Abstract
BACKGROUND:
The symptoms of irritable bowel syndrome (IBS) are common in the general population. The aim of this population-based study was to determine the prevalence of IBS and describe the associated factors including demographic, life style and health-seeking behaviors in Shiraz city, southern Iran.
METHODS:
From April to September 2004, 1978 subjects aged > 35 years old completed a validated and reliable questionnaire on IBS.
RESULTS:
The prevalence rate of IBS was 10.9%, higher in females, in 35-44 years old age group and among subjects eating fast food (14.1%) but was lower in those taking more fruits and vegetables (10.5%). The occurrence of anxiety, nightmare and restlessness was also significantly higher in subjects with IBS. It had an association with psychological distress and recurrent headaches but not with drinking tea/coffee, smoking or physical activity.
CONCLUSIONS:
In our area, IBS was correlated with gender, age, psychological distress, recurrent headaches and consumption of fast foods that necessitate health planning programs by health policy makers.
KEYWORDS: Irritable Bowel Syndrome, Prevalence, Demography, Life Style, Health Behavior
Irritable bowel syndrome (IBS) comprises 40% of outpatient consultations1 and 15% of adults in western countries.2 In US, IBS accounts for 3.5 million annual visits, costing about 8 billion USD.3
IBS, a gastrointestinal disorder with key pathophysiological features of disordered gut motility and visceral sensitivity, is usually painful and disabling.4 It is associated with major psychological and psychiatric elements5 and is characterized by abdominal pain and disturbed defecation.3 Symptoms are common in general population but a minority of patients may receive a doctor's advice.6,7
IBS is a chronic widespread disease often with severe consequences.8 Persons with IBS usually demonstrate impaired health-related quality of life9–11 affecting the patient's every day life.12–14 At five-year follow-ups, 5% re-ported complete and about 30% partial recovery.15 Women are affected more and in 50% of patients, symptoms start before 35 years of age while almost all report symptoms onset before they are 50.16 Here, we investigated the prevalence of IBS and the associated factors in Shiraz, southern Iran. We have previously reported the prevalence of gastroesophageal reflux disease (15.4%)17 and subjective lactose intolerance (28.4%)18 in this population.
Methods
From April to September 2004, using cluster random sampling method, 3600 subjects were enrolled based on postal code divisions of 17 districts in Shiraz, southern Iran. Each subject was invited to refer to Mottahari Clinic of Gastroenterohepatology Research Center affiliated to Shiraz University of Medical Sciences. The study received the approval from institution's Ethics Committee and a written consent was provided from each participant. Then, 1978 subjects that were of both genders, older than 35 years and from both urban and rural areas completed the questionnaire. The questionnaire had four sections of demographic factors, lifestyle, symptoms of IBS, and healthseeking behavior and a gastroenterologist completed the clinical questions. The reliability and validity of the questionnaire were calculated by inviting 100 subjects for a further interview. Rome II criteria were applied to identify IBS subjects.19 IBS was defined as abdominal pain recurring over a period of more than three months in the prior year with symptoms described by Tally et al.20 The variables were age, gender, habitat, marital status, educational level, BMI (weight in kg in the fasting state divided by the square of the height in meters resulting in five categories of thin [18 kg/m2], normal [18-24.9 kg/m2], overweight [25-29.9 kg/m2], obese [30-40 kg/m2] and very obese [40 kg/m2]), physical activity (at least 30 min/week or sufficient to produce adequate sweating), dietary habits, cigarette smoking, alcohol, coffee and tea consumption, and the use of aspirin and NSAIDs. Rural and urban residence areas were defined by the size of the habitat region (under 30000 inhabitants vs. 30000 inhabitants or more). Statistical analysis was performed using SPSS software (version 11.5) and two-sided Chi-Square test. A p value less than 0.05 was considered significant.
Results
The response rate was 54.9%. The mean age of subjects was 49.90 ± 11.14 years among whom, 39.7%, 29.7%, 17.2% and 13.5% of the participants were respectively in 35-44, 45-54, 55-64 and > 65 years age groups; 56.6% lived in urban regions; 29.4% were male and 21.2%, 31.2%, 38.1% and 9.5% of the subjects were illiterate, or with primary, high school and university educational levels, respectively. The reliability of the questionnaire was 82% while the validity was 70%.
