Background
Many arguments are favouring a renewed interest in vitamin D physiology, with a consequent increase in the number of scientific publications and media reports (1). Not surprisingly, TIME magazine nominated vitamin D as one of the “top medical breakthroughs” in the December issue of 2007. This vigorous increase of interest in vitamin D is powered by the spectacular insights into the pivotal regulatory role of vitamin D with regard to pleiotropic functions, by the data on worldwide trend to nutritional vitamin insufficiency (2) and by new knowledge on intracrine and paracrine actions of vitamin D metabolites (3).
Despite the fact that vitamin D is still called and known as a vitamin, it actually comprises a group of very closely interrelated hormonal compounds also related to the other main calciotropic hormone, the parathyroid hormone. Therefore, vitamin D is now viewed from a controller of calcium homeostasis (calciotropic) to an hormone with pleiotropic actions.
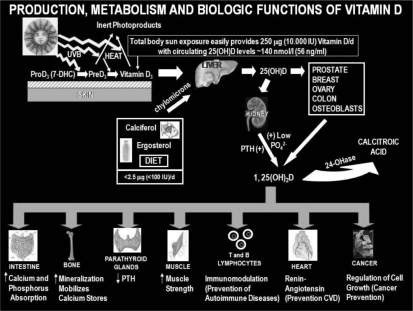
Vitamin D is synthesized in human skin after the photoisomerization of 7-dehydrocolesterol to pre-vitamin D3 under the influence of UV B radiation (wavelength, 280–315 nm) (Fig. 1). The major factors influencing this process are either environmental (latitude, season, time of day, ozone and clouds, reflectivity of the surface) or personal (skin type, age, clothing, use of sunscreen, genetics). From the skin, parental vitamin D3 find its way into the general circulation and it is then metabolized in the liver to 25-hydroxyvitamin D3 [25(OH)D3] (calcifediol) by one of several, high capacity cytochrome P450s (Fig. 1). 25(OH)D3 is an immediate precursor metabolite to the active form of vitamin D3, 1,25-dihydroxyvitamin D3 [1,25(OH)2D3], that is the product of the mitochondrial CYP27B1-hydroxylase confined primarily but not entirely to the proximal tubular epithelial cell of the kidney (Fig. 1). 1,25(OH)2D3 synthesis in the kidney is stimulated by parathyroid hormone (PTH) and inhibited by fibroblast growth factor 23 (FGF23) made by osteocytes (4).
Figure 1.
Osteoporotic proximal femur fractures: a) proximal femoral fractures d) inter and subtrochanteric fracture.
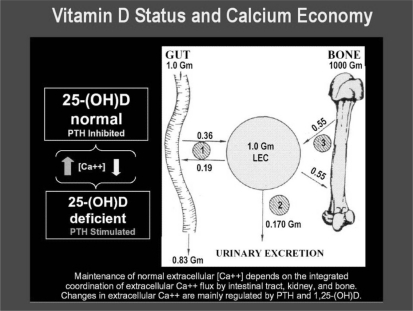
As vitamin D has a much shorter half-life than 25(OH)D3 (1–2 days versus 2–3 weeks), 25(OH)D3 was favoured as the best indicator of vitamin D status. Other reasons for 25(OH)D3 becoming the parameter of choice for estimating the vitamin D status include: it enters the host, either by cutaneous synthesis or by ingestion in the diet and it is the most abundant and stable vitamin D metabolite in human serum, as determined by its high affinity to vitamin D binding protein and by other members of the albumin superfamily of circulating proteins. Conversely, 1,25(OH)2D3 circulates in the serum at concentrations that are about 0.1% of those of the prohormone 25(OH)D3 and its synthesis is tightly regulated by the endocrine system. For these reasons 1,25(OH)2D3 levels in the serum are not used to evaluate the vitamin D status in humans (Fig. 2).
Figure 2.
Osteoporotic proximal femur fractures: a) proximal femoral fractures d) inter and subtrochanteric fracture.
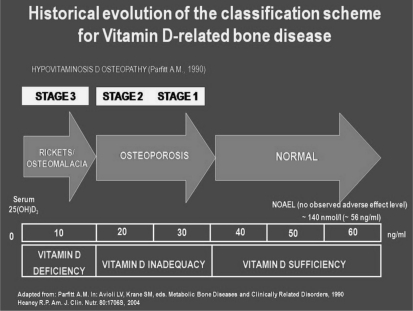
Using 25(OH)D3 circulating values and increases in serum PTH levels as markers of inadequacy and deficiency, it was possible to define the different cut-off values for the definition of the vitamin D status (Fig. 2). It is now generally agreed that the serum PTH will start to rise significantly when the serum 25(OH)D3 drops to less than 30 ng/ml; values of 25(OH)D3 between 30 ng/ml and 20 ng/ml are considered to represent vitamin D inadequacy, while those less than 20 ng/ml fall into the vitamin deficiency (Fig. 3). In this latter condition it is likely to observe clinical evidence of osteomalacia.
Figure 3.
Osteoporotic proximal femur fractures: a) proximal femoral fractures d) inter and subtrochanteric fracture.
There is growing evidence about high prevalence of unrecognized vitamin D deficiency worldwide in different age groups (2, 5–7).
Molecular bases of vitamin D metabolism and action
After production of vitamin D3 in the skin, the specific plasma alpha-globulin transport protein vitamin D-binding protein (DBP) is responsible for picking up the vitamin D3 and delivering it, along with the many vitamin D metabolites that it also binds, to all the elements of the vitamin D endocrine system (8). The first stop for vitamin D3 is normally the liver, where it is metabolized into 25(OH)D3, which has a long half-life of about 3–4 weeks. 25(OH)D3 is then transported by DBP to the kidney, which is the endocrine gland that produces the two steroid hormones 1,25(OH)2D3 (calcitriol) and the candidate hormone 24R,25-dihydroxyvitamin D3 [24,25(OH)2D3] (9). Calcitriol, which is actually the most active form of vitamin D [100-times higher than 25(OH)D3] has a very short half-life, of about a few hours. While calcitriol was first thought to be generated solely in the kidney, it is now recognized in many extrarenal tissues (10–12). The key enzymes in vitamin D metabolism are, therefore, the hepatic vitamin D-25-hydroxylase (CYP27A1,CYP2R1,CYP2A4 and CYP2J3), renal 25-hydroxyvitamin D-1alpha-hydroxylase (CYP27B1), and 25-hydroxyvitamin D-24-hydroxylase (CYP24A1) (13). Also CYP2R1, CYP27B1 and CYP24A1 were observed in tissues other than liver (14). Several liver cytochrome P450 isoforms have also been shown to possess vitamin D sidechain hydroxylation activity, wondering if this activity can be directed at the C26 position as well as the C25 position (13). Moreover cytochrome P450 CYP11A1 converts vitamin D3 to 20-hydroxyvitamin D3 [20(OH)D3] in different tissues (15). DBP then transports both secosteroids to their target tissues where appropriate biological responses are mediated.
The vitamin D metabolizing hydroxylases are regulated by different mechanisms: a rapid response involving protein kinase C and MAP kinase pathways, the binding by calcitriol to the vitamin D receptor (VDR) and the subsequent interaction of the VDR/calcitriol complex with its heterodimer partner retinoid-X-receptor and associated coactivators, and the methylation active on a more intermediate time scale (16–18).
Several reports have described an hormonal function for the various endogenous metabolites of the vitamin D endocrine complex, none being merely an inactivation product (15, 19). In particular, 25(OH)D3, previously regarded merely as a prohormone, is an agonistic VDR ligand, with gene regulatory and anti-proliferative properties synergistic with calcitriol (20).
