Abstract
BACKGROUND:
To investigate the association between Metabolic syndrome (MetS) and Health related quality of life (QoL) in Iranian population.
METHODS:
We used data from the post-intervention phase of Isfahan Healthy Heart Program (IHHP), a community trial for cardiovascular disease (CVD) prevention and control. We recruited 9570 healthy adults, aged ≥ 19 years who were randomly selected using multistage random sampling method. World Health Organization QoL questionnaire (WHOQOL-BREF) which contains 26 items was used to assess QoL. It assesses four domains of QoL; Physical health, Psychological health, Social relationship and Environmental issues. MetS was defined based on ATP III criteria.
RESULTS:
The mean age of participants was 38.8±15.6 years (mean ± SD) and the prevalence of MetS was 22.5%. From all participant 18.2% were illiterate and 13.2% had university educational level. Two way multivariate analyses of covariance (MANCOVA) test after adjusting age showed significant difference between women with and without Mets in regard to physical health and social relations domains, while none of QoL domains was different in men with Mets in comparison to men without it.
CONCLUSIONS:
After adjusting the role of socio-demographic factors as components of QoL score, no association was observed between QoL domains and MetS in men, while only social relations and physical health scores were higher in women with Mets compared to those without Mets. Other variety of health-related QoL assessment tools or definitions of MetS may show different relationship in the Iranian socio-cultural context.
Keywords: Metabolic syndrome, Quality of life, General population
Metabolic syndrome (MetS) increases the risk of cardiovascular diseases (CVD) and diabetes.1,2 Yet, it's pathogenesis is not completely understood.3 MetS is a chronic and progressive condition that influence physical, mental and sexual functions.4–6 The prevalence of MetS in Iran is increasing during recent years from 10 to 63.2% approximately. This diversity is due to variety in MetS definitions and different target populations in these studies.7–10 Our previous study that was conducted on 12600 adults in three counties in central Iran, reported a prevalence of 21.9%.9 The same study showed an increasing prevalence of MetS in the middleaged women in urban areas.9,11
Although MetS is being studied quite extensively, reports on the association between health-related quality of life (QoL) and MetS at the population level are scarce. Today, subjective well-being has become a part of health outcome evaluation in studies and clinical practice. QoL is one of the important health outcome concepts that are expressed subjectively by patients. It considers all health dimensions; physically, mentally and socioeconomically.12,13
It is considerable that MetS influences QoL, however evidences regarding this relationship are not common. Some studies in different countries determined the association of QoL with components of MetS. For example, hypertension had strong association with impaired QoL.14–19 Additionally, obesity was associated with impaired QoL in both genders.20–23 Others demonstrated that Insulin resistance had direct effect on the decreased scores of QoL.24
Many studies regarding MetS have been conducted in Iran, but none considered Mets and QoL, therefore, we decided to compare various domains of health-related QoL between subjects with Mets and without it.
Methods
Isfahan Healthy Heart Program (IHHP) was conducted in three counties; Isfahan and Najaf-Abad as intervention areas and Arak as reference area, all located in central Iran. IHHP was started in 2000, it consisted of three phases that include baseline surveys for situational analysis, intervention activities that implemented in the intervention areas (late in 2001-2005), and post-intervention survey (2007) to evaluate the program outcomes.25,26 Having resided for at least five years in these areas, not being pregnant and being mentally healthy were the inclusion criteria in this study.
After the baseline survey, a five-year intervention program was started both in urban and rural areas of Isfahan and Najaf-Abad and was continued until 2005. Arak was evaluated as a reference area without interventions. Ten intervention projects based on different target groups were designed and implemented to address the general population and specific target groups in an integrated package.26 Intervention strategies consisted of healthy nutrition, tobacco control, physical activity and coping strategies.27 We used the data of the postintervention phase that was conducted in 2007.