The prevalence rate of IBS was 10.9% (215 subjects). The IBS patients included 82 subjects (38.1%) with mild, 81 (37.7%) with moderate and 37 (17.2%) with severe disease, while in 15 patients (7.0%), the severity was unknown. Table 1 demonstrates the prevalence regarding demographic data, showing that IBS was more prevalent in 35-44 years old age group (13.28%, p = 0.013) and females (12.7%, p = 0.001). IBS was correlated with psychological distress (23.5%, p = 0.001) and recurrent headaches (21.4%, p = 0.001), but had no association with education, habitat, marital status, or BMI.
Table 1.
Prevalence of IBS according to different characteristics of subjects in Shiraz, southern Iran (n = 1978)
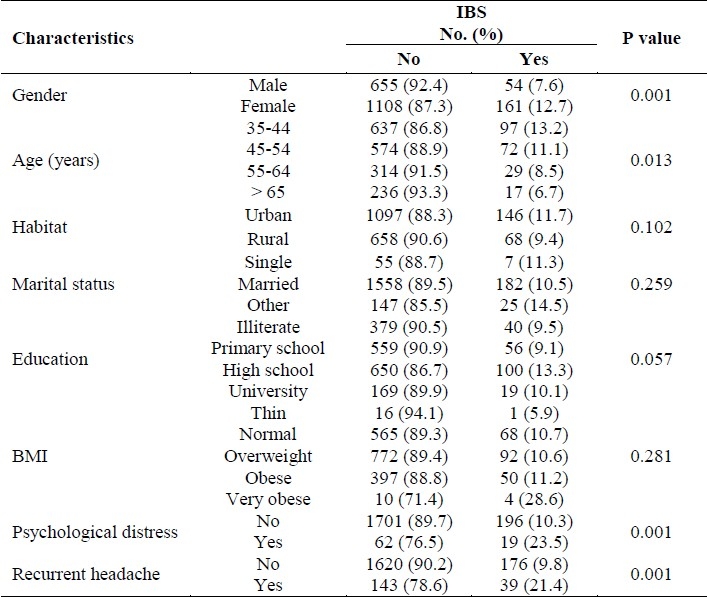
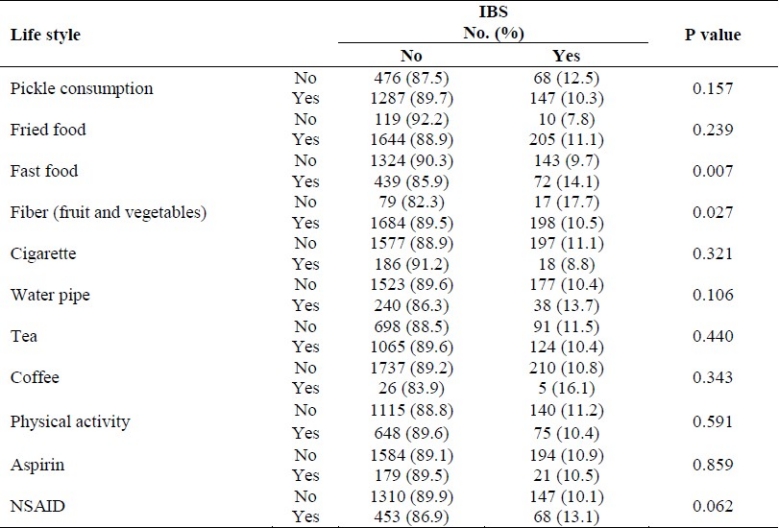
Table 2 depicts the prevalence of IBS according to dietary habits and life style. The results denotes to a higher prevalence in subjects consuming fast food (14.1%, p = 0.007) but a lower prevalence in those taking more fruits and vegetables (10.5%, p = 0.027). IBS had no correlation with drinking tea/coffee, smoking, physical activity or taking aspirin/NSAID.
Table 2.