Vitamin pleiotropy can be summarized by the following numbers: more than 30 cell types express the VDR, more than 10 organs are capable of paracrine 1- -hydroxylation, and more than 200 genes are under the control of calcitriol.
It is certainly plausible that genes that are involved in vitamin D metabolism, transport or activity may be related to risk of several chronic disorders, such as diabetes (21, 22) and osteoporosis (23, 24).
The growing availability of recombinant cytochromes P450 will allow for a search for potential inhibitors or stimulators. Modelling of the vitamin D binding pocket of VDR, DBP, and the vitamin D-related cytochrome P450 will become a major goal now that all three specific proteins have been cloned and overexpressed.
25-Hydroxylation in physiopathology
Vitamin D does not circulate for long in the blood-stream but, instead is immediately taken up by adipose tissue for storage or liver for further metabolism. Vitamin D3 undergoes its first step of activation, namely, 25-hydroxylation, in the liver (25). Even though the liver is the only significant site of 25-hydroxylation in vivo, there were occasional reports of other tissues containing this activity (26, 27). Indeed, 25-hydroxylation is carried out by four different cytochrome enzymes.
Dietary studies show regulation, albeit weak, of the liver 25-hydroxylase in animals given normal intakes of vitamin D after a period of vitamin D deficiency (28).
After the seminal work on the key role of the active vitamin D metabolite, calcitriol, in calcium homeostasis and bone mineralization, the precursor 25(OH)D3, calcifediol, was gradually ignored. Today this metabolite has been reconsidered and analyzed for its functions and it is now recognized to play a role in phosphate and calcium absorption, either via a direct effect on VDR or through a local or general increase in calcitriol production.
25(OH)D3 is a common marker of hepatic damage in individuals with chronic hepatitis (29). Patients suffering from chronic hepatitis C present with low levels of 25(OH)D3, with concentrations of vitamin D being associated with severity of inflammation and fibrosis. A relative vitamin D deficiency was associated with reduced expression of cytochrome P450 27A1. Tagher et al. found that circulating 25(OH)D3 was reduced in adults with non-alcoholic fatty liver disease in comparison with controls (30). In the latter patients vitamin D insufficiency favors progression of the liver disease from fatty liver disease to necroinflammation and fibrosis. Hepatic synthesis of calcifediol is also reduced in uremia secondary to a PTH-mediated reduction in liver CYP450 isoforms (31). Interestingly, daily oral 25(OH)D3 supplementation corrects most vitamin deficiencies in haemodialysis patients (32). 25(OH)D3 can be described as a natural non-toxic vitamin D metabolite which is present at high concentrations in serum.
Vitamin D supplementation to prevent osteoporosis
The prevalence of osteoporosis increases with advancing age, and is associated with increased susceptibility to fracture. Osteoporosis affects both sexes, but primarily postmenopausal women, because of the substantial decline in bone mass and changes in bone architecture associated with estrogen deficiency. By the end of the first decade following menopause, half of all White women have osteopenia or osteoporosis. For all these reasons it has been suggested that early postmenopausal women and patients treated with steroids should receive preventive therapy to preserve their bone mineral density. Indeed, calcium is the prevalent mineral of bone and its absorption from the intestine depends on vitamin D. A positive correlation between bone mass and calcium intake has been demonstrated in children and in adults (33, 34). Although there are many factors which modulate the progression of age-related bone loss syndromes, the pathogenesis of this process has been attributed, at least in part, to decreased calcium absorption by an aging intestine, to an associated elevation in circulating PTH, and to decreased synthesis of 1,25(OH)2D3. Decreased 1,25(OH)2D3 synthesis in the aging kidney results from both age-related progressive loss in the capacity of the renal 1-alpha-hydroxylase to respond to progressive elevation in PTH and an age-related decrease in the circulating 25(OH)D3. Indeed, vitamin D intake as well as solar exposure and cutaneous biosynthetic ability due to atrophic skin changes generally decrease with increasing age (35, 36). For all these reasons it is not surprising the finding that a low vitamin D status is common in adults and in the elderly, regardless of latitude (37, 38). All these changes in vitamin D metabolism render the ageing population at high risk for vitamin D deficiency, leading to severe consequences in terms of fall, osteoporosis, and fragility fractures.
Several studies reported that daily supplementation with vitamin D and calcium reduces fractures (39, 40). The first study that demonstrated that isolated vitamin D supplementation may prevent fractures without adverse effects was carried out in the general community (41). Vitamin D can protect against fractures through concentrations of PTH. Low concentrations of vitamin D are associated with increased concentrations of PTH, increased bone resorption, and lower bone mass. However, intervention in population studies were unable to show an effect in serum PTH levels (41).
The dilemma for the use of parental vitamin D3 for primary prevention in population-wide intervention is that whereas the population attributable risk is large, the absolute individual risk is still low (42). The risk-benefit balance for community based prevention differs from that for intervention in clinically defined groups. Safety, feasibility, and cost effectiveness are crucial.
Fractures associated with falls are a significant cause of morbidity and mortality in elderly people (43). Ninety percent of hip fractures in the elderly are associated with a fall. Given this high prevalence, severity and costs associated with treating osteoporotic fractures and effective methods of reducing or preventing falls and fractures in older people are needed. Although the possible effects of vitamin D and calcium on fracture prevention are generally attributed to increases in BMD, it is accepted that supplementation might increase muscular strength, thereby reducing the risk of falls (44). For this reason, vitamin D supplementation is highly recommended as a standard preventive measure in osteoporosis (38, 45–47). Indeed, vitamin D should be an integral part of effective osteoporosis management.
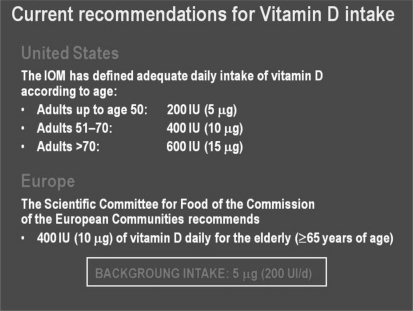
The most used approach to reducing vitamin D insufficiency or deficiency is supplementation. The daily estimated average of cholecalciferol use in an adult is 3,000–5,000 IU (48). In Europe a common RDA of 400 IU (10 g) daily has been proposed for people aged 65 years or over (49) (Fig. 4). However, according to recent evidences, higher vitamin D intakes than those currently recommended by RDAs should be advised, especially in the elderly population. The majority of the controlled clinical trials and of the intervention studies in populations used parental vitamin D3 (cholecalciferol) administered either daily or intermittently. Fortification of foods with vitamin D provides an alternative approach to direct supplementation.
Figure 4.
Osteoporotic proximal femur fractures: a) proximal femoral fractures d) inter and subtrochanteric fracture.
Taken all together the results obtained indicate the need for an adequate vitamin D and calcium intakes in the elderly, particularly in individuals living indoors in nursing homes, who exhibit a high prevalence of vitamin D deficiency. Certainly, a more widespread use of vitamin D would be worthwhile to protect the frail elderly. Indeed, parental vitamin D is one of the few treatment modalities where prevention, appropriately targeted, would result in savings to health services (50). There is, therefore, a good case to be made for routine treatment of the frail elderly to reduce the risk of fractures.
