Abstract
Two clinical cases of aspiration are reported in elderly ladies with differing presentations following inhalation of the same brand of calcium tablet. One of the patients distinctly recalled the choking episode, whereas the other failed to do so making the diagnosis of aspiration difficult. One of the aspirated tablets was successfully retrieved during rigid bronchoscopy after the patient reported several months of cough requiring multiple courses of antibiotics. The other aspirated tablet was coughed up by the patient after the successful treatment of a pneumonia complicated by a parapneumonic effusion.
KEY WORDS: Calcium tablets, foreign body aspiration, right-sided lung pathology
INTRODUCTION
Foreign body aspiration (FBA) is the most common cause of intra-luminal airway abnormalities in children.[1] However, FBA is unusual in adults and is often overlooked as a cause of airway obstruction.[2] Diagnosis of FBA can be difficult especially if the patient forgets the aspiration episode. FBA has variable clinical manifestations, ranging from trivial symptoms to irreversible lung damage and life-threatening infection and massive hemoptysis.[3] Chronic cases of aspiration may be difficult to diagnose radiologically. Radiographic findings of aspiration include lobar or segmental collapse, recurrent pneumonia, bronchiectasis and an endobronchial mass. A chronic inflammatory reaction with granulation tissue formation around the inhaled foreign body may mimic bronchogenic carcinoma.[2]
We report two cases of accidental aspiration of the same brand of calcium tablet manifesting in different ways.
CASE REPORT
Case 1
A 62-year-old non-smoking woman presented with a one-week history of cough, yellowish sputum, fever of 38.3°C and right-sided pleuritic chest pain. She also gave a four-month history of dyspnoea and reported a weight loss of 8 Kgs. Her past medical history was notable for invasive ductal right breast adenocarcinoma, 14 months prior treated with right mastectomy, axillary lymph node resection and radiotherapy. Chest radiography [Figure 1] performed before five months was normal. She was also hypercholesterolemic and osteoporotic, and treated with simvastatin, calcium carbonate and sodium alendronate.
Figure 1.
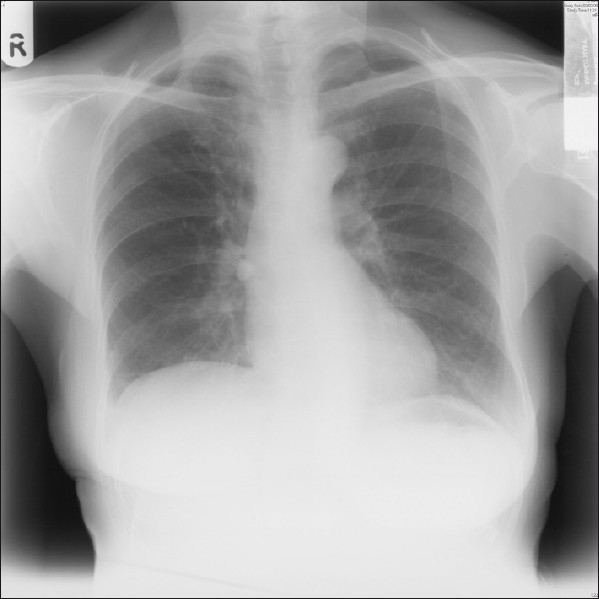
Chest radiograph initially was reported as normal, however on careful inspection a small round opacity is visible at the level of the right hilum
Respiratory examination revealed evidence of a small right-sided pleural effusion. Rest of the examination was normal apart from the mastectomy scar.
Blood investigations showed an elevated white blood cell count (WBC) of 16.28 X109/L, hemoglobin of 10.6 g/dl, platelets of 342,000, and ESR of 92 mm. Liver function tests showed minimal elevation of alanine transaminase and gamma glutamyltransferase. Serum calcium was normal.
Chest radiography was carried out on admission [Figure 2]. A diagnostic right thoracocentesis yielded hemorrhagic fluid. Biochemistry of the pleural fluid revealed: Protein of 45.8 g/dL, albumin of 22.4 g/dL and lactic dehydrogenase of 1,610 U/L (normal <200 U/L). Cytology was negative for malignant cells. Pleural fluid cultures were negative for bacterial growth.
Figure 2.
