Abstract
BACKGROUND:
Irritable bowel syndrome (IBS) is a chronic functional bowel disorder that up to 20% of the population is suffering from it. Also benign prostatic hyperplasia (BPH) is a common problem that approximately 90 percent of men may be affected by this condition until the eighth decade of their life. Prostatectomy as a surgery and pelvic intervention can cause IBS.
METHODS:
It was a case-control study including 66 patients in 2 case groups and 66 patients in 2 control groups. Case groups were patients who underwent open prostatectomy and transurethral resection of the prostate (TURP) and control groups were patients who were candidate for prostatectomy.
RESULTS:
Ten patients in case groups and five patients in control groups had IBS. There was no significant difference in IBS between control and case groups (p = 0.117).
CONCLUSIONS:
This is the first forward study regarding bowel symptom changes following prostatectomy. The main positive finding of this study is that open prostatectomy was followed by significant increase in diarrhea and bowel habit alternation associated with onset of abdominal pain. Specifically the change was found after open operation but not after TURP. Prostatectomy whether in form of open or transurethral may cause onset of abdominal discomfort and bowel habit change.
KEYWORDS: Irritable Bowel Syndrome, Transurethral Resection of Prostate, Prostatectomy
Irritable Bowel Syndrome (IBS) is a chronic functional bowel disorder that up to 20% of the population is reported to have its symptoms and patients may suffer from it forever, but is not life threatening.1,2 The prevalence and presence of functional bowel symptoms varies between communities and a clinician frequently encounters difficulties regarding miscellaneous diagnosis of the collection of signs and symptoms that patients present in different situations.3 According to ROME criteria, a patient who suffers from IBS typically suffers from diarrhea, constipation, or a mixture of both (IBSD, IBS-C, IBS-M).4 The syndrome is a complex of problems in lower abdomen with discomfort or pain, and altered bowel habits; Association to possible psychological factors may reduce a patient's quality of life or change patients severity and frequency of IBS symptoms.5,6 IBS was previously named ulcer and some other terms such as neurogenic mucous colits,7 irritable colon syndrome8 and spastic colon.9
Benign prostatic hyperplasia (BPH) is a common problem that approximately 90 percent of men may be affected by it until the eighth decade of their life.10 Many of these cases undergo prostatectomy, in form of open or transurethral operation, after which the patient may face post-surgical symptoms initiation or aggravation.
Surgery may aggravate IBS symptoms because of abdominal or pelvic interventions or it may reduce their symptoms because surgery may work as a placebo. Post-surgical irritable bowel syndrome was reported following cholecystectomy, appendectomy and especially after pelvic operations including hysterectomy.11–14
The goal of this study was to compare the relative frequency changes in IBS symptoms in the patients underwent prostate surgery.
Methods
This study was a case-control that was conducted in Isfahan; groups included 33 transurethral resection of the prostate (TURP) patients (Group A) and 33 patients who underwent open prostatectomy (Group B); the cases were interviewed from 12 weeks to 12 months after undergoing surgery (a total of 66 patients in case groups). A three-month lag to recruit the patients was set because primary symptoms of surgery might be recovered after 3 months and IBS symptoms would occur during these months after surgery.
Control groups were formed by enrollment of 33 TURP candidate patients (Group C) and 33 cases that were candidate for open prostatectomy (Group D). Both of these groups were interviewed before their operation.
Patients in both case and control groups were divided into two subgroups of middle aged (age ≤ 64) and old (age > 65).
Patients in both case and control groups were selected using convenience time-based sequential sampling method from a single academic center where they were under treatment by a unique urology surgeon. Those with history of prostatic malignancy, chemotherapy or radiotherapy, operation on abdominal or pelvic region as well as those with any positive findings indicating malignant prostatic disease, even during the current illness before and after prostatectomy, were excluded. Major psychiatric problems were ruled out by direct interview as well as reviewing medical history.
The project was approved by the Organizational Research Governance Council as well as the Regional Bioethics Committee. All cases were informed about the objectives of the study and enrolled after getting consent. The patients were interviewed in outpatient setting along with their routine follow-up consultation visit.