Treatment with vitamin D metabolites
The use of isolated parental vitamin D is hampered by limitations of the sources, being unavailable in desirable dose ranges and formulations on the vitamin counters of most pharmacies worldwide. Conversely, the vitamin is easily found in health food suppliers, although some efforts may be required to find them. Also, quality control is a concern when dealing with less regulated sources. Useful alternatives to parental vitamin D3 include prescription of more expensive proprietary vitamin D3 metabolites.
The successful use of the vitamin D metabolites, 1-α-hydroxy vitamin D3 (alfacalcidiol) and 1,25[OH2D3 (calcitriol)] in the correction of calcium malabsorption in postmenopausal osteoporosis and the equally successful use of parental vitamin D3 itself in the prevention of bone loss and fractures in older women have tended to confuse these two treatment modalities in some sections of the medical community. Indeed, the indications for treatment with vitamin D [or 25(OH)D3 (calcifediol)] are quite distinct from the indications for treatment with what are sometimes called the “hormonal” forms of vitamin D, notably calcitriol and alfacalcidiol. Practitioners need to appreciate the important distinction among these different metabolites and vitamin D itself.
Calcitriol
In contrast with primary vitamin D deficiency (i.e. in postmenopausal women) 1,25(OH)2D3 deficiency is caused by insufficient renal production of the active vitamin D hormone. Therefore, disorders associated with calcitriol deficiency could be corrected only increasing the supply of 1-alpha-derivatives. This is certainly true in conditions like hypoparathyroidism and kidney failure, when 1-alpha-hydroxylation does not function respectively for the lack of PTH and for the kidney tubular cell degeneration. However, studies exist on the potential use of calcitriol also in postmenopausal osteoporosis.
Both calcitriol and alfacalcidiol have been proposed as potential therapies for osteoporosis (51, 52). Both compounds strongly stimulate intestinal calcium absorption in a dose-dependent manner, leading to suppression of PTH secretion and to decreased bone turnover. Decreased calcitriol synthesis by the aging kidney results from both an age-related progressive loss in the capacity of the renal 1-alpha-hydroxylase to respond to progressive elevation in circulatory PTH and an age-related decrease in serum calcifediol, the precursor of calcitriol (53).
A number of clinical trials have been conducted over the years with the aim of verifying the efficacy of calcitriol in involutional osteoporosis. The effects reported are heterogeneous both on BMD and on fracture rates, with some showing a significant effect and others no effect on fracture risk (54).The two trials showing the greatest effect of calcitriol on vertebral fracture rates have been those of Tilyard et al. (55) on a large number of patients and that of Gallagher and Riggs (56) on a more modest number. Both studies utilized algorithms for the detection of new fractures similar to the studies reporting lesser effects on vertebral fracture, and may therefore underestimate the benefit. No studies have been undertaken to examine the effects of calcitriol on hip fractures.
It is widely appreciated that the window of efficacy for calcitriol is quite narrow. Whereas 0.4 μg/day may be insufficient for increasing calcium absorption in several patients, a dose of 0.5 μg/day is effective in nearly all patients, with an effect on BMD visible at doses above 0.43 μg/day (57).
Hypercalcemia and impairment of kidney function are rare with doses up to 0.5 μg/day, but more frequent with higher doses (1–2 μg/day). For these reasons, treatment with calcitriol necessitates monitoring of serum and urinary calcium, unlike treatment with parental vitamin D. There is a need to monitor treatment so that hypercalcemia is avoided. Increases in urinary calcium can occur before hypercalcemia and serial estimates can be made to avoid hypercalciuria, and the dose titrated appropriately. The use of calcium supplements is likely to increase the risk of toxicity and to decrease the dose tolerated, but lower doses with higher intakes of calcium might induce similar effects.
Calcitriol is certainly the drug of choice in the treatment of calcitriol deficient conditions by the specialists. General practitioners should better know the conditions that are mandatory for this treatment (i.e. hypoparathyroidism and kidney failure). The osteoporotic patients with overt osteomalacia could certainly benefit of an initial treatment with calcitriol before maintenance to be initiated with parental vitamin D3 administration.
Alfacalcidiol
Alfacalcidiol was initially synthesized in order to treat the bone disease of patients with chronic renal disease more effectively since the renal 1-α-hydroxylation of 25(OH)D3 is compromised in these individuals (58). Alfacalcidiol is a synthetic precursor of calcitriol, being converted into 1,25(OH)2D3 in vivo before exerting its biological functions. This activation takes place even with advanced liver disease. Because of this pharmacokinetic profile, alfacalcidiol is considered safer than calcitriol as regard the risk of undesirable events (i.e. hypercalcemia and hypercalciuria). However, as the majority of studies with alfacalcidiol were carried out in Japan, where the daily customary calcium intake is quite lower than in Western countries, the low incidence of hypercalcemia in treated Japanese patients could be explained by the reduced calcium intake.
Although studies designed to pursue the details of the biological response to alfacalcidiol have not been as extensive as those with calcitriol, results of clinical studies designed either to prevent or treat osteoporosis with alfacalcidiol are similar to those obtained with calcitriol (59–61). Other positive actions of alfacalcidiol include increase in muscle strength and neuromuscular coordination, with decrease in the risk of falls (62, 63).
Alfacalcidiol has been largely used in Japan in the last 25 years, but its prescription by general practitioners in Europe is very small and the novel formulations of oral and injectable parental vitamin D will not leave much space for the routine use of this compound either in vitamin D or in 1,25(OH)2D3 deficient conditions.
Calcifediol
25(OH)D3 (calcifediol), the predominant circulating form of vitamin D, is for this reason considered to be the most reliable index in a person’s vitamin D status. This vitamin D metabolite is another useful alternative in vitamin D supplementation, with lower risk of toxicity when compared to “activated forms” of vitamin D3, such as calcitriol and alfacalcidiol (64).
Beside being the storage form of vitamin D in the human body, calcifediol shows little intrinsic biological activity, at least at physiological concentrations. However, it has been suggested that 25(OH)D3 at very high levels, could mimic calcitriol to act on VDR to exert biological effects (65,66). Accordingly, it is theoretically feasible that calcitriol deficiency/resistance may be treated with needed doses of calcifediol.
Studies carried out in animals showed that calcifediol added to animal feed is absorbed in the intestine better than cholecalciferol and this explains the higher biopotency of 25(OH)D3 versus parental vitamin D3 in protective immunity to infection, in reproductive performance and in bone status markers (67–69). In the supplementation of animal diets calcifediol is today considered more bioavailable than vitamin D3 and, as such, could be considered an equivalent or even more advantageous source of vitamin D.
The extrarenal synthesis of calcitriol has been demonstrated in a number of cell types, including osteoclasts and osteoblasts (10–12,70), suggesting that 25D metabolism is an important intrinsic mechanism for optimizing its biological functions.
An alternate pathway for the metabolism of 25(OH)D3 is the formation of 24,25(OH)2D3, whose physiological role is controversial. Some authors have proposed that 24,25(OH)2D3 production represents a mean to inactivate circulating calcifediol and thus regulate production of calcitriol. In this view, 24,25(OH)2D3 is considered a catabolite of 25(OH)D3 (71).Results from in vitro studies and experiments in animal models contradict this conclusion (72). Evidence gathered in vivo also supports a physiological role for the natural 24,25(OH)2D3 metabolite during embryogenesis and in processes regulating bone growth, development, and repair (73). What is the mechanism of action of the 24,25(OH)2D3 metabolite in its target cells? Receptor-mediated signalling remains a logical possibility. Alternatively, it should be mentioned that nongenomic effects of 24,25(OH)2D3 have been described. 24,25(OH)2D3 significantly enhance bone mineralization, significantly decreases PTH secretion in humans and when used in combination with calcitriol is superior to either metabolite alone in the healing of experimental dietary rickets (74–76). More importantly 24,25(OH)2D3 supplementation was shown to be able to correct hyperparathyroidism improving skeletal abnormalities in X-linked hypophosphatemic rickets (77).
