Abstract
Background:
Self-medication is widely practiced in the study area, as many drugs are available over-the-counter, in addition to the use of local herbal preparations. Also, apprehension about the dangers of drug use in pregnancy appears to affect the compliance of prescribed medication. This study assess the drug use profile of an antenatal population.
Materials and Methods:
This was a questionnaire-based descriptive study of 410 antenatal clients attending primary, secondary and tertiary centers in Ibadan, Nigeria. The variables analysed were demographic data of respondents and level of health care received. Outcome measures were use of prescribed drugs, self-medication or herbal preparations. Chi-tests and logistic regression were used for statistical analysis.
Results:
All patients on prescribed medication for medical conditions claimed to be compliant with their drugs. Exactly 19.2% admitted to self-medication, mostly hematinics and pain-relieving pills (acetaminophen). No one admitted to alcohol or tobacco use, but 46.3%, especially attendees of the rural center (OR 5.79; 95% CI 2.56-13.10), ingested herbal concoctions while pregnant. Married women (OR 0.2; 95% CI 0.05-0.75) or those whose spouses had higher education (OR 0.43; 95% CI 0.21-0.89) were less likely to practice self-medication, while hypertensive women were more likely to practice it (OR 22.54; 95% CI 3.81-133.49).
Conclusions:
Social support has a role in safe drug use practices. This should be used to advantage by encouraging partners’ attendance at antenatal sessions. Patients need counseling on the dangers of procuring their usual prescription drugs without consultation. Use of herbal concoctions needs to be explored in the community.
Keywords: Compliance, herbs, self-medication, social support
INTRODUCTION
Women are generally educated to avoid drug use during pregnancy due to the perceived aftermath effect to the developing foetus. Few drugs have been studied in pregnancy and even fewer have undergone prospective follow-up in the child after its birth to evaluate long-term effects, due to the ethical considerations of studying a vulnerable group. Health care providers weigh the benefit of the drug to the woman against the risk to the fetus before prescribing medication. A study from Turkey found that 80% of women had used drugs during their first trimester.1 Over-the-counter availability of many drugs (including prescription drugs) in environments like ours, where legal restrictions are few, makes the risk of ingesting harmful drugs even greater. Further contributing to this is the proliferation of native herbal medicaments, many of which claim to have multifaceted potency in pregnancy. The ingredients (active or otherwise) of most of them are not known, neither is their level of refinement.
Akanbi et al.2 studied self-medication pattern of antimalarial drugs. They reported that most of their participants had used chloroquine and pyrimethamine before their first antenatal visit. This may have its advantages, as shown by their reduced parasite density; yet, pyrimethamine is an anti-folate drug with expected teratogenic potential. The authors did not discuss the gestational age of these women; their fetuses may have been at risk if they had ingested this drug during the period of organogenesis. Others studied the patterns of drug use in pregnancy and found that the commonest drug used was folic acid, followed by antimalarials;3 only 4% used drugs without a prescription, 12% used native herbs and less than 1% smoked.
However, some drugs are beneficial in pregnancy and withholding them poses several risks. These include routine hematinics and malaria prophylaxis, as well as specific drugs for medical illnesses complicating pregnancy. A study on hypertension showed that therapy during pregnancy significantly reduced maternal and perinatal morbidity and mortality, including pre-eclampsia, eclampsia and abruptio placenta.4 The Federal Ministry of Health of Nigeria recommends intermittent preventive treatment (IPT) of malaria5 and local studies have shown its effectiveness.6,7 The compliance to these prescribed drugs may be poor, as a paradoxical outcome of health talks and awareness campaigns against drug use in pregnancy.
Focus group discussions in a rural community revealed that some women do not use hematinics, fearing that it would make the baby big or result in excessive blood, and therefore excessive blood loss at delivery.8 Another study about IPT with sulfadoxine-pyrimethamine9 reported concerns expressed about its effect on pregnancy-though it was dispensed at their antenatal clinic-and some did not use the drug on account of this.