A structured interview was designed for data gathering and performed by one of the research teams using field coding. The questions covered irritable bowel syndrome criteria according to ROME guidelines including diarrheal symptoms, constipation, pain and discomfort initiation or aggravation.
To categorize the data of questionnaires, responses of instances were divided into negative where the answers were never or seldom and positive in the case of other answers. Quantitative variables were compared and analyzed between groups using t-test; in the case of need for non-parametric tests due to small sample size and similar problems, Mann-Whitney-U test was substituted. chi-square and Fisher's exact tests were used to study qualitative variables. For ordinal factors Spearman test was utilized. In all parts p < 0.05 was considered as significant.
Results
Mean age in case groups was 68.7 years (range: 51-84) and in control groups was 70.9 years (SD = 8.64, range: 52-79). No statistically significant difference was seen between them.
Ten patients in case groups (Group A and Group B) and 5 patients (8%) in control groups (Group C and Group D) had IBS. Data were analyzed using chi-square test and there was no significant difference in IBS between control and case groups (p = 0.117, Odd's Ratio = 2.18). Seven out of ten patients in case groups were from group A and the other 3 was from group B. Using the Fisher's exact test, no significant difference was revealed in relative frequency of IBS between control groups and group A (p = 0.98, Odd's Ratio CI 95% = 0.954-11.306); also there was no significant difference in definite IBS between control groups and group B (p = 1.00, Odd's Ratio CI 95% = 0.273-5.449).
Table 1 shows answers of control and case groups to questions regarding presence of functional bowel symptoms. On the basis of collected data, Spearman test was used and relative frequency of diarrhea in case groups were found to be significantly higher than control groups (p = 0.012, Odd's Ratio = 1.75). Control groups’ data were compared separately with group A and group B. Relative frequency of post-operative diarrhea in the patients who underwent open prostatectomy was higher than the control groups (p = 0.034, Odd's Ratio = 3.06). No significant difference in relative frequency of diarrhea was found between control groups and group B (patients underwent TURP) (p = 0.87, Odd's Ratio = 0.92). Within the case groups, the relative frequency of post-operative diarrhea was higher in group A (patients underwent open prostatectomy) than the group B (patients underwent TURP) (p = 0.026, Odd's Ratio = 0.30).
Table 1.
Frequency distribution of bowel symptoms in patients with BPH before and after surgery
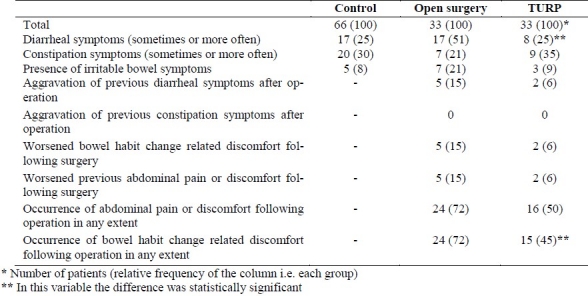
No significant differences in relative frequency of constipation were found between case groups and control groups (p = 0.61, Odd's Ratio = 0.74). Constipation was reported to be seen in similar extend by both open prostatectomy and TURP group (p = 0.632, Odd's Ratio = 0.72).
One part of the study referred to the onset of abdominal pain related with defecation in patients; no significant difference was seen between subgroup A and subgroup B in this regard (p = 0.87, Odd's Ratio = 0.92). Three patients in open prostatectomy group reported feeling better regarding these symptoms following surgery whereas in TURP group no one felt better.
Aggravation of functional bowel symptoms, including diarrhea, abdominal pain and bowel habit alternation was evaluated in the case groups between open prostatectomy subgroup and TURP subgroup after surgery and no significant difference in symptoms alteration was found (p = 0.427, Odd's Ratio = 2.77), except for occurrence of bowel habit change after surgery that were higher in open surgery group.