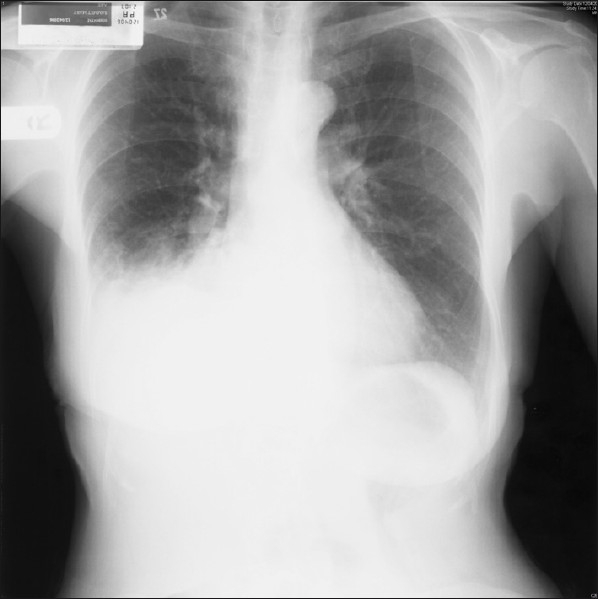
Chest radiograph at presentation showed a right lower zone consolidation associated with a pleural effusion
A diagnosis of right lower lobe pneumonia and a parapneumonic effusion was made following initial evaluation. The patient was started on intravenous cefuroxime axetil 750 mg three times daily and oral clarithromycin 500 mg twice daily. However, due to lack of improvement after three days of therapy, her antibiotic regime was changed to intravenous piperacillin sodium-tazobactam 4.5 g three times daily. The patient's clinical condition improved within 24 hours and the effusion resolved after 14 days of antibiotic treatment.
At the four-week follow-up visit, the patient brought along with a whole tablet of calcium carbonate that she had coughed prior to the visit. On further questioning, she recalled an accident during which she had choked on the tablet several months before. A follow-up CT scan of thorax ten weeks after her hospitalization was normal.
Case 2
A 74-year-old woman was admitted with recurrent episodes of fever associated with non-purulent productive cough of a few months duration. The patient recalled choking on a calcium tablet five months before. She had been prescribed several antibiotic courses by her general practitioner. Clinical examination revealed fever of 38°C, decreased air entry over the right lung base and a monophonic wheeze over the right mid-chest zone. A chest radiograph and a CT scan of thorax showed a tablet lodged in the right lower lobe bronchus and right lower lung segmental consolidation.
The patient was started on intravenous clindamycin 450 mg six hourly, ciprofloxacin 200 mg twice daily and meropenem 1 g three times daily and intensive chest physiotherapy. After eight days of admission she underwent flexible bronchoscopy. The right lower lobe bronchus was occluded with a hard, whitish mass surrounded by erythematous mucosa and granulation tissue. This was consistent with the calcium tablet aspirated a few months previously. A rigid bronchoscopy thereafter showed granulation tissue over the embedded foreign body. A second attempt at rigid bronchoscopy successfully retrieved and removed fragments of the calcium tablet and allowed visualization of the right lower lobe bronchi.
The patient was discharged home and followed up with no further complications. Follow-up chest radiograph showed residual bronchiectatic changes in the right lower lobe.
DISCUSSION
These two cases demonstrate aspiration episodes in elderly patients from the same brand of calcium tablet prescribed for osteoporosis. Both patients demonstrated right-sided chest abnormalities, however both cases were different. One of the patients clearly recalled choking on her tablet, whereas the other failed to recall the aspiration episode making the diagnosis of FBA more difficult. The other difference was that while one coughed up her tablet some months after aspiration, the other did not due to local impaction of the calcium tablet.