The aim of this study is to document the drug use profile of antenatal clients in Ibadan, Nigeria, including assessment of prescribed drug compliance and self-medication.
MATERIALS AND METHODS
It was a cross-sectional, descriptive study. Four hundred and ten pregnant women, attending antenatal clinic at three levels of care (primary, secondary and tertiary) in Yoruba-speaking Ibadan, the largest city in Nigeria, were recruited in the study. These centers serve rural, semi-urban and urban populations, respectively, and are all public, government-owned facilities. The primary and secondary centers offer free medical health care; however, apart from routine antenatal medication, all drugs are usually prescribed for the patients to procure for themselves as they are usually not stocked. Patients pay for all their care at the tertiary center (except, again, the routine antenatal drugs which are considered as part of the antenatal care which has been paid for), with the exception of those who subscribe to the National Health Insurance Scheme. A total sampling of all consenting clients who attended antenatal clinic in January 2009 was done.
A self-administered questionnaire with open- and close-ended questions was employed to elicit respondents’ demographic data, associated medical conditions and their drug compliance and self-medication practices. They were asked to check drugs they had used from a list that included routine drugs (hematinics and anti-malarial drugs), tobacco, alcohol and herbal preparations. Then, we asked them to specify “others”. Explanatory data included clients’ demographic data, their highest educational attainment and the level at which the clients receive health care. Outcome variables were the use of self-medication, compliance to prescribed medication and ingestion of herbal concoctions.
Chi-test and Fisher's exact test were used at 95% confidence level to evaluate the data obtained, with Stata-8 software. Level of significance was set at P<0.05. Multivariate analysis was performed by logistic regression.
RESULTS
The average age of the respondents was 29.0 ± 5.3 years. The average gestational age of commencement of antenatal care was 19.7 ± 13.0 weeks: only 74 (18.0%) registered in the first trimester, while 259 (63.3%) and 77 (18.7%) registered in the second and third trimesters, respectively. The mean gestational age of the subjects at the time of recruitment was 29.7 ± 6.4 weeks. Forty-two of the respondents had been diagnosed of medical conditions; these included hypertension in 10 (2.5%), diabetes mellitus in 4 (1%), renal disease in 1 (0.2%), asthma in 2 (0.5%), epilepsy in 2 (0.5%), and psychiatric disorders in 7 (1.8%) amongst others (16; 3.9%). Eight (19.0%) respondents were on medication for these conditions, but 2 (4.8%) of them were not sure. All claimed that they were compliant with prescribed drugs.
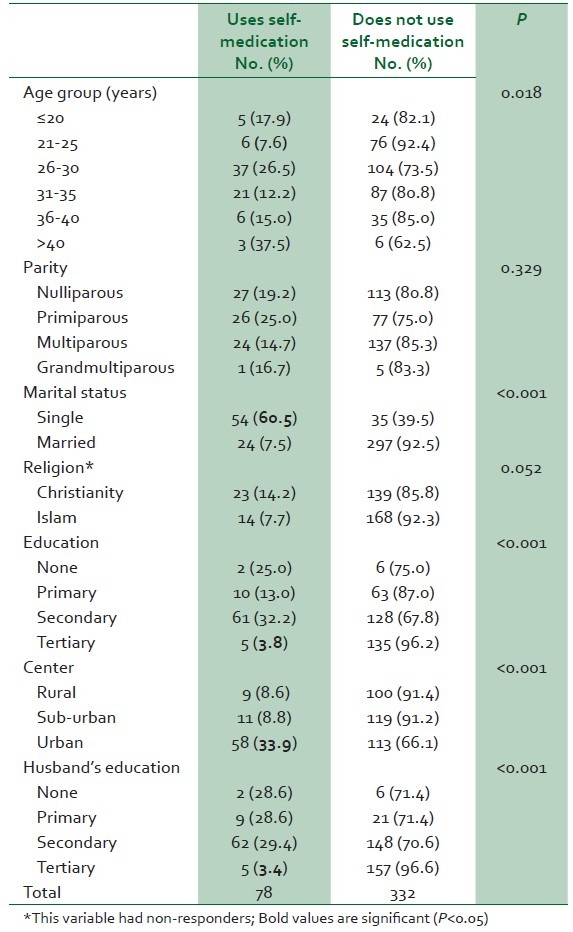
Self-medication was practiced by 78 (19.0%) respondents; Table 1 shows their demographic characteristics. Single (women who were not married, including those who were widowed, separated or divorced) and those attending the urban center were more likely to practice self-medication, while younger women, those with higher education (or who had spouses with higher education) were less likely to practice it.