Twenty patients were middle aged and forty six patients were old in case groups; twenty two patients in control groups were middle aged and forty four were old. There was no significant difference between groups regarding patients’ ages (p = 0.70, Odd's Ratio = 0.87). Then association of age with bowel symptoms aggravation was evaluated by chi-square test. Aggravation of functional bowel symptoms after surgery was reported by three middle aged patients while four old patients reported this change too. No statistically significant difference in IBS symptoms aggravation between middle aged and old patients was found (p = 0.425, Odd's Ratio CI 95% = 0.109-2.672).
Discussion
The main idea of this study was to determine the association between prostate surgery and change in functional bowel symptoms. In our knowledge, although the study sample was small, this is the first forward study regarding bowel symptom changes following prostatectomy; it is also notable that the present study compared minimally invasive versus routine surgery. Also to cover possible limitations, the control groups were selected from the same population that the case groups came from.
The instances in case groups were recruited 3 months after the surgery15; this time range was chosen since the initial stressful period should be passed before evaluating the patient for chronic pain and symptoms following operation. Also according to most of routine criteria of functional bowel disorders 12 weeks continuity4 is the least acceptable time period to fulfill the definitions.
It was previously reported in other cross-sectional studies that functional bowel symptoms were significantly correlated with history of abdominopelvic surgery; within these operations cholecystectomy was the most prevalent and those with irritable bowel symptoms had four fold history of gallbladder operation.14 These type of studies had a temporal ambiguity of causality relationships.
The main positive finding of this study is that open prostatectomy was followed by significant increase in diarrhea and bowel habit alternation associated with onset of abdominal pain. Specifically the change was found after open operation but not after TURP. As it could be seen in table 1, other bowel functional symptoms may also be altered after open prostatectomy but the main limitation of the present study was the limited sample size which would limit the power of the statistical tests to show the real differences. This is the problem of forward or prospective post-surgical functional bowel disorders studies and is related to difficulty of case finding and follow-up.16 It is also interesting that the majority of patients faced new functional problems after surgery especially after open operation although the symptoms may be minor or short term in most of them and will not extend for a long time as a chronic disorder.
One assumption for development of post-surgical bowel functional changes is an inflammatory process in the pelvic region that involves sensory nerves of this region with activation of mast cells and consequently visceral hypersensitivity.17
Other explanation of these functional bowel changes is triad of psychological stress, early post-operative pain and psychological background of the patient. It was considered that the higher is the psychological catastrophe related pain following surgery, the more would functional bowel be changed.18 Surely one of the main preventive means would be reducing pain and anxiety due to surgery that predispose the patients to consequent complications. It is more important in those with possible psychological backgrounds that are more prone to develop symptoms.19
Prostatectomy is similar to hysterectomy in some extend, since it is a pelvic surgery, relates with genital organs and possibly with personal gender-related body-image and identity and is done after youth period. Of course it is different in some aspects: extension of the operation and possible nerve manipulation, patients’ gender and its related psychological backgrounds, and age of the patients; But it is assumed that due to lack of data regarding postprostatectomy bowel function changes, hysterectomy-related studies may be considered as a similar model.
In the patients underwent open prostatectomy, surgery led to increase in relative frequency of diarrhea and bowel habit alternation associated with onset of abdominal pain. The present data are in agreement with van Dam study on bowel habit alteration, In which, hysterectomy was followed by a significant increase in the incidence of disturbed bowel function.20 But the report by Heaton emphasized on higher prevalence of constipation and defecation problems in hysterectomized patients.21
Previous reports showed that those with IBS who underwent operation may develop more pain and will have worse symptoms.22 Although for some IBS patients, surgery may have a placebo effect on their pain and discomfort symptoms and even recovery from IBS may occur.23 Previously, in an interesting study, it was reported that in 60% of cases, patients’ would relief from pain and discomfort after hysterectomy. To explain the etiology of changing symptoms in these patients, the author raised the idea of “non-IBS” related symptoms and real somatic effect of surgery on relief; Also placebo effect was mentioned in the causality chain of recovery.24 Similar changes in bowel symptoms were reported in minor proportion of the current open surgery group (3 out of 33); if 10 percent would be considered as the acceptable error of the tests, abdominal surgery aggravate symptoms in patients with functional bowel discomfort.
