9. doi: 10.2214/ajr.138.1.157. [DOI] [PubMed] [Google Scholar]
- 8.Hartmann W, Rausch V. New therapeutic application of the fiberoptic bronchoscope. Chest. 1977;71:237. doi: 10.1378/chest.71.2.237a. [DOI] [PubMed] [Google Scholar]
- 9.Roksvaag H, Skalleberg L, Nordberg C, Solheim K, Hoivik B. Endoscopic closure of bronchial fistula. Thorax. 1983;38:696–7. doi: 10.1136/thx.38.9.696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Salmon CJ, Ponn RB, Westcott JL. Endobronchial vascular occlusion coils for control of a large parenchymal bronchopleural fistula. Chest. 1990;98:233–4. doi: 10.1378/chest.98.1.233. [DOI] [PubMed] [Google Scholar]