Table 1.
Association between demographic characteristics of respondents and use of self-medication
Hematinics were the most commonly used conventional drugs in pregnancy (283; 69%), followed by acetaminophen (196; 48%). Twenty-five (6%) each used anti-malarial medication, vitamin C and metronidazole. Four respondents (1%) used calcium supplements. No one admitted to using alcohol or tobacco, but 190 respondents (46.3%) had ingested herbal concoctions in pregnancy.
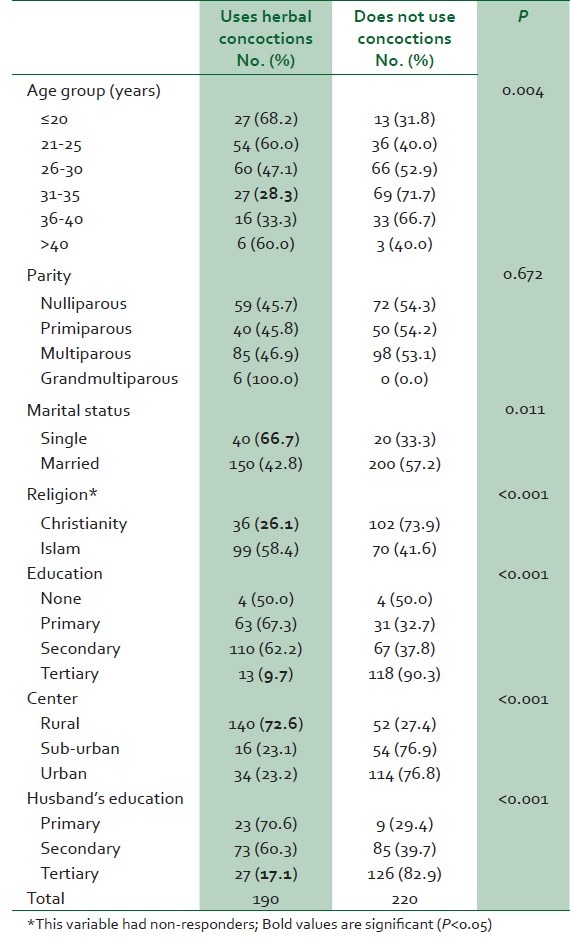
Table 2 shows that unmarried women and attendees of the rural center were more likely to use herbal concoctions, while women who (or whose spouses) had better education were less likely to use them.
Table 2.
