Abstract
Background
Interventions that target cancer patients and their caregivers have been shown to improve communication, support, and emotional well-being.
Objective
To adapt an in-person communication intervention for cancer patients and caregivers to a web-based format, and to examine the usability and acceptability of the web-based program among representative users.
Methods
A tailored, interactive web-based communication program for cancer patients and their family caregivers was developed based on an existing in-person, nurse-delivered intervention. The development process involved: 1) building a multidisciplinary team of content and web design experts, 2) combining key components of the in-person intervention with the unique tailoring and interactive features of a web-based platform, and 3) conducting focus groups and usability testing to obtain feedback from representative program users at multiple time points.
Results
Four focus groups with 2 to 3 patient-caregiver pairs per group (n = 22 total participants) and two iterations of usability testing with 4 patient-caregiver pairs per session (n = 16 total participants) were conducted. Response to the program's structure, design, and content was favorable, even among users who were older or had limited computer and internet experience. The program received high ratings for ease of use and overall usability (mean System Usability Score of 89.5 out of 100).
Conclusions
Many elements of a nurse-delivered patient-caregiver intervention can be successfully adapted to a web-based format. A multidisciplinary design team and an iterative evaluation process with representative users were instrumental in the development of a usable and well-received web-based program.
Keywords: Communication, caregiving, social support, technology assessment, cancer, oncology
INTRODUCTION
Interventions that target cancer patients and their caregivers have been shown to improve patient-caregiver communication, enhance dyadic support, and increase emotional well-being.1, 2 The internet may offer an opportunity to disseminate these interventions inexpensively to a broad audience, including those who are homebound or geographically isolated.3 Such programs have been shown to positively influence patient knowledge, behaviors, support, and clinical outcomes.4-6 Furthermore, when integrated with a patient's system of care, these programs can enhance patient-caregiver-clinician communication and positively impact care delivery.7
The FOCUS Program8, 9 was developed as a supportive-educative program for cancer patients and their caregivers. Based on a stress-coping framework,10 the program offers information and support to reduce negative appraisal of illness, enhance coping resources (communication, support), and improve emotional well-being. The program includes five core modules (Family Involvement, Optimistic Attitude, Coping Effectiveness, Uncertainty Reduction, and Symptom Management) and is delivered by nurses during three home visits and two telephone calls.
In randomized controlled trials,1, 11 FOCUS resulted in positive outcomes for patients and caregivers (e.g., less negative appraisal, hopelessness, uncertainty; improved communication, self-efficacy, emotional well-being). The cost and dissemination challenges imposed by an in-person, nurse-led intervention, however, led to interest in adapting the intervention to a web-based format. This article describes the process of developing a web-based version of the Family Involvement Module of FOCUS, and the results from initial evaluations of the program's usability and acceptability among cancer patients and their caregivers.
METHODS
Development of the Web-Based FOCUS Intervention
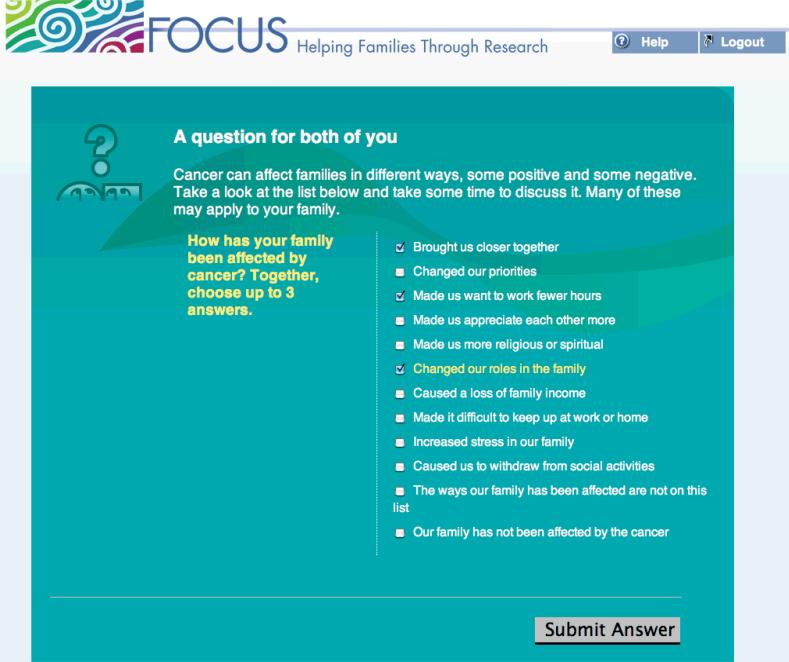
The web-based FOCUS program incorporates key components of the in-person FOCUS intervention, providing relational content that addresses communication, support, and teamwork. Just as FOCUS nurses asked patients and caregivers questions, provided feedback, and facilitated discussion, the web-based program utilizes a novel dyadic interface that directs questions to patients, caregivers, and the pair, and then provides tailored feedback based on the users’ responses.12 For example, the web-based program asks each patient and caregiver to jointly identify three concerns associated with cancer, and then provides tailored feedback suggesting specific strategies and additional websites to help them address their concerns (Figure 1).
