Abstract
Recently, a transoral robotic-assisted technique to access the thyroid gland has been introduced. Despite the advantages this approach may have over other minimally invasive and robotic-assisted techniques, we found that the placement of the camera through the floor of mouth led to restricted freedom of movement. We describe our modification to this technique to overcome this problem. In a study using two fresh human cadavers, the camera port of the da Vinci robot was placed in the midline oral vestibule instead of the floor of the mouth. A transoral thyroidectomy and central neck dissection was successfully performed. Our modification led to an unfettered view of the central neck and allowed for a total thyroidectomy and central neck dissection. Our modification of transoral robotic-assisted thyroidectomy provides superior access to the central compartment of the neck over other robotic-assisted thyroidectomy techniques.
Electronic supplementary material
The online version of this article (doi:10.1007/s11701-011-0287-2) contains supplementary material, which is available to authorized users.
Keywords: Transoral thyroidectomy, Thyroid, Robotic-assisted surgery, Robot, Minimally invasive, Central neck
Introduction
Minimally invasive and remote access thyroid surgery continue to evolve and are playing a growing role in the management of benign and select malignant thyroid tumors. Techniques for accessing the thyroid range from minimizing the length and visibility of the cervical scar (minimally-invasive video-assisted thyroidectomy, MIVAT [1–4]) to moving the incision away from the neck altogether to where it is not perceptible (transaxillary endoscopic [5, 6] and robotic-assisted thyroidectomy [7–9]). While these techniques offer various advantages compared to traditional open transcervical thyroidectomy, limitations remain, precluding their widespread adoption for most patients. Currently, approaches must compromise between optimizing cosmesis by hiding scars in the chest and axillary region while maximizing tissue dissection and post-operative pain versus minimizing tissue dissection at the expense of a neck scar. The optimal approach to the thyroid would involve minimal tissue disruption without leaving conspicuous scars. We have recently reported a technique for accessing the central compartment of the neck and removing the thyroid with the da Vinci robot that achieves these goals [10].
Our initial cadaver experience with the da Vinci robot explored a transoral approach with a single port for the camera in the floor of the mouth and two ports for the effector arms in the lateral vestibule under the lip. While this approach was successful, camera mobility was limited by the upper and lower dentition. We present our modifications for overcoming this shortcoming and also look at the feasibility of performing a central neck dissection.
Materials and methods
Two human cadavers were obtained from the Memorial Hermann Texas Medical Center. One was female and one male, both with full dentition. The procedure was initiated as we had previously described [10] with the neck in slight extension. An incision in the floor of the mouth was made in the midline and a submental subplatysmal pocket was created. Two incisions were made in the gingival–buccal sulcus and each mental nerve was identified and dissected from the surrounding tissue for approximately 2 cm to avoid tension on the nerve during the procedure. Dissection proceeded around the mandible into the submental pocket. 8-mm bariatric cannulae were placed in the two lateral incisions and a 12-mm cannula was placed in the floor of mouth incision. Care was taken to place the cannulae posterior to the mental nerves to allow full mobility of the effector arms without applying undue tension on the nerves. The da Vinci robot was brought to the bedside at an angle of approximately 30° and the cannulae were docked. The 0° endoscope was advanced through the cannula in the midline floor of the mouth. A Maryland dissector was placed through the left gingival–buccal incision and a Harmonic scalpel was advanced through the right gingival–buccal incision. Under endoscopic visualization, the effector arms were visible; however, the camera motion was limited by its position over the maxillary and under the mandibular dentition. Both the 12- and 8-mm 0° and 30° scopes were used but adequate freedom of movement to visualize the thyroid bed was not possible due to the dentition (Fig. 1).
Fig. 1.