Written informed consents were obtained from 9570 participants, aged ≥19 years after full explanation of the whole study. Questionnaires were completed for each participant that includes demographic data, past medical history and medication use. Marital state, education level, occupation and income were considered as Socio-economical factors. Education categorized based on training system in Iran as, primary, guidance and high school and university training. Income was categorized based on poverty boundary in Iran that was 3000000 Rials. Monthly income less than 300000 was considered very low, 3000000 to 4500000 as low, 4500000 to 6000000 as middle, 6000000 to 8000000 as high and more than this level as very high income. Each American dollar approximately equals to 10000 Iranian Rials.
We used updated ATP III definition for MetS. In this definition participants should meet three of the following criteria: waist circumference ≥ 102 cm (40 inch) in men and 88 cm (35 inch) in women; HDL < 1.03 mmol/L (40 mg/dl) in men and, 1.30 mmol/L (50 mg/dl) in women or specific treatment for this lipid abnormality; triglycerides ≥ 1.7 mmol/L (150 mg/dl) or specific treatment for this lipid abnormality; systolic blood pressure ≥ 130 mmHg or diastolic blood pressure ≥ 85 mmHg or treatment of previously diagnosed hypertension; and fasting blood glucose ≥ 5.6 mmol/L (100 mg/dl).28
We used the World Health Organization (WHO) brief version of quality of life questionnaire (WHOQoL-BREF). The WHOQoL-BREF contains a total of 26 questions, based on four domains of physical health, psychological health, social relationship and environmental issues. Physical health contains activities of daily life, dependence on medicinal substances and medical aids, energy and fatigue, mobility, pain and discomfort, sleep and rest and work capacity. Psychological health contains body image and appearance, negative feelings, positive feelings, self-esteem, spirituality or religion and personal beliefs, thinking, learning, memory and concentration. Social relationship contains personal relationships, social support, and sexual activity. Environmental issues contain financial resources, freedom, physical safety and security, health and social care accessibility and quality, home environment, physical environment (pollution, noise, traffic, and climate) and transport.30 We translated and validated the questionnaire for Iranian population. Additionally, it was standardized for Iranian population by Nejat and co-workers.30
Statistical analysis
Statistical procedure was done by Statistical Program for Social Sciences software (SPSS) - version 15. Categorical data were analyzed by Chi-square test and mean comparisons were done by t-test. To adjust the effect of age in the analysis we used two ways MANCOVA test after sex stratification. In this analysis, all four domains of QoL were entered to the model as dependent variables. Multivariate Wilks’ Lambda test was used to compare the mean values of all QoL domains in both groups (with or without Mets). All differences were considered as statistically significant at p < 0.05.
Results
Totally, 9570 participants were studied. Male to female ratio was 1. The Mean age of all participants was 38.8 ± 15.6 years (Mean±SD). However, the mean age was significantly higher in MetS than non-MetS group (48.99 ± 15.54 vs. 35.83 ± 14.28 years respectively).
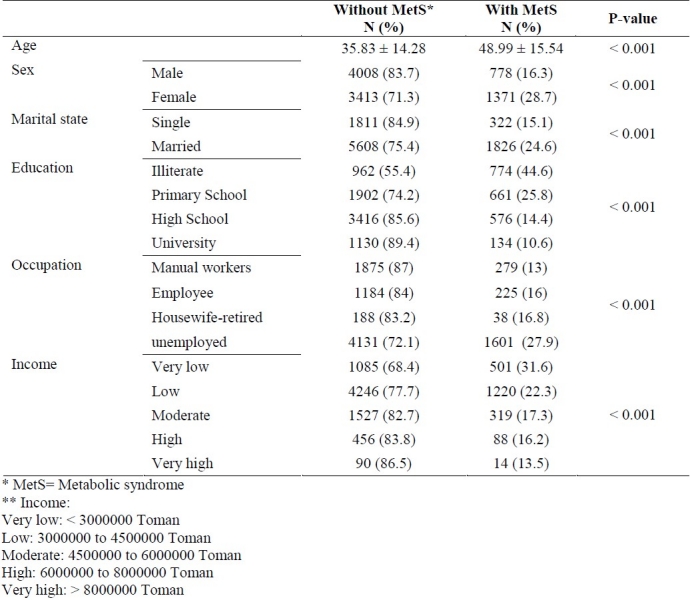
The prevalence of MetS was 22.5%. From all participant 18.2% were illiterate and 13.2% had university educational level (p < 0.001). There were many statistical differences related to socio-demographic characteristics between subjects with or without MetS (Table 1). As shown, MetS was more frequent in female gender, lower educational and income levels and in married persons (p < 0.001).