Association between demographic characteristics of respondents and ingestion of herbal concoction
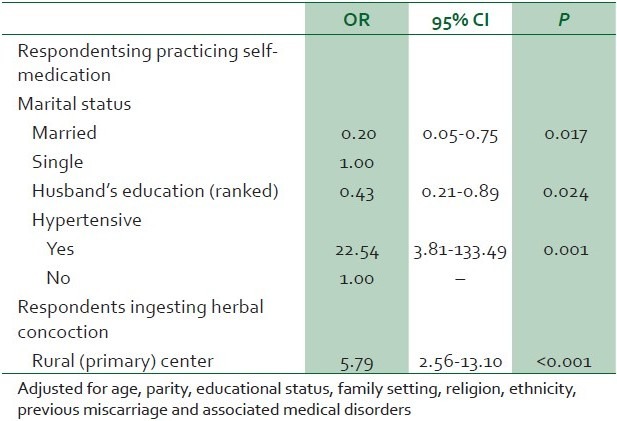
Logistic regression analysis [Table 3] confirmed that married women (OR 0.2; 95% CI 0.05-0.75) and those whose spouses had higher education (OR 0.43; 95% CI 0.21-0.89) were significantly less likely to use self-medication, while women who were hypertensive (OR 22.54; 95% CI 3.81-133.49) were much more likely to use it. Attendees of the rural center were more likely to use herbal concoctions (OR 5.79; 95% CI 2.56-13.10).
Table 3.
Significant associations of drug use behavior on multivariate analysis
DISCUSSION
All patients with associated medical illnesses claimed compliance to prescribed drugs, but as the drugs were not dispensed as direct observation therapy, it was difficult to ascertain. It is also possible that those who stated they were not on medication actually had medication prescribed for them by their healthcare providers, but were not being compliant. Only a proportion of respondents listed hematinics and anti-malarial medication amongst the drugs they used in pregnancy. These drugs are routinely prescribed and dispensed free (subject to availability) at all the study centers, thus giving a fair assessment of unsatisfactory drug compliance in pregnancy. The low level of anti-malarial drug use is particularly noteworthy. It may be assumed that they either did not use the prescribed intermittent preventive treatment for malaria, or they might not have been counseled before it was prescribed, and therefore did not know it was for malaria. The literature is replete with explanations for poor compliance with routine antenatal drugs.8–10 Also, almost a fifth of the respondents booked in the third trimester, when it might be too late to offer sulphadoxine-pyrimethamine; this may also be partly responsible for low usage.
As mentioned earlier, self-medication is very easy due to poor restriction policy on drug availability. About one-fifth of patients admitted that they indulged in this. Most of the drugs volunteered are relatively safe in pregnancy. The prevalent use of acetaminophen is not unexpected, as it is one of the few analgesics that are safe in pregnancy. As it is easily available, a client for whom it has been prescribed before will procure it again rather than come to queue up in an emergency room to be treated. Metronidazole (“Flagyl”, as our respondents stated) is used in the treatment of amebic dysentery, but is often abused in this environment (often by self-medication) as a treatment for diarrhea. The manufacturer recommends avoidance of high-dose regimens in pregnancy.11
Multivariate analysis revealed that married women were less likely to use self-medication. Social support has been shown to improve outcome and satisfaction of pregnancy,12 delivery,13 initiation14 and duration15 of breastfeeding and utilization of family planning methods.16 It can be argued that social support from a partner may also account for the avoidance of indiscriminate drug use in pregnancy, as the woman is likely to be influenced appropriately and also distracted from the minor disorders of pregnancy that mostly predispose to drug use. This is supported by the fact that those married to higher-educated men were less likely to use self-medication. These partners are likely to be better enlightened to the dangers of indiscriminate drug use and thus influence the women's behavior.