Prevalence of IBS according to dietary habits and lifestyle of subjects in Shiraz, southern Iran (n = 1978)
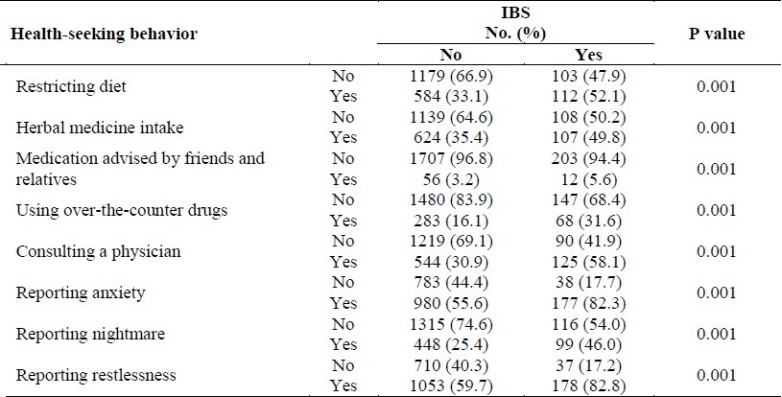
Subjects with IBS restricted their diets (16.1%, p = 0.001), used herbal therapies (14.6%, p = 0.001) and over-the-counter (OTC) medicines (19.4%, p = 0.001), consulted with physicians (18.7%, p = 0.001), and consumed medication recommended by their friends (17.6%, p = 0.001). They significantly experienced more anxiety (15.3%, p = 0.001), nightmare (18.1%, p = 0.001) and restlessness (14.5%, p = 0.001; Table 3).
Table 3.
Health-seeking behavior of subjects with IBS in Shiraz, southern Iran (n = 1978)
Discussion
Our prevalence rate is consistent with the findings of Halder et al in UK who reported a prevalence of 10.5%.21 Jones and Lydeard also showed a 10-20% prevalence in adult general population aged 20-90 in southern England.6 In Denmark, the prevalence ranged from 5 to 65%.15 IBS prevalence was 12.1% in Canada,22 14% in Pakistan,23 and 16.8% in South Korea.24 In France in subjects aged ≥ 18 years old, a prevalence of 1.1% was reported.25 The wide range of prevalence rates may be the consequence of cultural differences26 as well as different methodologies.24 In our study, gender, age, psychological distress, and recurrent headaches were correlated factors. Female to male ratios varied from 1:1 to > 2:1 throughout different reports.27 Han et al28 noticed that gender had no significant relation with IBS prevalence, Jafri et al23 reported a higher prevalence in 16-30 years old men and we found more prevalence in females which is in agreement with Park et al study.24 Similar trends were observed in France with a female to male ratio of 2.3.25 The differences in physiological sex-related status and in the autonomic and perceptual response to stress and pain may be responsible for variations in prevalence.29 Factors influencing gender differences include the sex role, response to behavioral stress, menstrual cycle, and affective symptoms.30 Men and women with IBS vary in activating brain networks of cognitive and autonomic responses to deliver and anticipate aversive visceral stimuli.27 Among our participants, the prevalence decreased as the age increased and the disease was more common in the youngest age group. Similarly, IBS prevalence was higher among Korean subjects in their 20's.28 Ruigómez et al31 noticed more prevalence in young and middle-aged population. In Nigeria, however, IBS was significantly associated with the increase of age.32
Habitat had no significant relation with occurrence of IBS in our study which is identical to Jafri et al23 who reported IBS in both urban and suburban communities in Pakistan. While we found no correlation with educational status, Celebi et al33 pointed out that IBS was higher in illiterate persons and lower in those with university degree. In another study, education was correlated with IBS prevalence.34
We observed a significantly higher prevalence of psychological distress in subjects with IBS. Moreover, IBS was more in subjects with anxiety, nightmares and restlessness (Table 3). In Nicholl et al35 study, anxiety and sleep problems were independent predictors of IBS onset. According to Secondulfo et al,36 50% of IBS patients described a stressful job and family disease, while IBS was significantly associated with depression in Nigeria.32
IBS was more prevalent in subjects with recurrent headaches (21.4%). This is consistent with the study by Si et al37 where 29.0% of IBS patients presented with headache. Similarly, complaint of headache was significantly more frequent in patients with IBS.38
With regards to dietary habits and life style of our subjects, IBS was significantly more in those who ate fast food but less common in the group with fruits and vegetables intake. The high fat content of fast foods, the spices used, and beverages typically consumed along with these foods, might explain this correlation. On the other hand, consumption of fruits and vegetables which have high fiber-contents seems to play a protective role in IBS. We found no correlation between IBS and pickle consumption, fried foods, cigarette or water-pipe smoking, tea or coffee consumption, and physical activity.