A number of clinical studies were carried out in humans in order to evaluate the effect of calcifediol in mineral and bone metabolism. In an open randomized study calcifediol, administered at a dosage of 32,000 IU per week, was demonstrated to be the most effective drug in the prevention and treatment of bone loss in patients after cardiac transplantation (78).The reasons for the authors to use calcifediol instead of other vitamin D metabolites were its lower cost, the positive effect previously shown in glucocorticoid-induced osteoporosis (79) and the lower incidence of hypercalcemia and hypercalciuria if compared to calcitriol (64, 80).
In 2000 Sosa et al. showed an increase in femoral neck BMD and a decrease in serum PTH in an open prospective study in osteoporotic postmenopausal women who suffered of proximal femoral fractures treated for one year with 1 gr calcium per day and 10,640 IU 25(OH)D3 per week when compared to a control group treated only with 1 gr calcium daily (81). In this study calcifediol treatment did not produce changes in biochemical markers of bone remodelling or in the BMD of the lumbar spine, and did not reduce the rate of appearance of new fractures. However, the number of patients in this study was small and the follow-up was too short to conclude that this intervention would not be able to reduce fractures in an at risk population. In this as in other studies 25(OH)D3 administration did not influence calcium levels in the serum and in the urines (81, 82).
In 2001 Larrosa et al. demonstrated that calcium and calcifediol supplementation at two different regimens, 16,000 IU per week and 16,000 IU every three weeks, in a cross-sectional study of 100 randomly recruited elderly institutionalized subjects normalized serum 25(OH)D3 levels, improved calcium absorption and compensated secondary hyperparathyroidism, yet higher 25(OH)D3 levels were achieved with the weekly therapeutic scheme (83). The study made possible to conclude that calcium and vitamin D supplementation should be employed routinely in the elderly instituzionalized population. In a paper in 2003 the same group was able to show that treatment with calcifediol is effective in compensating vitamin D deficiency in humans, using an initial weekly dose of 16,000 I.U. for four weeks and then the same maintenance dose every three or four weeks (84).
In two consequent studies Rossini et al. were able to demonstrate a good compliance to weekly treatment with weekly 4,000–6,000 IU calcifediol in postmenopausal and senile osteoporosis, while the daily administration of associated calcium and parental vitamin D was characterized by interruption of the therapy in over 50% of patients within six months (85, 86).
In a recent report our group showed that 20,000 IU calcifediol administered monthly with 500 mg calcium daily for three months to postmenopausal women was capable to correct hyperparathyroidism, without undesirable effects (87).
Certainly calcifediol represents a rational choice in patients who are taking anticonvulsant drugs in those with chronic liver disease, in subjects characterized by malabsorption and also in those with chronic kidney disease.
In children and in adults with cerebral palsy a high incidence of long-bone fractures was related to vitamin D deficiency (88). The use of antipileptic drugs is also associated with bone disease, characterized by low BMD and osteomalacia/rickets (89). Enzyme-inducing antipileptic drugs cause the induction of the hepatic cytocrome P450 enzyme system, lower serum vitamin D levels and decrease BMD (90). The simultaneous supplementation with oral calcium and 25OHD3 is effective in preventing the development of rickets and osteomalacia in patients undergoing antipileptic treatment (91).
As the activation of parental vitamin D3 to the 25-hydroxylated compound is performed in the liver, end-stage liver disease compromizes the production of 25(OH)D3. Moreover, vitamin D is one of the fat-soluble vitamins that require bile acid for absorption. In patients with cholestatic liver disease, absorption of vitamin D is poor because of poor secretion of bile juice (92). Indeed in chronic hepatitis patients had low 25(OH)D3 serum levels, possibly because of reduced CYP27A1 expression (93). Also patients with non-alcoholic fatty liver disease exhibit a marked decrease of circulating 25(OH)D3 levels (94). The role of vitamin D3 deficiency in liver disease progression needs further investigation. Administration of 25(OH)D3 could help to solve these problems.
Finally, calcifediol insufficiency is highly prevalent in chronic kidney disease, for an impairment in liver 25-hydroxylation of vitamin D secondary to a PTH-mediated reduction in liver CYP450 isoforms (95). This opens the avenue to the clinical use of the 25-hydroxylated form also in kidney failure, as originally proposed by DeLuca et al. (96).
Other Metabolites
Vitamin D analogs have been synthesized with similar bioeffects on PTH secretion, but with lower calcemia activity. Two drugs, 19-nor-1,25(OH)2D3 and 1α(OH)D2 are being used for the treatment of secondary hyperparathyroidism in the USA, and two are being used in Japan, 22-oxa-1,25(OH)2D3 and 1,25(OH)2-26,27F6D3 (97). Interestingly, the 22-oxa-derivative of calcitriol exerts an anabolic action on bone reconstruction by allogenic bone transplantation in rats (98). Also bromoacetoxy analogs have been synthesized and tested for improving the pharmacological profile of their parent compounds (99).
Future prospects
Vitamin D is an important calciotropic hormone whose endogenous production greatly overcomes the daily nutritional intake. Its function results in the control of the bone remodelling process with impacts on bone growth, maturation and metabolism. Even if the results of controlled clinical trials do not allow to derive final conclusions and to build guidelines, the administration of parental vitamin D has been shown to be pharmacologically active, safe and cost-effective for the prevention and treatment of osteoporosis.
Importantly, over the past decades several clinical trials have reported the efficacy of vitamin D hormone metabolites, as additional therapies of osteoporosis. However, further studies are needed to evaluate the relative impact of active vitamin D metabolites on fracture prevention. Such strategies should not, however, detract from the identification and treatment of other potentially modifiable causes of osteoporosis. Interestingly, for calcifediol, the first and largest product of the parental compound, evidences exist for a preferential use versus vitamin D in conditions like liver insufficiency, kidney failure, malabsorption and use of compounds influencing the hepatic vitamin D metabolism.
Acknowledgments
This work was supported by an unrestricted grant from F.I.R.M.O. Fondazione Raffaella Becagli to MLB.