Figure 1.
The FOCUS Web-Based Program
Several design elements were incorporated to optimize the accessibility of the web-based program for older individuals and people with limited computer experience. For example, the program features a large font size, enhanced contrast, smooth visual transitions, and a gentle color scheme. In addition, all content was examined to ensure an appropriate reading level.13
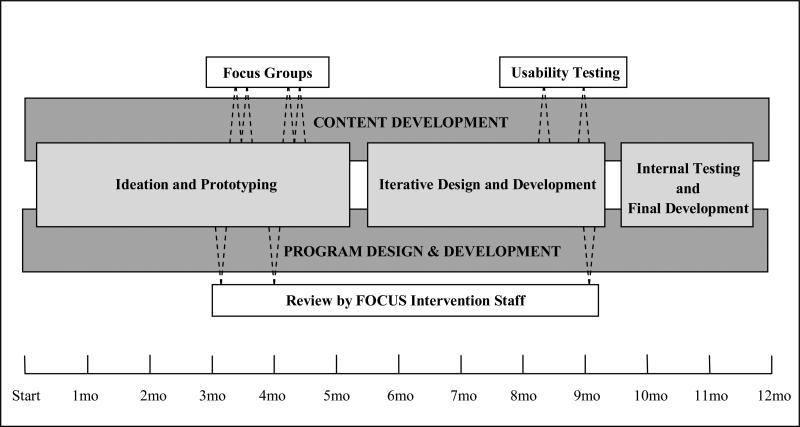
Central to the web-based program's development was a multidisciplinary team that included content experts, web developers, graphic designers, and individuals experienced in program usability processes (Figure 2). Content and design teams collaborated at regular intervals, providing an opportunity for discourse between developers of the original FOCUS intervention, and web experts with extensive experience designing highly tailored health-related internet interventions. Input was also solicited from seven nurses who implemented the in-person FOCUS Program with cancer patients and their caregivers in previous clinical trials with nearly 1000 dyads. Three of these nurses participated in weekly content meetings, and the others provided feedback at regular intervals regarding the content, design, and structure of the web-based program.
Figure 2. Timeline and Development Process for Adapting the FOCUS Intervention to a Tailored, Web-Based Format.
The development process comprised two multidisciplinary teams that met weekly, either independently or together. The Content Development Team included behavioral scientists, research investigators, FOCUS nurses, and usability specialists. The Program Design & Development Team included program developers, design specialists, behavioral scientists, and a project manager. Ideation and prototyping involved members of both Content and Design teams. Iterative design and development was led by the Design team. Focus groups of patients and their caregivers were conducted by research investigators, FOCUS nurses, and behavioral scientists. Usability testing was conducted by usability specialists and a FOCUS nurse. Content and design were reviewed periodically by FOCUS intervention staff. Internal testing and final development was conducted by developers and behavioral scientists.
An iterative approach (Figure 2) was utilized to incorporate feedback from the multidisciplinary team and from representative program users. For each component of the program, content and design features were reviewed by team members, often several times, and then prototypes were presented to patients and caregivers during focus groups and usability testing. User feedback led to further program modifications, after which rigorous internal testing was conducted to identify any remaining usability problems and to confirm accuracy of content and tailored feedback.
Program Evaluation
Early in the development process, the program was evaluated by four focus groups. Each focus group was composed of two or three patients and their caregivers, and was led by a member of the web design team and by a research nurse experienced with the FOCUS program. Participants reviewed paper and electronic mock-ups of the program, and were asked to provide positive and negative feedback on the web program's design, structure, content, and acceptability. Transcripts of the recorded groups were analyzed by two members of the content team to identify themes and representative quotes.