On the other hand the present study revealed no increase or decrease in irritable bowel syndrome incidence or severity after surgery whereas hysterectomy was found to be a possible risk factor for definite IBS. Although, if referring to data presented in table 1 regarding initiation of new pain or discomfort, it might be understood that in both groups of post-prostatectomy patients, pain or discomfort presents in large extend, although due to possible methodological limitations and small sample size, demonstration of definite IBS increment was impossible in this study.
Conclusions
In conclusion, it seems that prostatectomy, in both forms of open and transurethral, may cause onset of abdominal discomfort and bowel habit change that may resolve in time but significantly may induce bowel habit change in form of diarrheal symptoms. Further large scale studies may reveal these findings better.
Authors’ Contributions
PA and HM carried out the design, coordinated the study, and participated in most of the experiments. PA and AT prepared the manuscript. AD provided assistance in the design of the study, coordinated and carried out all the experiments and participated in manuscript preparation. AT provided assistance for all experiments. All authors have read and approved the content of the manuscript.
Acknowledgments
The authors wish to thank Dr. Imad Adibi for his assistance in statistical analysis.
Footnotes
Conflict of Interests
Authors have no conflict of interests.
References
- 1.Sandler RS. Epidemiology of irritable bowel syndrome in the United States. Gastroenterology. 1990;99(2):409–15. doi: 10.1016/0016-5085(90)91023-y. [DOI] [PubMed] [Google Scholar]
- 2.Camilleri M, Choi MG. Review article: irritable bowel syndrome. Aliment Pharmacol Ther. 1997;11(1):3–15. doi: 10.1046/j.1365-2036.1997.84256000.x. [DOI] [PubMed] [Google Scholar]
- 3.Adibi P, Behzad E, Pirzadeh S, Mohseni M. Bowel habit reference values and abnormalities in young Iranian healthy adults. Dig Dis Sci. 2007;52(8):1810–3. doi: 10.1007/s10620-006-9509-2. [DOI] [PubMed] [Google Scholar]
- 4.Drossman DA. Rome III: the new criteria. Chin J Dig Dis. 2006;7(4):181–5. doi: 10.1111/j.1443-9573.2006.00265.x. [DOI] [PubMed] [Google Scholar]
- 5.Hahn BA, Yan S, Strassels S. Impact of irritable bowel syndrome on quality of life and resource use in the United States and United Kingdom. Digestion. 1999;60(1):77–81. doi: 10.1159/000007593. [DOI] [PubMed] [Google Scholar]
- 6.Drossman DA. Review article: an integrated approach to the irritable bowel syndrome. Aliment Pharmacol Ther. 1999;13(Suppl 2):3–14. doi: 10.1046/j.1365-2036.1999.0130s2003.x. [DOI] [PubMed] [Google Scholar]
- 7.Bockus HL, Bank J, Wilkinson SA. Neurogenic mucous colitis. Am J Med Sci. 1928;176(6):813–29. [Google Scholar]
- 8.Chaudhary NA, Truelove SC. The irritable colon syndrome: a study of the clinical features, predisposing causes, and prognosis in 130 cases. Q J Med. 1962;31(123):307–22. [PubMed] [Google Scholar]
- 9.Ryle JA. An address on chronic spasmodic affections of the colon and diseases which they simulate. Lancet. 1928;212(5492):1115–9. [Google Scholar]
- 10.Bosch JL, Hop WC, Kirkels WJ, Schröder FH. Natural history of benign prostatic hyperplasia: appropriate case definition and estimation of its prevalence in the community. Urology. 1995;46(3 Suppl A):34–40. doi: 10.1016/s0090-4295(99)80248-9. [DOI] [PubMed] [Google Scholar]