We observed a significant relationship between IBS symptoms and consulting a physician (58.1%). In France, 83.7% of IBS patients consulted a health-care practitioner for their condition25 whereas in Malaysia, 13.1% consulted their physician.38 Ringström et al found that mental health and poor social, emotional and physical functioning were independent predictors of being a healthcare seeker while mild symptoms and ability to control symptoms were reasons for not seeking healthcare.39 Moreover, our IBS patients restricted their diets, took herbal medicine, used over-the-counter (OTC) drugs, and consumed medication recommended by their friends. According to Tan et al,38 20.2% of IBS patients reported self-medication. In another study, 50% had sought alternative care or advice from friends and/or relatives.39
Conclusions
Prevalence of IBS defined by ROME II criteria was 10.9% in Shiraz, southern Iran, higher in females, younger individuals, consumers of fast food, and in subjects with psychological distress and recurrent headaches. There was no association between IBS and drinking tea/coffee, smoking or physical activity. Our results may help health policy makers in the area with their health programs.
Authors’ Contributions
MSF carried out the design and finalized the article. FK and DM prepared the manuscript and supervised the study. MN and MB participated in data collection. STH analyzed the data. AM participated in the design of the study. MS and NZ designed the questionnaire. All authors have read and approved the content of the manuscript.
Acknowledgments
Authors want to thank Mr. Saeed Amirzadehfard and the laboratory personnel of Gastroenterohepatology Research Center for their assistance in the project. This study was funded by Office of Vice Chancellor for Research of Shiraz University of Medical Sciences (Grant No. 1771).
Footnotes
Conflict of Interests
Authors have no conflict of interests.
References
- 1.Neal KR, Hebden J, Spiller R. Prevalence of gastrointestinal symptoms six months after bacterial gastroenteritis and risk factors for development of the irritable bowel syndrome: postal survey of patients. BMJ. 1997;314(7083):779–82. doi: 10.1136/bmj.314.7083.779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Drossman DA, Li Z, Andruzzi E, Temple RD, Talley NJ, Thompson WG, et al. U.S. householder survey of functional gastrointestinal disorders. Prevalence, sociodemography, and health impact. Dig Dis Sci. 1993;38(9):1569–80. doi: 10.1007/BF01303162. [DOI] [PubMed] [Google Scholar]
- 3.Tally NJ, Gabriel SE, Harmsen WS, Zinsmeister AR, Evans RW. Medical cost in community subjects with irritable bowel syndrome. Gastroenterology. 1995;109(6):1736–41. doi: 10.1016/0016-5085(95)90738-6. [DOI] [PubMed] [Google Scholar]
- 4.Drossman DA, Creed FH, Olden KW, Svedlund J, Toner BB, Whitehead WE. Psychological aspects of the functional gastrointestinal disorders. Gut. 1999;45(Suppl II):II25–30. doi: 10.1136/gut.45.2008.ii25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Walker EA, Roy-Byrne PP, Katon WJ, Li L, Amos D, Jiranek G. Psychiatric illness and irritable bowel syndrome: a comparison with inflammatory bowel disease. Am J Psychiatry. 1990;147(12):1656–61. doi: 10.1176/ajp.147.12.1656. [DOI] [PubMed] [Google Scholar]
- 6.Jones R, Lydeard S. Irritable bowel syndrome in the general population. BMJ. 1992;304(6819):87–90. doi: 10.1136/bmj.304.6819.87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Thompson WG, Heaton KW, Smyth GT, Smyth C. Irritable bowel syndrome in general practice: prevalence, characteristics, and referral. Gut. 2000;46(1):78–82. doi: 10.1136/gut.46.1.78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hahn B, Yan S, Strassels S. Impact of irritable bowel syndrome on quality of life and resource use in the United States and United Kingdom. Digestion. 1999;60(1):77–81. doi: 10.1159/000007593. [DOI] [PubMed] [Google Scholar]