Table 1.
Socio-demographic characteristics of participants with or without metabolic syndrome
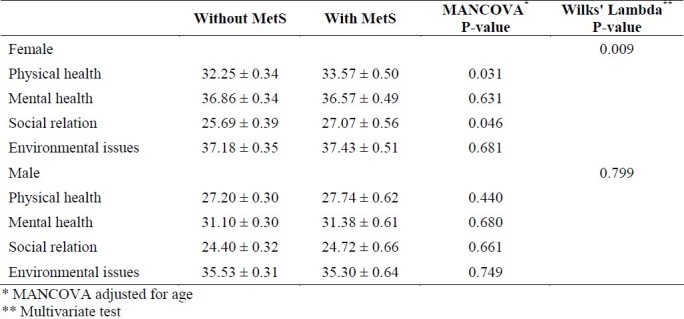
Univariate analysis demonstrated statistical significant differences between participants with and without MetS regarding WHO QoL-BREF domains. Figure 1 shows mean and 95%CI of QoL domains in Univariate analysis based on the presence of Mets without adjusting for age. As shown in figure 1, important point was the higher scores of QoL domains in participants with MetS than those without it. However, after adjusting for age in both genders using MANCOVA test, there was no significant differences between two groups except for social relations and physical health domains in women (p = 0.046, p = 0.031 respectively) (Table 2).
Figure 1.
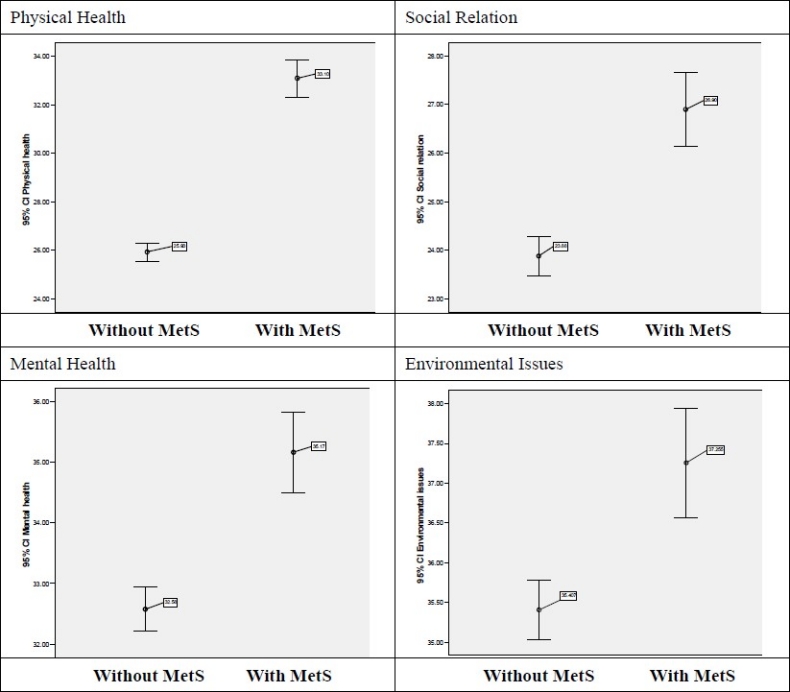
Mean and 95%CI of quality of life domains in Univariate analysis based on the presence of metabolic syndrome (Unadjusted by age)
Table 2.
Age-adjusted mean score of quality of life domains in subjects with or without metabolic syndrome based on sex (Mean± Std. Error)
Discussion
Our results did not find any significant association between QoL various domains and Mets syndrome except social relations and physical health that was significantly higher in women with MetS than those without MetS (Table 2). These findings are inconsistent with other studies. It is notable that our questions responses and the QoL questionnaire were validated.