It is unclear why hypertensive women were significantly more likely to use self-medication. It is possible that they chose to procure drugs that had been prescribed to them in the past, rather than visit their health care facility. Health-seeking behavior is known to be poor in this environment, especially due to the high cost of health care, as well as delay and frequent disruption of services at most public facilities.17,18 None of the patients used social drugs (alcohol and tobacco) during pregnancy. This is satisfactory, but not unexpected, as women do not commonly use these substances in the study area.19 A study in mid-West Nigeria found that less than 1% smoked tobacco.3
Despite regular health talks on the subject at all these centers, almost half of the respondents use herbal concoctions. This prevalent use was also found in a study by Fakeye et al.20 in 2009, and to a lesser extent by Gharoro and Igbafe.3 It may be a reflection of the community, as attending the rural center was significantly associated with herbal use. It is not all of our antenatal attendees that deliver in the facility they registered at.21 Some go to traditional birth attendants (TBAs) where herbal concoctions are employed22 or to religious birthing homes. But whether they are prescribed by TBAs or the use is initiated by self, it is apparent that there is a high level of confidence in the efficacy and safety of these drugs on the part of the respondents. Fakeye et al.20 showed that reasons proffered for taking herbal medications included perceived better safety (being natural) and efficacy than conventional medications, easier access and lower cost of herbs, as well as cultural belief in its ability to cure many illnesses. Many of them did not combine them with conventional drugs to forestall drug-herb interaction, thus depriving them of the benefits of prescribed medication. It will be useful to hold focus group discussions in the community to ascertain what these concoctions are, what function they are supposed to perform, and adverse effects that have been identified from these preparations. This may inform the directed health education that is clearly needed on the matter.
The onus lies on health care providers to inform patients about the drugs they are using, their function and possible adverse effects so that they can use the drugs safely and have a reasonable index of suspicion of arising complications. The place of social support is also apparent in safe drug use practice. This should be explored to an advantage, encouraging partners to attend antenatal sessions with their wives so that they learn about the pregnancy together and can reinforce safe practices as taught in these sessions.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Basgul A, Akici A, Uzuner A, Kalaça S, Kavak ZN, Tural A, et al. Drug utilization and teratogenicity risk categories during pregnancy. Adv Ther. 2007;24:68–80. doi: 10.1007/BF02849994. [DOI] [PubMed] [Google Scholar]
- 2.Akanbi OM, Odaibo AB, Afolabi KA, Ademowo OG. Effect of self-medication with antimalarial drugs on malaria infection in pregnant women in south-western Nigeria. Med Princ Pract. 2005;14:6–9. doi: 10.1159/000081915. [DOI] [PubMed] [Google Scholar]
- 3.Gharoro EP, Igbafe AA. Pattern of drug use amongst antenatal patients in Benin City, Nigeria. Med Sci Monit. 2000;6:84–7. [PubMed] [Google Scholar]
- 4.Jahic M, Jahic E, Nurkic M, Nurkic J. Hypertension in pregnancy. Med Arh. 2008;62:169–71. [PubMed] [Google Scholar]
- 5.National guidelines and strategies for malaria prevention and control during pregnancy. Abuja: Federal Ministry of Health Nigeria. 2005:1–50. [Google Scholar]
- 6.Falade CO, Yusuf OB, Fadero FF, Mokuolu OA, Hamer DH, Salako LA. Intermittent preventive treatment with sulphadoxine-pyrimethamine is effective in preventing maternal and placental malaria in Ibadan, south-western Nigeria. Malar J. 2007;6:88. doi: 10.1186/1475-2875-6-88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tukur IU, Thacher TD, Sagay AS, Madaki JK. A comparison of sulfadoxine-pyrimethamine with chloroquine and pyrimethamine for prevention of malaria in pregnant Nigerian women. Am J Trop Med Hyg. 2007;76:1019–23. [PubMed] [Google Scholar]