- 9.Dean BB, Aguilar D, Barghout V, Kahler KH, Frech F, Groves D, et al. Impairment in work productivity and health related quality of life in patients with IBS. Am J Manag Care. 2005;11(1 Suppl):S17–26. [PubMed] [Google Scholar]
- 10.EL-Serag HB. Impact of irritable bowel syndrome: prevalence and effect on health related quality of life. Rev Gastroenterol Disord. 2003;3(Suppl 2):S3–11. [PubMed] [Google Scholar]
- 11.EL-Serag HB, Olden K, Bjorkman D. Health related quality of life among persons with irritable bowel syndrome: a systemic review. Aliment Pharmacol Ther. 2002;16(6):1171–85. doi: 10.1046/j.1365-2036.2002.01290.x. [DOI] [PubMed] [Google Scholar]
- 12.Longstreth GF, Bolus R, Naliboff B, Chang L, Kulich KR, Carlsson J, et al. Impact of irritable bowel syndrome on patients lives: development and psychometric documentation of a diseases-specific measure for use in clinical trials. Eur J Gastroenterol Hepatol. 2005;17(4):411–20. doi: 10.1097/00042737-200504000-00004. [DOI] [PubMed] [Google Scholar]
- 13.Hulisz D. The burden of illness of irritable bowel syndrome: current challenges and hope for the future. J Manag Care Pharm. 2004;10(4):299–309. doi: 10.18553/jmcp.2004.10.4.299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pace F, Molteni P, Bollani S, Sarzi-Puttini P, Stockbrügger R, Bianchi Porro G, et al. Inflammatory bowel disease versus irritable bowel syndrome: a hospital-based, case control study of disease impact on quality of life. Scand J Gastroentrol. 2003;38(10):1031–8. doi: 10.1080/00365520310004524. [DOI] [PubMed] [Google Scholar]
- 15.Kay L, Jørgensen T, Jensen KH. The epidemiology of irritable bowel syndrome in a random population: prevalence, incidence, natural history and risk factors. J Intern Med. 1994;236(1):23–30. doi: 10.1111/j.1365-2796.1994.tb01115.x. [DOI] [PubMed] [Google Scholar]
- 16.Maxwell PR, Mendall MA, Kumar D. Irritable bowel syndrome. Lancet. 1997;350(9092):1691–5. doi: 10.1016/s0140-6736(97)05276-8. [DOI] [PubMed] [Google Scholar]
- 17.Saberi-Firoozi M, Khademolhosseini F, Yousefi M, Mehrabani D, Zare N, Heydari ST. Risk factors of gastroesophageal reflux disease in Shiraz, southern Iran. World J Gastroenterol. 2007;13(41):5486–91. doi: 10.3748/wjg.v13.i41.5486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Saberi-Firoozi M, Khademolhosseini F, Mehrabani D, Yousefi M, Salehi M, Heidary ST. Subjective lactose intolerance in apparently healthy adults in southern Iran: is it related to irritable bowel syndrome? Indian J Med Sci. 2007;61(11):591–7. [PubMed] [Google Scholar]
- 19.Tally NJ, Boyce P, Jones M. Predictors of health care seeking for irritable bowel syndrome: a population based study. Gut. 1997;41(3):394–8. doi: 10.1136/gut.41.3.394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Tally NJ, Boyce P, Jones M. Identification of distinct upper and lower gastrointestinal symptom groupings in an urban population. Gut. 1998;42(5):690–5. doi: 10.1136/gut.42.5.690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Halder SL, Locke GR, 3rd, Schleck CD, Zinsmeister AR, Talley NJ. Influence of alcohol consumption on IBS and dyspepsia. Neurogastroenterol Motil. 2006;18(11):1001–8. doi: 10.1111/j.1365-2982.2006.00815.x. [DOI] [PubMed] [Google Scholar]
- 22.Thompson WG, Irvine EJ, Pare P, Ferrazzi S, Rance L. Functional gastrointestinal disorders in Canada: first population-based survey using Rome II criteria with suggestions for improving the questionnaire. Dig Dis Sci. 2002;47(1):225–35. doi: 10.1023/a:1013208713670. [DOI] [PubMed] [Google Scholar]
- 23.Jafri W, Yakoob J, Jafri N, Islam M, Ali QM. Irritable bowel syndrome and health seeking behaviour in different communities of Pakistan. J Pak Med Assoc. 2007;57(6):285–7. [PubMed] [Google Scholar]