Many studies have reported impaired QoL in subjects with MetS. Studies from USA, Brazil, Finland, Sweden, Korea and Italy showed an association between QoL impairment and MetS.31–35,4 Although other studies showed that QoL in woman is strongly impacted by Mets, it is difficult to discern it as a risk of or sequel to impaired QoL.36 The first reason to explain the difference between our and other studies is the variety of QoL assessment tools. We used the WHOQoL-BREF questionnaire which is one of the most standardized questionnaires of QoL worldwide. Others used EuroQoL, Center for disease control Health Related QoL-4, Gothenburg QoL instrument, Short form 36-item (SF-36) and other specific instruments.31,34,35 There are two kinds of questionnaires that can assess health-related QoL, the generic questionnaire which evaluate QoL in general conditions at the population level; and specific questionnaire that have been designed to assess QoL in specific conditions or groups; like cardiovascular disease, asthma, elderly etc.12,38 Most studies that have investigated the association of MetS and QoL used the general questionnaires.
Another subject that may explain the difference between our findings and others is the criteria for MetS definition. Several criteria exist to define MetS. We used ATP-III criteria. A previous study in Iran reported a higher prevalence of MetS based on ATP-III criteria than on IDF and modified WHO ones.10
Different study designs may also explain the different results reported by various studies. Our study was a community-based trial done in three counties in the central part of Iran which had sufficient sample size. Perhaps, variety in methodology and sample size causes differences between studies. However, it is considerable that the best design is a longitudinal one which is expensive and time-bounded.
Different socio-economical status and cultural concerns may be another reason for the differences in results. QoL is a subjective well-being measure that is extensively influenced by cultural context. Although using standard instruments harmonizes the variety, but it depends on subjective concepts.12 On the other hand, in the past decades Iranian population has experienced relatively rapid socioeconomic status (SES) improvement, resulting in many lifestyle modifications that have promoted increased prevalence of obesity and associated diseases, such as Mets.
As concluded in previous studies, socio-demographic variables are very strong predictors of MetS.38,39 In our study, we found significant association between MetS and age, sex, education and occupation. However, in our multivariate analysis after adjusting the role of socio-demographic factors, significant association was observed only between social relations and health domains of QoL and MetS.
Limitation
One of the limitations in the current study was its cross-sectional design that MetS and QoL were measured at the same time. Although longitudinal studies are preferred to evaluate causal relationships, however a cross-sectional one could be enough to achieve association between QoL and Mets which was our main objective. Second, we used the generic QoL instrument. MetS specific QoL instrument has not been developed yet and other studies have used this questionnaire for the same purpose. Another limitation was the cultural context in Iran. Although the QoL questionnaire has been validated before, but we believe that for some people it was difficult to answer some items like questions about their income.
Conclusions
We conclude that there is no association between MetS and QoL in Iranian subjects except in the concept of social and physical health domains in women. We recommend further studies with other QoL measurement tools and perhaps a Mets specific one and also other Mets definitions. Furthermore, another study design may be more effective to assess the aforementioned relationships.
Authors’ Contributions
AAT has designed the study and drafted this manuscript. MGH has carried out the study and drafted the manuscript. NS designing the study, revised the manuscript procedures, and drafted the manuscript. MAR has analysed the data and drafted the tables. KR helped in designing the study. BZ helped in statistical analysis. MB helped in designing the study. SZ revised the manuscript. AKH helped in designing the study. AY helped in designing the study. All authors read and approved the final manuscript.
Acknowledgments
This program was supported by a grant (No. 31309304) from the Iranian Budget and Planning Organization, as well as the Deputy for Health of the Iranian Ministry of Health and Medical Education and Iranian Heart Foundation. It was conducted by Isfahan Cardiovascular Institute with the collaboration of Isfahan Provincial Health Center, both affiliated to Isfahan University of Medical Sciences.
Footnotes
Conflict of Interests Authors have no conflict of interests.