- 8.Ejidokun OO. Community attitudes to pregnancy, anaemia, iron and folate supplementation in urban and rural Lagos, south-western Nigeria. Midwifery. 2000;16:89–95. doi: 10.1054/midw.1999.0196. [DOI] [PubMed] [Google Scholar]
- 9.Akinleye SO, Falade CO, Ajayi IO. Knowledge and utilization of intermittent preventive treatment for malaria among pregnant women attending antenatal clinics in primary health care centers in rural southwest, Nigeria: A cross-sectional study. BMC Pregnancy Childbirth. 2009;9:28. doi: 10.1186/1471-2393-9-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Asa OO, Onayade AA, Fatusi AO, Ijadunola KT, Abiona TC. Efficacy of intermittent preventive treatment of malaria with sulphadoxine-pyrimethamine in preventing anaemia in pregnancy among Nigerian women. Matern Child Health J. 2008;12:692–8. doi: 10.1007/s10995-008-0319-3. [DOI] [PubMed] [Google Scholar]
- 11.British National Formulary. [Last accessed on 2010 Jul 17];2010 59 Available from: http://bnf.org/bnf/bnf/current/3932.htm . [Google Scholar]
- 12.Olayemi O, Bello FA, Aimakhu CO, Obajimi GO, Adekunle AO. Male participation in pregnancy and delivery in Nigeria: A survey of antenatal attendees. J Biosoc Sci. 2009;41:493–503. doi: 10.1017/S0021932009003356. [DOI] [PubMed] [Google Scholar]
- 13.Morhason-Bello IO, Adedokun BO, Ojengbede OA, Olayemi O, Oladokun A, Fabamwo AO. Assessment of the effect of psychosocial support during childbirth in Ibadan, south-west Nigeria: A randomised controlled trial. Aust N Z J Obstet Gynaecol. 2009;49:145–50. doi: 10.1111/j.1479-828X.2009.00983.x. [DOI] [PubMed] [Google Scholar]
- 14.Morhason-Bello IO, Adedokun BO, Ojengbede OA. Social support during childbirth as a catalyst for early breastfeeding initiation for first-time Nigerian mothers. Int Breastfeed J. 2009;4:16. doi: 10.1186/1746-4358-4-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Olayemi O, Aimakhu CO, Bello FA, Motayo VO, Ogunleye AA, Odunukan OW, et al. The influence of social support on the duration of breast-feeding among antenatal patients in Ibadan. J Obstet Gynaecol. 2007;27:802–5. doi: 10.1080/01443610701666876. [DOI] [PubMed] [Google Scholar]
- 16.Ojengbede OA, Morhason-Bello IO, Adedokun BO, Becker S, Oni G, Tsui A. Husbands’ support during childbirth as a catalyst for modern family planning uptake in Nigeria: A randomised controlled trial. Uganda: International Family Planning Conference proceedings. 2009. Nov 17-19, [Last accessed on 2010 Sep 1]. Available from: http://www.fpconference2009.org/media//DIR_169701/d7df454c660c706cffff8089ffffd502.pdf .
- 17.Osubor KM, Fatusi AO, Chiwuzie JC. Maternal health-seeking behavior and associated factors in a rural Nigerian community. Matern Child Health J. 2006;10:159–69. doi: 10.1007/s10995-005-0037-z. [DOI] [PubMed] [Google Scholar]
- 18.Tinuade O, Iyabo RA, Durotoye O. Health-care-seeking behaviour for childhood illnesses in a resource-poor setting. J Paediatr Child Health. 2010;46:238–42. doi: 10.1111/j.1440-1754.2009.01677.x. [DOI] [PubMed] [Google Scholar]
- 19.Obionu CN. Implications of inadequate recording of alcohol-drinking and tobacco-smoking habits of patients. Postgrad Med J. 1998;5:92–3. [Google Scholar]
- 20.Fakeye TO, Adisa R, Musa IE. Attitude and use of herbal medicines among pregnant women in Nigeria. BMC Complement Altern Med. 2009;9:53. doi: 10.1186/1472-6882-9-53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.In: National Population Commission (NPC) [Nigeria] and ICF Macro. Nigeria Demographic and Health Survey 2008. Abuja, Nigeria: National Population Commission and ICF Macro; 2009. Maternal Health and Obstetric Fistula. [Google Scholar]
- 22.Ahmed OA, Odunukwe NN, Akinwale OP, Raheem TY, Efienemokwu CE, Ogedengbe O, et al. Knowledge and practices of traditional birth attendants in prenatal services in Lagos State, Nigeria. Afr J Med Med Sci. 2005;34:55–8. [PubMed] [Google Scholar]