Once a working prototype was available, usability testing was conducted to evaluate the usability and acceptability of the web-based program. Testing procedures were based on established guidelines14 that were modified per recommendations of usability experts at the University of Michigan School of Information. Patients and caregivers were tested together as dyads in order to identify problems with paired-user features, and because paired-user testing has been shown to yield valuable information through natural discussion.15, 16 A facilitator moderated the usability testing sessions, asking participants to ‘think aloud’ while completing a set of representative task scenarios. Sessions were videotaped using Silverback usability software that captured screenshots alongside participants’ interactions with the program (Silverback, Version 1.1.2, Clearleft Limited, Brighton, U.K.). A note-taker monitored the participants’ interaction with the application, documenting feedback, problems with the program, and ease of program navigation as a pair.
Usability testing participants completed a questionnaire after the testing session in which they were asked about the perceived ease of use17 and the usability18 of the program. In addition, videotaped testing sessions were reviewed to assess the rate of critical errors (i.e., errors affecting program process) and non-critical errors (i.e., minor errors that did not affect task completion), and to assess how often dyads achieved the task's goal with no help, minor help, or major help from the facilitator.
Participants
Focus group and usability testing participants were recruited from two comprehensive cancer centers in Michigan after obtaining IRB approval. Patients with lung, colorectal, breast, or prostate cancer, and one family member selected by each patient, were recruited to participate as a dyad. Efforts were made to ensure that each cancer type was represented at least once in focus groups and usability testing, and to recruit dyads that represented a range of relationships (e.g. parent-child, spouses, friends) and different levels of internet experience. All participants provided informed consent, and received a $20 gift card as a token of appreciation.
RESULTS
Over a six month period, four focus groups with 2 to 3 patient-caregiver dyads per group (n = 22 participants) and two iterations of usability testing with 4 patient-caregiver dyads per session (n = 16 participants) were conducted. The mean participant age was 52.6 (15.5) years and close to one-third of participants were over the age of 60. Participants were diverse in terms of race (39.5% non-white), sex (65.8% women), cancer diagnosis (42.1% breast, 21.1% prostate, 21.1% lung, 15.8% colorectal), and dyad type (52.6% spouses, 31.6% parent-child, 15.8% friends). Half of the focus group participants (n = 12) reported that they were “not skilled at all” to “somewhat skilled” using the internet. In contrast, nearly all usability testing participants (n = 15) reported they felt “very skilled” using the internet.
Usability testing participants rated the program as easy to understand and use (Table 1). Analysis of users’ completion of four pre-specified tasks revealed that task completion improved and task errors decreased between testing iterations. Overall rates of task completion were high, with scores of 90.6% and 93.8% for the first and second testing iterations, respectively. None of the pairs required major assistance from the facilitator to complete any of the tasks. The total number of errors for all users decreased from 3 critical errors and 8 non-critical errors in the first testing iteration, to 2 critical errors and 4 non-critical errors in the second testing iteration.
Several themes emerged during focus groups and usability testing. First, participants commented favorably, and sometimes emotionally, about the importance of program content. For example, a common statement about the program was that it led to communication between patients and caregivers about previously unshared feelings, stimulating “discussion that you might not have or you might not even think of.” Second, users occasionally felt restricted by the constraints of the web-based program. For example, several usability testing participants voiced frustration when the program required that they select three, and only three, strengths that their partner exhibits. As one patient reflected, “Three is not enough, if you've got a good team... It's hard to pick three because they're all very important.” Third, design features were clearly essential to accommodate individuals with cancer who might be in poor health. For example, focus group participants reported that color schemes with blues and greens were “comfortable,” and “reassuring”, but requested a larger font size and more space between responses to assist people with shaky hands who might click the wrong item.
In general, participants were comfortable completing the program on the web and working together as a dyad. Two focus group participants had very little or no experience using the internet, and both felt comfortable having their family members guide them through the program. Usability testing participants commented that challenges could arise if users have different reading speeds or are accustomed to using the computer independently, but most acknowledged that there was value in completing the program as a pair. As one family member stated, “You're going through the cancer as a team so it's good to look at the computer together as a team.” Fourteen of the sixteen usability testing participants agreed that they would use this type of program to complete a health intervention in the future (Table).
Table.