References
- 1.Adams JS, Hewison M. Update in Vitamin D. J Clin Endocrinol Metab. 2010;95:471–478. doi: 10.1210/jc.2009-1773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kuchuk NO, van Schoor NM, Pluijm SM, Chines A, Lips P. Vitamin D status, parathyroid function, bone turnover, and BMD in postmenopausal women with osteoporosis: global perspective. J Bone Miner Res. 2009;24:693–701. doi: 10.1359/jbmr.081209. [DOI] [PubMed] [Google Scholar]
- 3.Hewison M. Vitamin D and innate immunity. Curr Opin Invest Drugs. 2008;9:485–490. [PubMed] [Google Scholar]
- 4.Quarles LD. Endocrine functions of bone in mineral metabolism regulation. J Clin Invest. 2008;118:3820–3828. doi: 10.1172/JCI36479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lips P. Vitamin D status and nutrition in Europe and Asia. J Steroid Biochem Mol Biol. 2007;103:620–625. doi: 10.1016/j.jsbmb.2006.12.076. [DOI] [PubMed] [Google Scholar]
- 6.Yetley EA. Assessing the vitamin D status of the US population. Am J Clin Nutr. 2008;88:558S–564S. doi: 10.1093/ajcn/88.2.558S. [DOI] [PubMed] [Google Scholar]
- 7.Ginde AA, Liu MC, Camargo CA., Jr Demographic differences and trends of vitamin D insufficiency in the US population, 1988–2004. Arch Intern Med. 2009;169:626–632. doi: 10.1001/archinternmed.2008.604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bouillon R, Okamura WH, Norman AW. Structure-function relationships in the vitamin D endocrine system. Endocr Rev. 1995;16:200–257. doi: 10.1210/edrv-16-2-200. [DOI] [PubMed] [Google Scholar]
- 9.Kato A, Seo E-G, Einhorn TA, Bishop JE, Norman AW. Studies on 24R,25-dihydroxyvitamin D3: evidence for a non-nuclear membrane receptor in chick tibial fracture-healing callus. Bone. 1998;23:141–146. doi: 10.1016/s8756-3282(98)00085-4. [DOI] [PubMed] [Google Scholar]
- 10.Zehnder D, Bland R, Williams MC, McNinch RW, Howie AJ, Stewart PM, Hewison M. Extrarenal expression of the 25-hydroxyvitamin D3-1alpha-hydroxylase. J Clin Endocrinol Metab. 2001;86:888–894. doi: 10.1210/jcem.86.2.7220. [DOI] [PubMed] [Google Scholar]
- 11.Turner AG, Dwivedi PP, Anderson PH, May BK, Morris HA. Regulation of the 5′-flanking region of the human CYP27B1 gene in osteoblast cells. Mol Cell Endocrinol. 2009;311:55–61. doi: 10.1016/j.mce.2009.06.001. [DOI] [PubMed] [Google Scholar]
- 12.Zhou S, LeBoff MS, Glowacki J. Vitamin D metabolism and action in human bone marrow stromal cells. Endocrinology. 2010;151:14–22. doi: 10.1210/en.2009-0969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Masuda S, Byford V, Arabian A, Sakai Y, Demay MB, St-Arnaud R, Jones G. Altered pharmacokinetics of 1,25-dihydroxyvitamin D3 and 25-hydroxyvitamin D3 in the blood and tissues of the 25-hydroxyvitamin D-24-hydroxylase (Cyp24a1) null mouse. Endocrinology. 2005;146:825–834. doi: 10.1210/en.2004-1116. [DOI] [PubMed] [Google Scholar]
- 14.Blomberg JM, Nielsen JE, Jorgensen A, Rajpert-De Meyts E, Kristensen DM, Jorgensen N, Skakkebawk NE, Juul A, Leffers H. Vitamin D receptor and vitamin D metabolizing enzymes are expressed in the human male reproductive tract. Hum Reprod. 2010;25:1303–1311. doi: 10.1093/humrep/deq024. [DOI] [PubMed] [Google Scholar]
- 15.Zbytek B, Janjetovic Z, Tuckey RC, Zmijewski MA, Sweatman TW, Jones E, Nguyen MN, Slominski AT. 20-Hydroxyvitamin D3, a product of vitamin D3 hydroxylation by cytochrome P450scc, stimulates keratinocyte differentiation. J Invest Dermatol. 2008;128:2271–2280. doi: 10.1038/jid.2008.62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Omdahl JL, Morris HA, May BK. Hydroxylase enzymes of the vitamin D pathway: expression, function, and regulation. Annu Rev Nutr. 2002;22:139–166. doi: 10.1146/annurev.nutr.22.120501.150216. [DOI] [PubMed] [Google Scholar]
- 17.Novakovic B, Sibson M, Ng HK, Manuelpillai U, Rakyan V, Down T, Beck S, Fournier T, Evain-Brion D, Dimitriadis E, Craig JM, Morley R, Saffery R. Placenta-specific methylation of the vitamin D 24-hydroxylase gene: implications for feedback autoregulation of active vitamin D levels at the fetomaternal interface. J Biol Chem. 2009;284:14838–14848. doi: 10.1074/jbc.M809542200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wjst M, Heimbeck I, Kutschke D, Pukelsheim K. Epigenetic regulation of vitamin D converting enzymes. J Ster Biochem Mol Biol. 2010;121:80–83. doi: 10.1016/j.jsbmb.2010.03.056. [DOI] [PubMed] [Google Scholar]
- 19.Nemere I. 24,25-Dihydroxyvitamin D3 suppresses the rapid actions of 1,25-dihydroxyvitamin D3 and parathyroid hormone on calcium transport in chick intestine. J Bone Miner Res. 1999;14:1543–1549. doi: 10.1359/jbmr.1999.14.9.1543. [DOI] [PubMed] [Google Scholar]
- 20.Lou YR, Molnàr F, Perakyla M, Qiao S, Kalueff AV, St-Arnaud R, Carlberg C, Tuohimaa P. 25-Hydroxyvitamin D(3) is an agonistic vitamin D receptor ligand. J Ster Biochem Mol Biol. 2010;118:162–170. doi: 10.1016/j.jsbmb.2009.11.011. [DOI] [PubMed] [Google Scholar]
- 21.Martin RJ, McKnight AJ, Patterson CC, Sadlier DM, Maxwell AP, Warren/UK GoKinD Study Group Collaborators Nephrol Dial Transplant. 2010;25:497–503. doi: 10.1093/ndt/gfp515. [DOI] [PubMed] [Google Scholar]
- 22.Massart F, Marcucci G, Brandi ML. Pharmacogenetics of bone treatments the VDR and ER gene story. Pharmacogenomics. 2008;9(6):733–746. doi: 10.2217/14622416.9.6.733. [DOI] [PubMed] [Google Scholar]
- 23.Massart F, Reginster JY, Brandi ML. Genetics of menopause-associated diseases. Maturitas. 2001;40(2):103–116. doi: 10.1016/s0378-5122(01)00283-3. [DOI] [PubMed] [Google Scholar]
- 24.Mitri J, Pittas AG. Diabetes: Shining a light: the role of vitamin D in diabetes mellitus. Nat Rev Endocrinol. 2010;6:478. doi: 10.1038/nrendo.2010.107. [DOI] [PubMed] [Google Scholar]
- 25.Blunt JW, DeLuca HF, Schnoes HK. 25-Hydroxycholecalciferol. A biologically active metabolite of vitamin D3. Biochemistry. 1968;7:3317–3322. doi: 10.1021/bi00850a001. [DOI] [PubMed] [Google Scholar]