- 24.Park KS, Ahn SH, Hwang JS, Cho KB, Chung WJ, Jang BK, et al. A survey about irritable bowel syndrome in South Korea: prevalence and observable organic abnormalities in IBS patients. Dig Dis Sci. 2008;53(3):704–11. doi: 10.1007/s10620-007-9930-1. [DOI] [PubMed] [Google Scholar]
- 25.Bommelaer G, Dorval E, Denis P, Czernichow P, Frexinos J, Pelc A, et al. Prevalence of irritable bowel syndrome in the French population according to the Rome I criteria. Gastroenterol Clin Biol. 2002;26(12):1118–23. [PubMed] [Google Scholar]
- 26.Matheis A, Martens U, Kruse J, Enck P. Irritable bowel syndrome and chronic pelvic pain: a singular or two different clinical syndrome? World J Gastroenterol. 2007;13(25):3446–55. doi: 10.3748/wjg.v13.i25.3446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Naliboff BD, Berman S, Chang L, Derbyshire SW, Suyenobu B, Vogt BA, et al. Sex-related differences in IBS patients: central processing of visceral stimuli. Gastroentrology. 2003;124(7):1738–47. doi: 10.1016/s0016-5085(03)00400-1. [DOI] [PubMed] [Google Scholar]
- 28.Han SH, Lee OY, Bae SC, Lee SH, Chang YK, Yang SY, et al. Prevalence of irritable bowel syndrome in Korea: population-based survey using the Rome II criteria. J Gastroenterol Hepatol. 2006;21(11):1687–92. doi: 10.1111/j.1440-1746.2006.04269.x. [DOI] [PubMed] [Google Scholar]
- 29.Camilleri M. Management of the irritable bowel syndrome. Gastronetrology. 2001;120(3):652–68. doi: 10.1053/gast.2001.21908. [DOI] [PubMed] [Google Scholar]
- 30.Chang L, Heitkemper MM. Gender differences in irritable bowel syndrome. Gastroenterology. 2002;123(5):1686–701. doi: 10.1053/gast.2002.36603. [DOI] [PubMed] [Google Scholar]
- 31.Ruigómez A, Wallander MA, Johansson S, García Rodríguez LA. One-year follow-up of newly diagnosed irritable bowel syndrome patients. Aliment Pharmacol Ther. 1999;13(8):1097–102. doi: 10.1046/j.1365-2036.1999.00576.x. [DOI] [PubMed] [Google Scholar]
- 32.Ladep NG, Okeke EN, Samaila AA, Agaba EI, Ugoya SO, Puepet FH, et al. Irritable bowel syndrome among patients attending General Outpatients’ clinics in Jos, Nigeria. Eur J Gastroenterol Hepatol. 2007;19(9):795–9. doi: 10.1097/MEG.0b013e3282202ba5. [DOI] [PubMed] [Google Scholar]
- 33.Celebi S, Acik Y, Deveci SE, Bahcecioglu IH, Ayar A, Demir A, et al. Epidemiological features of irritable bowel syndrome in a Turkish urban society. J Gastroenterol Hepatol. 2004;19(7):738–43. doi: 10.1111/j.1440-1746.2004.03367.x. [DOI] [PubMed] [Google Scholar]
- 34.Wigington WC, Johnson WD, Minocha A. Epidemiology of irritable bowel syndrome among African Americans as compared with whites: a population-based study. Clin Gastroenterol Hepatol. 2005;3(7):647–53. doi: 10.1016/s1542-3565(05)00367-8. [DOI] [PubMed] [Google Scholar]
- 35.Nicholl BI, Halder SL, Macfarlane GJ, Thompson DG, O’Brien S, Musleh M, et al. Psychosocial risk markers for new onset irritable bowel syndrome--results of a large prospective population-based study. Pain. 2008;137(1):147–55. doi: 10.1016/j.pain.2007.08.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Secondulfo M, Mennella R, Fonderico C. Role of psychological factors in patients with irritable bowel syndrome. Intenista. 2002;10:169–73. [Google Scholar]
- 37.Si JM, Wang LJ, Chen SJ, Sun LM, Dai N. Irritable bowel syndrome consulters in Zhejiang province: the symptoms pattern, predominant bowel habit subgroups and quality of life. World J Gastroenterol. 2004;10(7):1059–64. doi: 10.3748/wjg.v10.i7.1059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Tan YM, Goh KL, Muhidayah R, Ooi CL, Salem O. Prevalence of irritable bowel syndrome in young adult Malaysians: a survey among medical students. J Gastroenterol Hepatol. 2003;18(12):1412–6. doi: 10.1046/j.1440-1746.2003.03212.x. [DOI] [PubMed] [Google Scholar]
- 39.Ringström G, Abrahamsson H, Strid H, Simrén M. Why do subjects with irritable bowel syndrome seek health care for their symptoms? Scan J Gastroenterol. 2007;42(10):1194–203. doi: 10.1080/00365520701320455. [DOI] [PubMed] [Google Scholar]