Ease of Use and Usability of a Web-Based Communication Program Among Representative Cancer Patients and Their Family Caregivers (n = 16)
| Mean (SD)* | |
|---|---|
| I thought that this program was easy to understand | 6.6 (0.5) |
| I could complete the tasks that were asked of me in this program | 6.8 (0.4) |
| I found this program confusing | 1.4 (1.0) |
| Usability of Program | |
| I thought that this program was easy to use | 6.6 (0.5) |
| I would choose to use this type of program in the future to complete an intervention that aims to improve my health | 5.9 (1.0) |
| The program was too complex | 1.1 (0.3) |
| I would need help from a technical support to be able to use this program | 1.1 (0.3) |
| The program ran smoothly | 6.3 (0.8) |
| The program was inconsistent (there were parts of the program that seemed out of place) | 2.3 (1.7) |
| I think that most people would learn to use this program quickly | 6.4 (0.8) |
| Using this program felt awkward to me | 1.3 (0.4) |
| I felt very confident using this program | 6.6 (0.6) |
| I needed to learn a lot of things before I could get going with this program | 2.3 (2.1) |
| Total Usability Score† | 89.5 (8.3) |
Responses were on a 7-point scale, ranging from 1 “Strongly Disagree” to 7 “Strongly Agree.”
Composite of all usability questions (100-point score); adapted from Brooke, 1996.18
DISCUSSION
Interactive web-based programs for cancer patients and their caregivers offer an opportunity to deliver tailored information via a route that is efficient, accessible, and cost-effective. Our experience developing a web-based version of a family communication program for cancer patients and their caregivers suggests that many elements of an in-person, nurse-delivered intervention can be successfully adapted to the internet. For example, the program utilized a dyadic approach, facilitated patient-caregiver communication, and provided highly tailored feedback that was designed to resemble the feedback that nurses provided in the in-person intervention. The program was rated as easy to understand and use by representative patients and caregivers, including those who were older and less experienced with the computer and internet.
There were several aspects of the development strategy that were critical to the success of the program. First, the multidisciplinary team included individuals with experience delivering the in-person FOCUS intervention, as well as experts in content, tailored interventions, web design and application development, and program usability evaluation. Each team member was involved at multiple time points during the development process (Figure 2), and their involvement facilitated the translation of core aspects of the in-person intervention to the web. Second, the involvement of cancer patients and their caregivers during formative focus groups and usability testing provided valuable insight about how to sensitively phrase questions, response options, and feedback. The inclusion of individuals who were older and/or inexperienced with the internet additionally resulted in a number of important program modifications that improved program accessibility for these users. Finally, the iterative evaluation process created an opportunity to refine the program and examine the effects of changes.19
Our development process was limited by several factors. The majority of usability testing participants rated themselves as fairly comfortable and skilled with the internet, which could have skewed our outcomes for program usability and ease of use. However, during focus groups we found that individuals with limited computer experience often relied on their partner to navigate the program, suggesting that some technology-related barriers may be overcome in this manner. In addition, budget restrictions allowed us to test only a portion of the final content. Nevertheless, the material and design features presented during testing were representative of the entire program, and users reported that even the abbreviated program provided valuable, thought-provoking content.
In conclusion, we found that an iterative development strategy involving a multidisciplinary team and representative cancer patient-caregiver dyads facilitated the successful development of a novel dyadic web-based intervention. A Phase II pre-post trial is now in progress to assess the effects of this program on quality of life and other psychosocial outcomes. Future research should also explore the trade-offs of providing such interventions via different modalities, as the optimal program may take advantage of the low cost, accessible, tailoring features of the web, while offering opportunities for interaction with “real people” at key moments.
ACKNOWLEDGMENTS
Contributors: The authors thank Al Bliss and Alison Neff from the Center for Health Communications Research for their contributions to program design and the development process, respectively. Mark Newman, Paul Resnick, and Katherine Lawrence from the University of Michigan School of Information provided important guidance about usability testing procedures. Kelly Brittain from the Karmanos Cancer Center assisted us in recruitment for focus groups and usability testing. Ann Hoffman assisted with note-taking during focus groups. Finally, we greatly appreciate the valuable feedback that we received from the FOCUS intervention team, including Joan Bickes, Andrea DeAgostino, Margaret Falahee, Janet Harden, Darlene Mood, and Julie Walker.
Funders: Development of the web-based FOCUS communication program was supported through a grant from the National Cancer Institute (#R21CA138725). Dr. Zulman is supported by the Robert Wood Johnson Foundation Clinical Scholars Program and an associated VA Advanced Fellowship.
Role of the Sponsor: The funding sources had no role in the design and conduct of the study, in the collection, analysis, and interpretation of the data, or in the preparation, review, or approval of the manuscript.