References
- 1.Isomaa B, Almgren P, Tuomi T, Forsén B, Lahti K, Nissén M, et al. Cardiovascular morbidity and mortality associated with the metabolic syndrome. Diabetes Care. 2001;24(4):683–9. doi: 10.2337/diacare.24.4.683. [DOI] [PubMed] [Google Scholar]
- 2.Lakka HM, Laaksonen DE, Lakka TA, Niskanen LK, Kumpusalo E, Tuomilehto J, Salonen JT. The metabolic syndrome and total and cardiovascular disease mortality in middle-aged men. JAMA. 2002;288(21):2709–16. doi: 10.1001/jama.288.21.2709. [DOI] [PubMed] [Google Scholar]
- 3.Fulop T, Tessier D, Carpentier A. The metabolic syndrome. Pathol Biol. 2006;54(7):375–86. doi: 10.1016/j.patbio.2006.07.002. [DOI] [PubMed] [Google Scholar]
- 4.Corica F, Corsonello A, Apolone G, Mannucci E, Lucchetti M, Bonfiglio C, et al. Metabolic syndrome, psychological status and quality of life in obesity: the QUOVADIS Study. Int J Obes. 2008;32(1):185–91. doi: 10.1038/sj.ijo.0803687. [DOI] [PubMed] [Google Scholar]
- 5.Gardner AW, Momtgomery PS, Parker DE. Metabolic syndrome impairs physical function, health-related quality of life, and peripheral circulation in patients with intermittent claudication. J Vasc Surg. 2006;43(6):1191–6. doi: 10.1016/j.jvs.2006.02.042. discussion 1197. [DOI] [PubMed] [Google Scholar]
- 6.Esposito K, Giugliano D. Obesity, the metabolic syndrome, and sexual dysfunction. Int J Impot Res. 2005;17(5):391–8. doi: 10.1038/sj.ijir.3901333. [DOI] [PubMed] [Google Scholar]
- 7.Kelishadi R, Gharipour M, Sadri GH, Tavasoli AA, Amani A. Cardiovascular disease risk factors, metabolic syndrome and obesity in an Iranian population. East Mediterr Health J. 2008;14(5):1070–9. [PubMed] [Google Scholar]
- 8.Nabipour I, Amiri M, Imami SR, Jahfari SM, Shafeiae E, Nosrati A, et al. The metabolic syndrome and nonfatal ischemic heart disease; a population-based study. Int J Cardiol. 2007;118(1):48–53. doi: 10.1016/j.ijcard.2006.06.017. [DOI] [PubMed] [Google Scholar]
- 9.Sarrafzadegan N, Kelishadi R, Baghaei A, Hussein Sadri G, Malekafzali H, Mohammadifard N, et al. Metabolic syndrome: an emerging public health problem in Iranian women: Isfahan Healthy Heart Program. Int J Cardiol. 2008;131(1):90–6. doi: 10.1016/j.ijcard.2007.10.049. [DOI] [PubMed] [Google Scholar]
- 10.Zabetian A, Hadaegh F, Azizi F. Prevalence of metabolic syndrome in Iranian adult population, concordance between the IDF with the ATPIII and the WHO definitions. Diabetes Res Clin Pract. 2007;77(2):251–7. doi: 10.1016/j.diabres.2006.12.001. [DOI] [PubMed] [Google Scholar]
- 11.Gharipour M, Kelishadi R, Baghaie M, Rabiei K. Metabolic syndrome in an Iranian adult population. Eur Heart J. 2006;27(Suppl1):250–1. [Google Scholar]
- 12.Peterman AH, Rothrock N, Cella D. Evaluation of health-related quality of life. [cited 2010 March 8]. Available from URL: http://www.uptodate.com/contents/evaluation-of-health-related-quality-of-life .