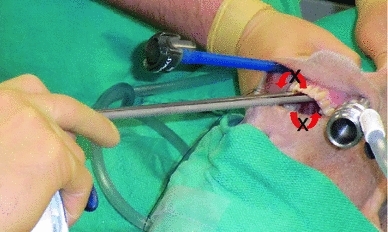
Original approach to the central neck with the endoscopic camera entering through the floor of the mouth. Rotation along the axis of the scope was precluded by the maxillary and mandibular dentition
Recognizing the limitation of this approach in a population that overwhelmingly has full dentition, we sought an alternative port position for the camera. A third gingival–buccal incision was made in the midline, leaving a cuff of mucosa to facilitate closure. The fasciculus of each levator mentalis muscle was identified and the midline was opened. Dissection continued around the inferior aspect of the mandible until the submental pocket was entered. The 12-mm cannula was placed and found to have excellent mobility around the inferior edge of the mandible without any limitation from the dentition (Fig. 2). A 12-mm 0° scope was placed and the robot was docked. CO2 insufflation at 8 L/min maintained a working cavity without the need for external retractors (Fig. 3). Superb visualization of the central cavity was obtained. The key steps of the procedure are illustrated in Fig. 4. A brief video is available on-line (LINK). The recurrent laryngeal nerve was identified and preserved, and a right thyroid lobectomy and central neck dissection was performed, the latter as defined by the borders elucidated by the American Thyroid Association’s consensus statement on central neck dissection [11]. The inferior border of the dissection was the innominate artery which was easily visualized with this approach. At the conclusion of the procedure, the neck was opened to confirm an appropriate resection (Fig. 5). The approach and dissection were repeated in the second cadaver.
Fig. 2.
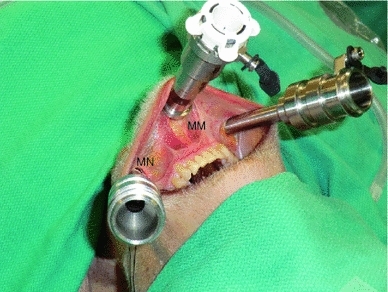
Placement of the three ports. Each lateral port was positioned posterior to the mental nerve (MN) and the camera port was placed in the midline between the fasiculus of the mentalis muscle (MM)
Fig. 3.
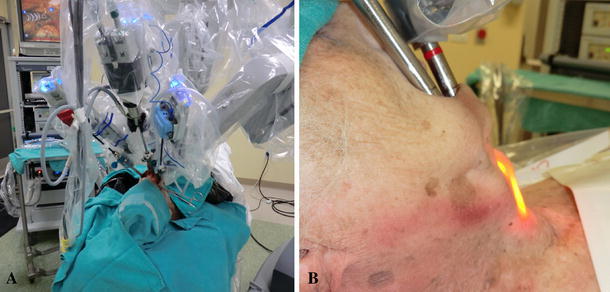
a Docking of the robot. b A view of the flexed neck demonstrating the insufflated working space and no need for external retractors
Fig. 4.
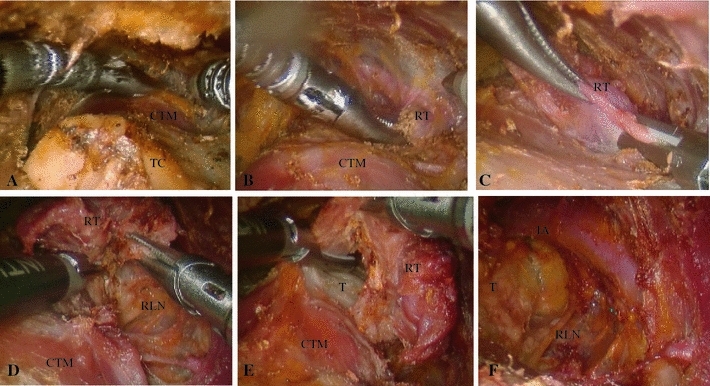
Various stages of transoral robotic-assisted thyroidectomy with central neck dissection. a Creation of working cavity with CO2 insufflation at 8 L/min. b Identification of the superior pole of the right thyroid lobe. c Division of the superior thyroid pedical with the Harmonic scalpel. d Elevation of the right thyroid lobe off the trachea and identification of the recurrent laryngeal nerve. e Division of the isthmus. f Central neck after thyroid lobectomy and lymphadenectomy demonstrating innominate artery, recurrent laryngeal nerve and trachea. TC thyroid cartilage, CTM cricothyroid muscle, RT right thyroid lobe, RLN recurrent laryngeal nerve, T trachea, IA innominate artery
Fig. 5.