Funding source: (R21 CA138725; L. Northouse PI)
Footnotes
Prior Presentations: None
Conflict of Interest: None disclosed
References
- 1.Northouse LL, Mood DW, Schafenacker A, et al. Randomized clinical trial of a family intervention for prostate cancer patients and their spouses. Cancer. 2007 Dec 15;110(12):2809–2818. doi: 10.1002/cncr.23114. [DOI] [PubMed] [Google Scholar]
- 2.Scott JL, Halford WK, Ward BG. United we stand? The effects of a couple-coping intervention on adjustment to early stage breast or gynecological cancer. J Consult Clin Psychol. 2004 Dec;72(6):1122–1135. doi: 10.1037/0022-006X.72.6.1122. [DOI] [PubMed] [Google Scholar]
- 3.Strecher VJ. Internet methods for delivering behavioral and health-related interventions (eHealth). Annual Review of Clinical Psychology. 2007;3:53–76. doi: 10.1146/annurev.clinpsy.3.022806.091428. [DOI] [PubMed] [Google Scholar]
- 4.Gibbons M, Wilson R, Samal L, et al. Impact of Consumer Health Informatics Applications. Agency for Healthcare Research and Quality; Rockville, MD: 2009. Evidence Report/Technology Assessment No. 188. [Google Scholar]
- 5.Kroeze W, Werkman A, Brug J. A systematic review of randomized trials on the effectiveness of computer-tailored education on physical activity and dietary behaviors. Ann Behav Med. 2006 Jun;31(3):205–223. doi: 10.1207/s15324796abm3103_2. [DOI] [PubMed] [Google Scholar]
- 6.Murray E, Burns J, See TS, Lai R, Nazareth I. Interactive Health Communication Applications for people with chronic disease. Cochrane Database Syst Rev. 2005;(4):CD004274. doi: 10.1002/14651858.CD004274.pub4. [DOI] [PubMed] [Google Scholar]
- 7.Dubenske LL, Chih MY, Denauer S, Gustafson DH, Cleary JF. Development and implementation of a clinician reporting system for advanced stage cancer: Initial lessons learned. Journal of the American Medical Informatics Association. 2008;15(5):679–686. doi: 10.1197/jamia.M2532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Northouse LL, Walker J, Schafenacker A, et al. A family-based program of care for women with recurrent breast cancer and their family members. Oncol Nurs Forum. 2002 Nov-Dec;29(10):1411–1419. doi: 10.1188/02.ONF.1411-1419. [DOI] [PubMed] [Google Scholar]
- 9.Harden J, Margaret F, Joan B, et al. Factors associated with prostate cancer patients’ and their spouses’ satisfaction with a family-based intervention. Cancer Nursing. 2009;32(6):482–492. doi: 10.1097/NCC.0b013e3181b311e9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lazarus RS, Folkman S, editors. Stress, appraisal, and coping. Springer; New York: 1984. [Google Scholar]
- 11.Northouse L, Kershaw T, Mood D, Schafenacker A. Effects of a family intervention on the quality of life of women with recurrent breast cancer and their family caregivers. Psychooncology. 2005 Jun;14(6):478–491. doi: 10.1002/pon.871. [DOI] [PubMed] [Google Scholar]
- 12.Hawkins RP, Kreuter M, Resnicow K, Fishbein M, Dijkstra A. Understanding tailoring in communicating about health. Health Educ Res. 2008 Jun;23(3):454–466. doi: 10.1093/her/cyn004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.McLaughlin H. [July 20, 2008];SMOG: Simple measure of gobbledygook. 2008 http://www.harrymclaughlin.com/SMOG.htm.
- 14.United States Department of Health and Human Services [May 12, 2010];Usability.gov: Your guide for developing usable & useful Web sites. 2010 http://www.usability.gov.
- 15.Bastien JM. Usability testing: a review of some methodological and technical aspects of the method. Int J Med Inform. 2009 Apr;79(4):e18–23. doi: 10.1016/j.ijmedinf.2008.12.004. [DOI] [PubMed] [Google Scholar]
- 16.Wilson C, Blostein J. Usability techniques: Pros and cons of co-participation in usability studies. Usability Interface. 1998 [Google Scholar]
- 17.Davis FD. Perceived usefulness, perceived ease of use, and user acceptance of information technology. MIS Quarterly. 1989;13:319–329. [Google Scholar]
- 18.Brooke J. SUS: a “quick and dirty” usability scale. In: Jordan PW, Thomas B, Weerdmeester BA, McClelland AL, editors. Usability Evaluation in Industry. Taylor and Francis; London: 1996. [Google Scholar]
- 19.Koyani S, Bailey R, Nall J, Allison S, Mulligan CB,K, Tolson M. [May 10, 2010];Research-based web design and usability guidelines. 2004 www.usability.gov/guidelines/guidelines_book.pdf.