- 13.Fallowfield L. Quality of life assessment in patients with heart disease. Br Heart J. 1993;69(5):371–2. doi: 10.1136/hrt.69.5.371-a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Os I. Quality of life in hypertension. J Hum Hypertens. 1994;8(Suppl 1):S27–30. [PubMed] [Google Scholar]
- 15.Hayes DK, Denny CH, Keenan NL, Croft JB, Greenlund KJ. Health-related quality of life and hypertension status, awareness, treatment, and control: National Health and Nutrition Examination Survey, 2001-2004. J Hypertens. 2008;26(4):641–7. doi: 10.1097/HJH.0b013e3282f3eb50. [DOI] [PubMed] [Google Scholar]
- 16.Ayalon L, Gross R, Tabenkin H, Porath A, Heymann A, Porter B. Correlates of quality of life in primary care patients with hypertension. Int J Psychiatry Med. 2006;36(4):483–97. doi: 10.2190/2W72-7758-2227-8H45. [DOI] [PubMed] [Google Scholar]
- 17.Li W, Liu L, Puente JG, Li Y, Jiang X, Jin S, et al. Hypertension and health-related quality of life: an epidemiological study in patients attending hospital clinics in China. J Hypertens. 2005;23(9):1667–76. doi: 10.1097/01.hjh.0000174971.64589.39. [DOI] [PubMed] [Google Scholar]
- 18.Stein JD, Brown GC, Brown MM, Sharma S, Hollands H, Stein HD. The quality of life of patients with hypertension. J Clin Hypertens (Greenwich) 2002;4(3):181–8. doi: 10.1111/j.1524-6175.2002.00970.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bardage C, Isacson DG. Hypertension and health-related quality of life.An epidemiological study in Sweden. J Clin Epidemiol. 2001;54(2):172–81. doi: 10.1016/s0895-4356(00)00293-6. [DOI] [PubMed] [Google Scholar]
- 20.Larsson U, Karlsson J, Sullivan M. Impact of overweight and obesity on health-related quality of life-a Swedish population study. Int J Obes Relat Metab Disord. 2002;26(3):417–24. doi: 10.1038/sj.ijo.0801919. [DOI] [PubMed] [Google Scholar]
- 21.Jia H, Lubetkin EI. The impact of obesity on healthrelated quality-of-life in the general adult US population. J Pub Health. 2005;27(2):156–64. doi: 10.1093/pubmed/fdi025. [DOI] [PubMed] [Google Scholar]
- 22.Huang IC, Frangakis C, Wu AW. The relationship of excess body weight and health-related quality of life: Evidence from a population study in Taiwan. Int J Obes (Lond) 2006;30(8):1250–9. doi: 10.1038/sj.ijo.0803250. [DOI] [PubMed] [Google Scholar]
- 23.Ford ES, Moriarty DG, Zack MM, Mokdad AH, Chapman DP. Self-reported body mass index and health-related quality of life: Findings from the behavioural risk factor surveillance system. Obes Res. 2001;9(21):31. doi: 10.1038/oby.2001.4. [DOI] [PubMed] [Google Scholar]
- 24.Schlotz W, Ambery P, Syddall HE, Crozier SR, Sayer AA, Cooper C, et al. Specific associations of insulin resistance with impaired health-related quality of life in the Hertfordshire Cohort Study. Qual Life Res. 2007;16(3):429–36. doi: 10.1007/s11136-006-9129-5. [DOI] [PubMed] [Google Scholar]
- 25.Sarraf-Zadegan N, Sadri G, Malek Afzali H, Baghaei M, Mohammadi Fard N, Shahrokhi S, et al. Isfahan Healthy Heart Programme: a comprehensive integrated community-based programme for cardiovascular disease prevention and control.Design, methods and initial experience. Acta Cardiol. 2003;58(4):309–20. doi: 10.2143/AC.58.4.2005288. [DOI] [PubMed] [Google Scholar]
- 26.Sarraf-Zadegan N, Baghaei M, Sadri G, Kelishadi R, Malek AH, Boshtam M, et al. Isfahan healthy heart program: Evaluation of comperhensive, community-based interventions for non-communicable disease prevention. Prev Contr. 2006;2(2):73–84. [Google Scholar]