- 26.Tucker G, Gagnon RE, Haussler MR. Vitamin D3-25-hydroxylase: tissue occurrence and lack of regulation. Arch Biochem Biophys. 1973;155:47–57. doi: 10.1016/s0003-9861(73)80008-6. [DOI] [PubMed] [Google Scholar]
- 27.Ichikawa F, Sato K, Nanjo M, Nishii Y, Shinki T, Takahashi N, Suda T. Mouse primary osteoblasts express vitamin D3 25-hydroxylase mRNA and convert 1alpha-hydroxyvitamin D3 into 1,25-dihydroxyvitamin D3. Bone. 1995;16:129–135. [PubMed] [Google Scholar]
- 28.Bhattacharyya MH, DeLuca HF. The regulation of the rat liver calciferol-25-hydroxylase. J Biol Chem. 1973;248:2969–2973. [PubMed] [Google Scholar]
- 29.Petta S, Cammà C, Scazzone C, Tripodo C, Di Marco V, Bono A, Cabibi D, Licata G, Porcasi R, Marchesini G, Craxi A. Low vitamin D serum level is related to severe fibrosis and low responsiveness to interferon-based therapy in genotype 1 chronic hepatitis C. Hepatology. 2010;51:1158–1167. doi: 10.1002/hep.23489. [DOI] [PubMed] [Google Scholar]
- 30.Tagher G, Bertolini L, Scala L, Cigolini M, Zenari L, Falezza G, Arcaro G. Associations between serum 25-hydroxyvitamin D3 concentrations and liver histology in patients with non-alcoholic fatty liver disease. Nutr Metab Cardiovasc Dis. 2007;17:517–524. doi: 10.1016/j.numecd.2006.04.002. [DOI] [PubMed] [Google Scholar]
- 31.Michaud J, Naud J, Ouimet D, Demers C, Petit JL, Leblond FA, Bonnardeaux A, Gascon-Barrè M, Pichette V. Reduced hepatic synthesis of calcidiol in uremia. J Am Soc Nephrol. 2010;21:1488–1497. doi: 10.1681/ASN.2009080815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Jean G, Terrat JC, Vanel H, Hurot JM, Lorriaux C, Mayoir B, Chazot C. Daily oral 25-hydroxycholecalciferol supplementation for vitamin D deficiency in haemodialysis patients: effects on mineral metabolism and bone markers. Nephrol Dial Transplant. 2008;23:3670–3676. doi: 10.1093/ndt/gfn339. [DOI] [PubMed] [Google Scholar]
- 33.Jackman LA, Millane SS, Martin BR, Wood OB, McCabe GP, Peacock M, Weaver CM. Calcium retention in relation to calcium intake and postmenarcheal age in adolescent females. Am J Clin Nutr. 1997;66:327–333. doi: 10.1093/ajcn/66.2.327. [DOI] [PubMed] [Google Scholar]
- 34.Welten DC, Kemper HC, Post GB, van Staveren WA. A metanalysis of the effect of calcium intake on bone mass in young and middle aged females and males. J Nutr. 1995;25:2802–2813. doi: 10.1093/jn/125.11.2802. [DOI] [PubMed] [Google Scholar]
- 35.Mosekilde L. Vitamin D and the elderly. Clin Endocrinol. 2005;62:265–281. doi: 10.1111/j.1365-2265.2005.02226.x. [DOI] [PubMed] [Google Scholar]
- 36.Holick MF, Mastuoka LY, Wortsman J. Age, vitamin D and solar ultraviolet radiation. Lancet. 1989;4:1104–1105. doi: 10.1016/s0140-6736(89)91124-0. [DOI] [PubMed] [Google Scholar]
- 37.Looker A, Dawson-Hughes B, Calvo MS, Gunter EW, Sahyoun NR. Serum 25-hydroxyvitamin D status of adolescents and adults in two seasonal subpopulations from NHANES III. Bone. 2002;30:771–777. doi: 10.1016/s8756-3282(02)00692-0. [DOI] [PubMed] [Google Scholar]
- 38.Lips P. Vitamin D deficiency and secondary hyperparathyroidsism in the elderly: consequences for bone loss and fractures and therapeutic implications. Endocr Rev. 2001;22:477–501. doi: 10.1210/edrv.22.4.0437. [DOI] [PubMed] [Google Scholar]
- 39.Dawson-Hughes B, Harris SS, Krall EA, Dallal GE. Effect of calcium and vitamin D supplementation on bone density in men and women 65 years of age or older. N Engl J Med. 1997;337:670–676. doi: 10.1056/NEJM199709043371003. [DOI] [PubMed] [Google Scholar]
- 40.Chapuy MC, Arlot ME, Duboeuf F, Brun J, Crouzet B, Arnaud S, Delmas PD, Meurnier PJ. Vitamin D3 and calcium to prevent hip fractures in the elderly women. N Engl J Med. 1992;327:1637–1642. doi: 10.1056/NEJM199212033272305. [DOI] [PubMed] [Google Scholar]
- 41.Trivedi DP, Doll R, Khaw KT. Effect of four monthly oral vitamin D3 (cholecalciferol) supplementation on fractures and mortality in men and women living in the community: randomised double blind controlled trial. Br Med J. 2003;326:469. doi: 10.1136/bmj.326.7387.469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Rose G. Strategy of preventive medicine. Oxford: Oxford University Press; 1992. [Google Scholar]
- 43.Bischoff-Ferrari HA, Conselmann M, Dick W, Theiler R, Stahelin HB. Effect of vitamin D on muscle strength and relevance in regard of osteoporosis prevention. Z Rheumatol. 2003;62:518–521. doi: 10.1007/s00393-003-0561-4. [DOI] [PubMed] [Google Scholar]
- 44.Pfeifer M, Bergerow B, Minne HW. Vitamin D and muscle function. Osteoporos Int. 2002;13:187–194. doi: 10.1007/s001980200012. [DOI] [PubMed] [Google Scholar]
- 45.Jackson C, Gaugris S, Sen SS, Hosking D. The effect of cholecalciferol (vitamin D3) on the risk of fall and fracture: a meta-analysis. Q J Med. 2007;100:185–192. doi: 10.1093/qjmed/hcm005. [DOI] [PubMed] [Google Scholar]
- 46.Bischoff HA, Stahelin HB, Dick W, Akos R, Knecht M, Salis C, Nebiker M, Theiler R, Pfeifer M, Begerow B, Lew RA, Conzelmann M. Effects of vitamin D and calcium supplementation on falls: a randomized controlled trial. J Bone Miner Res. 2003;18:343–351. doi: 10.1359/jbmr.2003.18.2.343. [DOI] [PubMed] [Google Scholar]
- 47.Pfeifer M, Begerow B, Minne HW, Nachtigall D, Hansen C. Effects of a short-term vitamin D and calcium supplementation on body sway and secondary hyperparathyroidism in elderly women. J Bone Miner Res. 2000;15:1113–1118. doi: 10.1359/jbmr.2000.15.6.1113. [DOI] [PubMed] [Google Scholar]
- 48.Barger-Lux MJ, Heaney RP, Dowell S, Chen TC, Holick MF. Vitamin D and its major metabolites: serum levels after graded oral dosing in healthy men. Osteoporos Int. 1998;8:222–230. doi: 10.1007/s001980050058. [DOI] [PubMed] [Google Scholar]
- 49.Report on osteoporosis in the European Community – Action on prevention. Luxembourg Office for Official Publications of the European Community European Commission. 1998. p. 12.