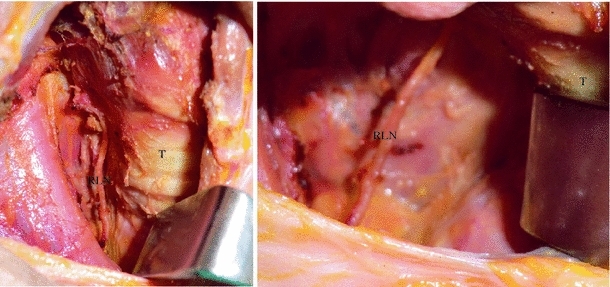
Post-operative transcervical view of the operative bed demonstrating the area of resection including a right thyroid lobectomy and central neck dissection. RLN recurrent laryngeal nerve, T trachea
Results and discussion
We recently described a transoral robotic-assisted thryoidectomy in which the endoscopic port enters the floor of mouth [10]. Although this approach was successful for the previous dentate cadaver, we were unable to maneuver the camera adequately in either of the cadavers used in this dissection due to impingement on the mandibular and maxillary teeth. This limitation, combined with concerns of complications from violating the floor of the mouth, led us to modify the approach. By moving the endoscopic port anterior to the mandible between the mentalis muscles, we were able to obtain excellent mobility without any restriction from the facial skeleton. This modification no longer limits this approach to patients with favorable dentition that would permit passage of the endoscope into the floor of mouth. Furthermore, it should avoid potential deficits in speech and swallowing by avoiding dissection through the tongue and floor of the mouth musculature. However, an anterior midline approach between the mentalis muscles has the potential to result in “puckering” or sagging of the mental subunit and cosmetic deformity of the mentum [12, 13]. Furthermore, there remains a risk to the mental nerve with the lateral gingival–buccal port placement. We found that by dissecting the nerve free from the surrounding soft tissue and placing the cannulae posterior to the nerve, there was no tension placed on the nerve during the procedure.
The transoral approach offers superb visibility of the central compartment of the neck down to the level of the innominate artery below the sternal notch. In contrast to other endoscopic and robotic-assisted approaches that have a lateral entry point, the transoral approach provides a midline exposure and equivalent access to both the right and left thyroid lobes and central compartments. This is a considerable advantage over the transaxillary technique, in which approaching the contralateral thyroid lobe or paratracheal nodal basin may be quite challenging. We believe that the view from the transoral approach is more akin to that afforded by the traditional open approach and might diminish the learning curve [14], since this approach is well known by experienced thyroid surgeons. It provides a more familiar perspective for identifying the recurrent laryngeal nerve and provides excellent exposure, allowing a complete central neck dissection. We believe the exposure afforded by this approach to the central neck is superior to that of the transaxillary approach; specifically to the deep aspects of level VI inferior to the gland and clavicle to reach the borders of a true paratracheal dissection, as we confirmed in our cadaver. Thus, transoral robotic-assisted thyroidectomy may provide the safest access to both paratracheal beds, permitting more comprehensive treatment of the posterolateral suspensory ligament of Berry, the recurrent laryngeal nerve, and any paratracheal lymphatics.
Technical challenges remain in accessing the central compartment though the mouth. The initial dissection around the inferior aspect of the mandible to create a submental subplatysmal pocket is difficult. We are continuing to explore different methods to atraumatically open this space in order to accomodate the robotic instrumentation. Smaller instrumentation and the imminent arrival of single-port technology will greatly facilitate this approach. Furthermore, the extraction of the surgical specimen though the small port incisions needs to be refined. Although further refinements in technique will be necessary before it is introduced on live human patients, the transoral robotic-assisted approach to the central compartment continues to evolve and promises to have a role in minimally invasive thyroid surgery.