- 27.Sarrafzadegan N, Kelishadi R, Esmaillzadeh A, Mohammadifard N, Rabiei K, Roohafza H, et al. Do lifestyle interventions work in developing countries? Findings from the Isfahan Healthy Heart Program in the Islamic Republic of Iran. Bull World Health Organ. 2009;87(1):39–50. doi: 10.2471/BLT.07.049841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.British Hypertension Society. Technique of blood pressure measurement- a poster to illustrate recommended techniques. J Hypertens. 1985;3:293. [Google Scholar]
- 29.Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. Executive Summary of The Third Report of The National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, And Treatment of High Blood Cholesterol In Adults (Adult Treatment Panel III) JAMA. 2001;285(19):2486–97. doi: 10.1001/jama.285.19.2486. [DOI] [PubMed] [Google Scholar]
- 30.Geneva: WHO; 1996. WHOQOL group. WHO quality of life questionnaire (WHOQOL-BREF): Introduction, Administration, Scoring, and Generic version of assessment. [Google Scholar]
- 31.Nedjat S, Montazeri A, Holakoie K, Madjdzadeh SR. Standardization of Iranian version of WHO quaity of life questionnaire (WHO-BREF) Iran J Health School. 2006;4(4):1–12. [Google Scholar]
- 32.Ford ES, Li C. Metabolic syndrome and health-related quality of life among US adults. Ann Epidemiol. 2008;18(3):165–71. doi: 10.1016/j.annepidem.2007.10.009. [DOI] [PubMed] [Google Scholar]
- 33.Roriz-Cruz M, Rosset I, Wada T, Sakagami T, Ishine M, Roriz-Filho JS, et al. Stroke-independent association between metabolic syndrome and functional dependence, depression, and low quality of life in elderly community-dwelling Brazilian people. J Am Geriatr Soc. 2007;55(3):374–82. doi: 10.1111/j.1532-5415.2007.01068.x. [DOI] [PubMed] [Google Scholar]
- 34.Miettola J, Niskanen LK, Viinamaki H, Sintonen H, Kumpusalo E. Metabolic syndrome is associated with impaired health-related quality of life: Lapinlahti 2005 study. Qual Life Res. 2008;17(8):1 055–62. doi: 10.1007/s11136-008-9386-6. [DOI] [PubMed] [Google Scholar]
- 35.Frisman GH, Kristenson M. Psychosocial status and health related quality of life in relation to the metabolic syndrome in a Swedish middle-aged population. Eur J Cardiovasc Nurs. 2009;8(3):207–15. doi: 10.1016/j.ejcnurse.2009.01.004. [DOI] [PubMed] [Google Scholar]
- 36.Han JH, Park HS, Shin CI, Chang HM, Yun KE, Cho SH, et al. Metabolic syndrome and quality of life (QOL) using generalised and obesity-specific QOL scales. Int J Clin Pract. 2009;63(5):735–41. doi: 10.1111/j.1742-1241.2009.02021.x. [DOI] [PubMed] [Google Scholar]
- 37.Qader SS, Shakir YA, Samsioe G. Could quality of life impact the prevalence of metabolic syndrome? Results from a population-based study of Swedish women: the Women's Health in the Lund Area Study. Metab Syndr Relat Disord. 2008;6(3):203–7. doi: 10.1089/met.2008.0014. [DOI] [PubMed] [Google Scholar]
- 38.Patrick DL, Deyo RA. Generic and disease-specific measures in assessing health status and quality of life. Med Care. 1989;27(S217):S221. doi: 10.1097/00005650-198903001-00018. [DOI] [PubMed] [Google Scholar]
- 39.Stewart-Knox B. Psychological underpinnings of metabolic syndrome. Proc Nutr Soc. 2005;64(3):363–9. doi: 10.1079/pns2005444. [DOI] [PubMed] [Google Scholar]
- 40.Langenberg C, Kuh D, Wadsworth M, Brunner E, Hardy R. Social circumstances and education: life course origins of social inequalities in metabolic risk prospective national birth cohort. Am J Public Health. 2006;12(96):2216–21. doi: 10.2105/AJPH.2004.049429. [DOI] [PMC free article] [PubMed] [Google Scholar]