- 50.Torgerson DJ, Kanis JA. Cost-effectiveness of preventing hip fractures in the elderly population using vitamin D and calcium. QJM. 1995;88:135–139. [PubMed] [Google Scholar]
- 51.Buckhardt P, Lamy O. Vitamin D and its metabolites in the treatment of osteoporosis. Osteoporos Int. 1998;8:S40–S44. doi: 10.1007/pl00022732. [DOI] [PubMed] [Google Scholar]
- 52.Avioli LV. Vitamin D the D-hormones, alfacalcidiol and calcitriol, as therapeutic agents for osteoporotic populations. Calcif Tissue Int. 1999;65:292–294. doi: 10.1007/s002239900701. [DOI] [PubMed] [Google Scholar]
- 53.Gallagher JC, Riggs BL, Eisman J, DeLuca HF. Intestinal calcium absorption and serum vitamin D metabolites in normal subjects and osteoporotic patients: effect of age and dietary calcium. J Clin Invest. 1979;64:729–736. doi: 10.1172/JCI109516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Kanis JA, McCloskey EV, de Takats D, Bernard J, Zhang DM. Treatment of osteoporosis with vitamin D. Osteoporos Int. 1997;7(Suppl 3):S140–S146. doi: 10.1007/BF03194360. [DOI] [PubMed] [Google Scholar]
- 55.Gallagher JC, Riggs BL. Action of 1,25-dihydroxyvitamin D3 on calcium balance and bone turnover and its effects on vertebral fracture rate. Metabolism. 1990;4:S30–S34. doi: 10.1016/0026-0495(90)90269-i. [DOI] [PubMed] [Google Scholar]
- 56.Tilyard M, Spears GFS, Thomson J, Dovey S. Treatment of postmenopausal osteoporosis with calcitriol or calcium. N Engl J Med. 1992;326:357–362. doi: 10.1056/NEJM199202063260601. [DOI] [PubMed] [Google Scholar]
- 57.Papadimitropoulos E, Wells G, Shea B, Gillespie W, Weaver B, Zytaruk N, Cranney A, Adachi J, Tugwell P, Josse R, Greenwood C, Guyatt G, Osteoporosis Methodology Group and the Osteoporosis Research Advisory Group Metaanalysis of the efficacy of vitamin D treatment in preventing osteoporosis postmenopausal women. Endocr Rev. 2002;23:560–569. doi: 10.1210/er.2001-8002. [DOI] [PubMed] [Google Scholar]
- 58.Barton DH, Hesse HR, Pechet MM, Rizzardo E. A convenient synthesis of 1alphavitaminD3. J Am Chem Soc. 1973;95:2748–2749. doi: 10.1021/ja00789a090. [DOI] [PubMed] [Google Scholar]
- 59.Orimo H, Shiraki M, Hayashi T, Nakamura T. Reduced occurrence of vertebral crush fractures in senile osteoporosis treated with 1alpha(OH)D3. Bon and prevention of falls and fractures. Bone Miner. 1987;3:47–52. [PubMed] [Google Scholar]
- 60.Orimo H, Shiraki M, Hayashi Y, Hoshino T, Onaya T, Miyazaki S, Kurosawa H, Nakamura T, Ogawa N. Effects of 1alpha-hydroxyvitamin D3 on lumbar bone mineral density and vertebral fractures in patients with postmenopausal osteoporosis. Calcif Tissue Int. 1994;54:370–376. doi: 10.1007/BF00305521. [DOI] [PubMed] [Google Scholar]
- 61.Pouilles JM, Tremollieres F, Ribot C. Prevention of postmenopausal bone loss with 1 alpha-hydroxyvitamin D3: a three-year prospective study. Clin Rheumatol. 1992;11:1492–1497. doi: 10.1007/BF02283104. [DOI] [PubMed] [Google Scholar]
- 62.Schacht E, Richy F, Reginster JY. The therapeutic affects of alfacalcidiol on bone strength, muscle metabolism. J Musculoskelet Neuronal Interact. 2005;5:273–284. [PubMed] [Google Scholar]
- 63.Sorenson OH, Lund B, Saltin B. Myopathy in bone loss of aging: improvement by treatment with 1-alphahydroxycholecalciferol and calcium. Clin Sci. 1979;56:157–161. doi: 10.1042/cs0560157. [DOI] [PubMed] [Google Scholar]
- 64.Heaney RP. Vitamin D: how much do we need and how much is too much? Osteoporos Int. 2000;11:553–555. doi: 10.1007/s001980070074. [DOI] [PubMed] [Google Scholar]
- 65.Olson EB, DeLuca HF. 25-Hydroxycholecalciferol: direct effect on calcium transport. Science. 1969;165:405–407. doi: 10.1126/science.165.3891.405. [DOI] [PubMed] [Google Scholar]
- 66.Cholodro IH, Brickman AS, Coburn JW, Osborn TW, Norman AW. Effect of 25.hydroxy-vitamin D3 on intestinal absorption of calcium in normal man and patients with renal failure. Metabolism. 1978;27:745–753. doi: 10.1016/0026-0495(78)90013-6. [DOI] [PubMed] [Google Scholar]
- 67.Chou SH, Chung TK, Yu B. Effects of supplemental 25-hydroxycholecalciferol on growth performance, small intestinal morphology, and immune response of broiler chickens. Poultry Sci. 2009;88:2333–2341. doi: 10.3382/ps.2009-00283. [DOI] [PubMed] [Google Scholar]
- 68.Lauridsen C, Halekoh U, Larsen T, Jensen SK. Reproductive performance and bone status markers of gilts and lactating sows supplemented with two different forms of vitamin D. J Anim Sci. 2010;88:202–213. doi: 10.2527/jas.2009-1976. [DOI] [PubMed] [Google Scholar]
- 69.Sahin N, Balci TA, Kucuk O, Smith MO, Sahin K. Effects of 25-hydroxycholecalciferol and soy isoflavones supplementation on bone mineralisation of quail. Br Poult Sci. 2009;50:709–715. doi: 10.1080/00071660903261944. [DOI] [PubMed] [Google Scholar]
- 70.Kogawa M, Findlay DM, Anderson PH, Ormsby R, Vincent C, Morris HA, Atkins GJ. Osteoclastic metabolism of 25(OH)-vitamin D3: a potential mechanism for optimization of bone resorption. Endocrinology. 2010 Aug 25; doi: 10.1210/en.2010-0334. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 71.Parfitt AM, Mathews CHE, Brommage R, Jarnagin K, DeLuca HF. Calcitriol but no other metabolite of vitamin D is essential for normal bone growth and development in the rat. J Clin Invest. 1984;73:576–586. doi: 10.1172/JCI111246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Boyan BK, Dean DD, Sylvia VL, Schwartz Z. Cartilage and vitamin D: genomic and nongenomic regulation by 1,25(OH)2D3 and 24,25(OH)2D3. In: Feldman D, Glorieux FH, Pike JW, editors. Vitamin D. Academic press; San Diego: pp. 395–421. [Google Scholar]
- 73.Norman AW, Leathers V, Bishp JE. Normal egg hatchability requires the simultaneous administration to the hen of 1alpha,25-dihydroxycholecalciferol and 24R, 25-dihydroxycholecalciferol. J Nutr. 1983;113:2505–2515. doi: 10.1093/jn/113.12.2505. [DOI] [PubMed] [Google Scholar]
- 74.Endo H, Kiyoki M, Kawashima K, Naguchi T, Hashimoto Y. Vitamin D metabolites and PTH synergistically stimulate bone formation. Nature. 1980;286:262–264. doi: 10.1038/286262a0. [DOI] [PubMed] [Google Scholar]
- 75.Yamate T, Tanaka H, Nagai Y, Yamato H, Taniguchi N, Nakamura T, Seino Y. Bone forming ability of 24R,25-hydroxyvitamin D3 in the hypophosphatemic mouse. J Bone Miner Res. 1994;9:1967–1974. doi: 10.1002/jbmr.5650091217. [DOI] [PubMed] [Google Scholar]