Electronic supplementary material
Conflict of interest
None.
Footnotes
F. C. Holsinger contributed equally to the first author.
References
- 1.Miccoli P, et al. Minimally invasive video-assisted thyroidectomy: multiinstitutional experience. World J Surg. 2002;26(8):972–975. doi: 10.1007/s00268-002-6627-7. [DOI] [PubMed] [Google Scholar]
- 2.Miccoli P, et al. Minimally invasive video-assisted thyroidectomy. Am J Surg. 2001;181(6):567–570. doi: 10.1016/S0002-9610(01)00625-0. [DOI] [PubMed] [Google Scholar]
- 3.Miccoli P, Materazzi G. Minimally invasive, video-assisted thyroidectomy (MIVAT) Surg Clin North Am. 2004;84(3):735–741. doi: 10.1016/j.suc.2004.03.003. [DOI] [PubMed] [Google Scholar]
- 4.Terris DJ, Gourin CG, Chin E. Minimally invasive thyroidectomy: basic and advanced techniques. Laryngoscope. 2006;116(3):350–356. doi: 10.1097/01.mlg.0000191462.58630.e4. [DOI] [PubMed] [Google Scholar]
- 5.Duncan TD, et al. Endoscopic transaxillary near total thyroidectomy. JSLS. 2006;10(2):206–211. [PMC free article] [PubMed] [Google Scholar]
- 6.Miyano G, Lobe TE, Wright SK. Bilateral transaxillary endoscopic total thyroidectomy. J Pediatr Surg. 2008;43(2):299–303. doi: 10.1016/j.jpedsurg.2007.10.018. [DOI] [PubMed] [Google Scholar]
- 7.Kang SW, et al. Robotic thyroid surgery using a gasless, transaxillary approach and the da Vinci S system: the operative outcomes of 338 consecutive patients. Surgery. 2009;146(6):1048–1055. doi: 10.1016/j.surg.2009.09.007. [DOI] [PubMed] [Google Scholar]
- 8.Kang SW, et al. Robot-assisted endoscopic surgery for thyroid cancer: experience with the first 100 patients. Surg Endosc. 2009;23(11):2399–2406. doi: 10.1007/s00464-009-0366-x. [DOI] [PubMed] [Google Scholar]
- 9.Lee J, Kang SW, Jung JJ, Choi UJ, Yun JH, Nam KH, Soh EY, Chung WY (2011) Multicenter study of robotic thyroidectomy: short-term postoperative outcomes and surgeon ergonomic considerations. Ann Surg Oncol. doi:10.1245/s10434-011-1628-0 [DOI] [PubMed]
- 10.Richmon JD, et al. Transoral robotic-assisted thyroidectomy: a preclinical feasibility study in 2 cadavers. Head Neck. 2011;33(3):330–333. doi: 10.1002/hed.21454. [DOI] [PubMed] [Google Scholar]
- 11.Orloff LA, Kuppersmith RB. American Thyroid Association’s central neck dissection terminology and classification for thyroid cancer consensus statement. Otolaryngol Head Neck Surg. 2010;142(1):4–5. doi: 10.1016/j.otohns.2009.11.013. [DOI] [PubMed] [Google Scholar]
- 12.Zide BM, McCarthy J. The mentalis muscle: an essential component of chin and lower lip position. Plast Reconstr Surg. 1989;83(3):413–420. doi: 10.1097/00006534-198903000-00001. [DOI] [PubMed] [Google Scholar]
- 13.Chaushu G, et al. The effect of precise reattachment of the mentalis muscle on the soft tissue response to genioplasty. J Oral Maxillofac Surg. 2001;59(5):510–516. doi: 10.1053/joms.2001.22678. [DOI] [PubMed] [Google Scholar]
- 14.Lee J, et al. The learning curve for robotic thyroidectomy: a multicenter study. Ann Surg Oncol. 2011;18(1):226–232. doi: 10.1245/s10434-010-1220-z. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