- 11.Filip M, Saftoiu A, Popescu C, Gheonea DI, Iordache S, Sandulescu L, et al. Postcholecystectomy syndrome - an algorithmic approach. J Gastrointestin Liver Dis. 2009;18(1):67–71. [PubMed] [Google Scholar]
- 12.McNally MA, Locke GR, Zinsmeister AR, Schleck CD, Peterson J, Talley NJ. Biliary events and an increased risk of new onset irritable bowel syndrome: a population-based cohort study. Aliment Pharmacol Ther. 2008;28(3):334–43. doi: 10.1111/j.1365-2036.2008.03715.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lu CL, Liu CC, Fuh JL, Liu PY, Wu CW, Chang FY, et al. Irritable bowel syndrome and negative appendectomy: a prospective multivariable investigation. Gut. 2007;56(5):655–60. doi: 10.1136/gut.2006.112672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Longstreth GF, Yao JF. Irritable bowel syndrome and surgery: a multivariable analysis. Gastroenterology. 2004;126(7):1665–73. doi: 10.1053/j.gastro.2004.02.020. [DOI] [PubMed] [Google Scholar]
- 15.Perkins FM, Kehlet H. Chronic pain as an outcome of surgery.A review of predictive factors. Anesthesiology. 2000;93(4):1123–33. doi: 10.1097/00000542-200010000-00038. [DOI] [PubMed] [Google Scholar]
- 16.Sperber AD, Morris CB, Greemberg L, Bangdiwala SI, Goldstein D, Sheiner E, et al. Development of abdominal pain and IBS following gynecological surgery: a prospective, controlled study. Gastroenterology. 2008;134(1):75–84. doi: 10.1053/j.gastro.2007.10.041. [DOI] [PubMed] [Google Scholar]
- 17.Barbara G, Wang B, Stanghellini V, de Giorgio R, Cremon C, Di Nardo G, et al. Mast cell-dependent excitation of visceral-nociceptive sensory neurons in irritable bowel syndrome. Gastroenterology. 2007;132(1):26–37. doi: 10.1053/j.gastro.2006.11.039. [DOI] [PubMed] [Google Scholar]
- 18.Granot M, Ferber SG. The roles of pain catastrophizing and anxiety in the prediction of postoperative pain intensity: a prospective study. Clin J Pain. 2005;21(5):439–45. doi: 10.1097/01.ajp.0000135236.12705.2d. [DOI] [PubMed] [Google Scholar]
- 19.Borly L, Anderson IB, Bardram L, Christensen E, Sehested A, Kehlet H, et al. Preoperative prediction model of outcome after cholecystectomy for symptomatic gallstones. Scand J Gastroenterol. 1999;34(11):1144–52. doi: 10.1080/003655299750024968. [DOI] [PubMed] [Google Scholar]
- 20.van Dam JH, Gosselink MJ, Drogendijk AC, Hop WC, Schouten WR. Changes in bowel function after hysterectomy. Dis Colon Rectum. 1997;40(11):1342–7. doi: 10.1007/BF02050820. [DOI] [PubMed] [Google Scholar]
- 21.Heaton KW, Parker D, Cripps H. Bowel function and irritable bowel symptoms after hysterectomy and cholecystectomy -- a population based study. Gut. 1993;34(8):1108–11. doi: 10.1136/gut.34.8.1108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Longstreth GF, Preskill DB, Youkeles L. Irritable bowel syndrome in women having diagnostic laparoscopy or hysterectomy: relation to gynecologic features and outcome. Dig Dis Sci. 1990;35(10):1285–90. doi: 10.1007/BF01536421. [DOI] [PubMed] [Google Scholar]
- 23.Klein KB. Controlled treatment trials in the irritable bowel syndrome: a critique. Gastroenterology. 1988;95(1):232–41. doi: 10.1016/0016-5085(88)90319-8. [DOI] [PubMed] [Google Scholar]
- 24.Prior A, Stanley KM, Smith AR, Read NW. Relation between hysterectomy and the irritable bowel: a prospective study. Gut. 1992;33(6):814–7. doi: 10.1136/gut.33.6.814. [DOI] [PMC free article] [PubMed] [Google Scholar]