FBA is uncommon in adults and poses a diagnostic challenge to the respiratory physician. A detailed history as well as entertaining a high index of suspicion is necessary in arriving at the correct diagnosis of aspiration. This can be associated with significant morbidity.[4] FBA in adults is most common in the seventh decade.[5] FBA is usually associated with conditions causing abnormalities in upper airway protective mechanisms, poor dentition, dental procedures, mental retardation, neurological disorders, impaired level of consciousness, alcohol and sedative abuse.[4] Less commonly, laughing or sneezing may also predispose to FBA. Up to two thirds of foreign bodies passing through the vocal cords lodge at the carina or the right main bronchus (due to its more vertical orientation and slightly larger diameter) but smaller ones may reach more distal airways.[5]
The symptoms and signs of FBA depend on the site, size, composition and period for which the foreign body has been lodged. Most cases of aspiration are associated with food items especially vegetable matter.[6] However, aspiration of toxic foreign bodies and tablets can lead to local airway inflammation. Several cases of toxic FBA are reported from aspiration of ferrous sulphate,[7] aspirin, bismuth, tetracycline,[8] phenobarbitone and charcoal. Plastic or enteric coated capsules are more ‘inert’ causing fewer complications. Complications of tablet aspiration range from haemoptysis, bronchiectasis, recurrent pneumonia, lung abscess, empyema, bronchiolitis obliterans, pneumothorax, pneumomediastinum, middle lobe syndrome to bronchial necrosis, bronchial stenosis, fatal pneumonia and respiratory failure.[9]
A chest radiograph taken in expiration is helpful in the diagnosis of a radio-opaque foreign body. The chest radiograph can be normal in up to 25% of cases. Radiolucent foreign bodies may be associated with lobar pneumonia, atelectasis, compensatory emphysema or air trapping in partial bronchial obstruction. The rigid bronchoscope remains the ideal instrument for retrieval of large foreign bodies from the main bronchi as this technique ensures better access, oxygen delivery and easy passage of grasping forceps. Flexible bronchoscopy is useful in the diagnosis and the retrieval of smaller foreign bodies in the peripheral smaller bronchi.[10] Neglected cases of FBA may require surgical intervention.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Marom EM, McAdams HP, Erasmus JJ, Goodman PC. The many faces of pulmonary aspiration. AJR Am J Roentgenol. 1999;172:121–8. doi: 10.2214/ajr.172.1.9888751. [DOI] [PubMed] [Google Scholar]
- 2.Nigam BK. Bronchial foreign body masquerading as a lung carcinoma. Indian J Chest Dis Allied Sci. 1990;32:43–7. [PubMed] [Google Scholar]
- 3.Pattison CW, Leaming AJ, Towsend ER. Hidden foreign body as a cause of recurrent haemoptysis in a teenage girl. Ann Thorac Surg. 1988;45:330–1. doi: 10.1016/s0003-4975(10)62475-7. [DOI] [PubMed] [Google Scholar]
- 4.Zubairi AB, Haque AS, Husain SJ, Khan JA. Foreign body aspiration in adults. Singapore Med J. 2006;47:415–8. [PubMed] [Google Scholar]
- 5.Limper AH, Prakash UB. Tacheobronchial foreign bodies in adults. Ann Intern Med. 1990;112:604–9. doi: 10.7326/0003-4819-112-8-604. [DOI] [PubMed] [Google Scholar]
- 6.Lin YS, Chu NF, Wu DM, Shen MH. Prevalence and factors associated with the consumption of betel nut among military conscripts in Taiwan. Eur J Epidemiol. 2004;19:343–51. doi: 10.1023/b:ejep.0000024695.87008.ff. [DOI] [PubMed] [Google Scholar]
- 7.Lamaze R, Trechot P, Martinet Y. Bronchial necrosis and granuloma formation induced by the aspiration of a tablet of ferrous sulphate. Eur Respir J. 1994;7:1710–1. doi: 10.1183/09031936.94.07091710. [DOI] [PubMed] [Google Scholar]
- 8.Sundar KM, Elliott CG, Thomsen GE. Case Report tetracycline aspiration. Respiration. 2001;68:416–9. doi: 10.1159/000050538. [DOI] [PubMed] [Google Scholar]
- 9.Jager D, Muller KM, Gillissen A, Schultze-Werninghaus G. Cough, dyspnoea and purulent sputum in a 66-year-old non-smoking female. Eur Respir J. 1999;13:456–9. doi: 10.1183/09031936.99.13245699. [DOI] [PubMed] [Google Scholar]
- 10.Rafanan AL, Hehta AC. Adult airway foreign body removal. Clin Chest Med. 2001;22:319–30. doi: 10.1016/s0272-5231(05)70046-0. [DOI] [PubMed] [Google Scholar]