- 76.Canterbury JM, Lerman S, Claflin AJ, Henry H. Inhibition of parathyroid hormone secretion by 25-hydroxycholecalciferol and 24,25-dihydroxycholecalciferol in the dog. J Clin Invest. 1978;61:1375–1383. doi: 10.1172/JCI109055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Carpenter TO, Keller M, Schwartz D, Mitnick M, Smith C, Ellison A, Carey D, Comite F, Horst R, Travers R, Glorieux FH, Gundberg CM, Poole AR, Insogna KL. 24,25 Dihydroxyvitamin D supplementation corrects hyperparathyroidism and improves skeletal abnormalities in X-linked hypophosphatemic rickets. A clinical research center study. J Clin Endocrinol Metab. 1996;81:2381–2388. doi: 10.1210/jcem.81.6.8964881. [DOI] [PubMed] [Google Scholar]
- 78.Garcia-Delgado I, Prieto S, Gil-Fraguas L, Robles E, Rufilanchas JJ, Hawkins F. Calcitonin, etidronate, and calcidiol treatment in bone loss after cardiac transplantation. Calcif Tissue Int. 1997;60:155–159. doi: 10.1007/s002239900206. [DOI] [PubMed] [Google Scholar]
- 79.Hahan TJ, Halstead L, Teitelbaum S. Altered mineral metabolism in glucocorticoid-induced osteopenia. J Clin Invest. 1979;64:655–665. doi: 10.1172/JCI109506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Dykman TR, Haralson KM, Gluck OS, Murphy WA, Teitelbaum SL, Jajm TH, Hahn BH. Effect of oral 1,25 dihydroxyvitamin D and calcium on glucocorticoid-induced osteopenia in patients with rheumatic diseases. Arthr Rheum. 1984;27:1336–1343. doi: 10.1002/art.1780271203. [DOI] [PubMed] [Google Scholar]
- 81.Sosa M, Làinez P, Arbelo A, Navarro MC. The effect of 25-dihydroxyvitamin D on the bone mineral metabolism of elderly women with hip fracture. Rheumatology. 2000;39:1263–1268. doi: 10.1093/rheumatology/39.11.1263. [DOI] [PubMed] [Google Scholar]
- 82.Peacock M, Liu G, Carey M, McClintock R, Ambrosius W, Hui S, Johnston CC. Effect of calcium on 25OH vitamin D3 dietary supplementation on bone loss at the hip in men and women over the age of 60. J Clin Endocrinol Metab. 2000;85:3011–3019. doi: 10.1210/jcem.85.9.6836. [DOI] [PubMed] [Google Scholar]
- 83.Larrosa M, Gratacòs J, Vaqueiro M, Prat M, Campos F, Roqué M. Prevalence of hypovitaminosis D in elderly instituzionalized residents: influence of substitutive treatment. Med Clin. 2001;117:611–614. doi: 10.1016/s0025-7753(01)72195-1. [DOI] [PubMed] [Google Scholar]
- 84.Larrosa M, Gratacós J, Fernàndez ME, Berlanga E, Casado E, Gómez A, Real J. Calcidiol treatment and serum 25-OHD3 levels. What treatment regimen should be used? Rev Esp Reumatol. 2003;30(10):548–553. [Google Scholar]
- 85.Rossini M, Viapiana O, Gatti D, James G, Girardello S, Adami S. La correzione dell’ipovitaminosi D nel lungo termine: confronto tra diverse modalità di somministrazione di vitamina D nella pratica clinica. Minerva Med. 2005;96:1–7. [Google Scholar]
- 86.Rossini M, Viapiana O, Idolazzi I, Fracassi F, Gatti D, Adami S. Razionale e risultati del trattamento settimanale con calcifediolo nel-l’osteoporosi postmenopausale e senile. Minerva Med. 2007;98:53–68. [PubMed] [Google Scholar]
- 87.Cavalli L, Cavalli T, Marcucci G, Falchetti A, Masi L, Brandi ML. Biological effects of various regimes of 25-hydroxyvitamin D3 (calcidiol) administration on bone mineral metabolism in postmenopausal women. Clin Cases Miner Bone Metab. 2009;6:169–173. [PMC free article] [PubMed] [Google Scholar]
- 88.Bischof F, Basu D, Pettifor IM. Pathological long-bone fractures in residents with cerebral palsy in a long-term care facility in South Africa. Develop Med Child Neurol. 2002;44:119–122. doi: 10.1017/s0012162201001773. [DOI] [PubMed] [Google Scholar]
- 89.Pack AM, Gidal B, Vazquez B. Bone disease associated with antiepileptic drugs. Cliveland Clin J Med. 2004;71:S42–S48. doi: 10.3949/ccjm.71.suppl_2.s42. [DOI] [PubMed] [Google Scholar]
- 90.Pack AM, Olarte LS, Morrell MJ, Flaster E, Resor SR, Shane E. Bone mineral density in an outpatient population receiving enzyme-inducing antiepileptic drugs. Epilepsy Behav. 2003;4:169–174. doi: 10.1016/s1525-5050(03)00036-2. [DOI] [PubMed] [Google Scholar]
- 91.Krishna Moorthy G, Karande S, Ahire N, Mathew L, Kulkarni M. Bone metabolism alteration on antiepileptic drug therapy. Indian J Pediatric. 2009;76:377–383. doi: 10.1007/s12098-009-0005-5. [DOI] [PubMed] [Google Scholar]
- 92.Ohajima H, Shigeno C, Inomata Y, Egawa H, Uemoto S, Asonuma K, Kiuchi T, Konishi J, Tanaka K. Long-term effects of liver transplantation on bone mineral density in children with end-stage liver disease: a 2-year prospective study. Liver Transplant. 2003;9:360–364. doi: 10.1053/jlts.2001.50038. [DOI] [PubMed] [Google Scholar]
- 93.Petta S, Cammà C, Scappone C, Tripodo C, Di Marco V, Bono A, Cabibi D, Licata G, Porcasi R, Marchesini G, Craxi A. Low vitamin D serum level is related to severe fibrosis and low responsiveness to interferon-based therapy in genotype 1 chronic hepatitis C. Hepatology. 2010;51:1158–1167. doi: 10.1002/hep.23489. [DOI] [PubMed] [Google Scholar]
- 94.Targher G, Bertolini L, Scala L, Cigolini M, Zenari L, Falezza G, Arcaro G. Associations betweeen serum 25-hydroxyvitamin D3 concentrations and liver histology in patients with non-alcoholic fatty liver disease. Nutr Metab Cardiovasc Dis. 2007;17:517–524. doi: 10.1016/j.numecd.2006.04.002. [DOI] [PubMed] [Google Scholar]
- 95.Michaud I, Naud J, Ouimet D, Demers C, Petit JL, Leblond FA, Bounardeaux A, Gascon-Barrè M, Pichette V. Reduced hepatic synthesis of calcidiol in uremia. J Am Soc Nephrol. 2010;21:1488–1497. doi: 10.1681/ASN.2009080815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.DeLuca HF, Avioli LV. Treatment of renal osteodystrophy with 25-hydroxycholecalciferol. Arch Intern Med. 1970;126(5):896–899. [PubMed] [Google Scholar]
- 97.Slatopolsky E, Finch J, Brown A. New vitamin D analogs. Kidney Int Suppl. 2003;85:S83–S87. doi: 10.1046/j.1523-1755.63.s85.20.x. [DOI] [PubMed] [Google Scholar]
- 98.Merida L, Shigetomi M, Ihara K, Tsubone T, Ikeda K, Yamaguchi A, Sugiyama T, Kawai S. Effects of vitamin D analog, 22-oxa-1,25-dihydroxyvitamin D3 on bone reconstruction by vascularized bone allograft. Bone. 2002;30:422–427. doi: 10.1016/s8756-3282(01)00680-9. [DOI] [PubMed] [Google Scholar]
- 99.Lange TS, Zou Y, Singh RK, Kim KK, Kristjansdottir K, Sholler GLS, Brard L. Chemotherapeutic effect of calcidiol derivative B3CD in a neuroblastoma xenograft model. Chem Biol Drug Des. 2010;76:164–173. doi: 10.1111/j.1747-0285.2010.00988.x. [DOI] [PMC free article] [PubMed] [Google Scholar]