Abstract
BACKGROUND:
Phytoestrogens are a group of plants derived compounds with weekly estrogen effect that appear to have protective effects on metabolic and hormonal abnormalities of women with polycystic ovary syndrome (PCOS). So the aim of this study was to investigate the effect of soy phytoestrogens on reproductive hormones and lipid profiles in PCOS women.
METHODS:
In this quasi-randomized trial, 146 subjects with PCOS were divided into two groups; the experimental group who received Genistein (Bergamon, Italy) 18 mg twice a day orally and the control group that received similar capsules with cellulose for 3 months. Hormonal features and lipid profiles were measured before and after 3 months of supplement therapy.
RESULTS:
After 3 months of supplement therapy there were no statistically significant differences in high density lipoprotein cholesterol (HDL) and follicle stimulating hormone (FSH) serum levels in Genistein and placebo group before and after treatment; however serum levels of luteinizing hormone (LH), triglyceride (TG), low density lipoprotein cholesterol (LDL), dehydroepiandrostrone sulfate (DHEAS) and testosterone were significantly decreased after 3 months therapy in Genistein group.
CONCLUSIONS:
Genistein consumption may prevent cardiovascular and metabolic disorders in PCOS patients by improving their reproductive hormonal and lipid profiles.
Keywords: Polycystic Ovary Syndrome, Genistein, Phytoestrogens, Cardiovascular Diseases
Polycystic ovary syndrome (PCOS) is the most common endocrinopathy represent in 15.2% of Iranian women in reproductive period based on Rotterdam criteria.1 The etiology of PCOS remains unclear, however several studies have suggested that PCOS is an x-linked dominant condition.2 Risk of ischemic heart disease, insulin resistance, hyperlipidemia, obesity, hypertension and metabolic syndrome are higher in these women.3–5 The most commonly used definition of PCOS includes at least two of three Rotterdam consensus clinical biochemical criteria and/or signs of hyperandrogenism, oligo and/or anovulation and sonographic finding of PCOS.6–9 Phytoestro gens are structurally similar to endogenous estrogen and have affinity to estrogen receptors. There are various types of phytoestrogens such as isoflavones, prenylated flavonoids, and coumestans. Genistein and daidzein are the most common form of them.
Insulin resistance can be encountered in women with PCOS that plays a role in lipoprotein disturbances and body morphology alteration and may predispose to early development of cardiovascular disease, diabetes and hyperlipidemia.10 Many studies showed that the consumption of Genistein have favorable effects on glucose, lipid metabolisms improving and may provide beneficial effects on cardiovascular system, obesity, diabetes and hyper-lipidemia which are risk factors for cardiovascular diseases.11–13 So the aim of this study was to investigate the effect of soy phytoestrogens on reproductive hormones and lipid profiles in PCOS women.
Methods
In this prospective quasi-randomized, doubleblinded, placebo-controlled study, a total of 146 reproductive women aged between 18-35 years old who were referred to outpatient clinics of Shahid Beheshty and Al-Zahra Hospitals from December 2009 to February 2010 for infertility treatments, having at least two of three Rotterdam consensus criteria as oligomenorrhea or amenorrhoeic cycle, hyperandrogen-ism, or 10 or more follicles with size range of 2-10 mm on trans vaginal sonography (AlOKA1000,7.5MH.Z probe), were enrolled.
Women should not have taken any hormonal or medication drugs, effective on metabolic systems for 3 months before starting the study and patients with diseases such as liver diseases, hyper or hypothyroidism, hyperprolactinemia, adrenal hyperplasia, kidney disease, cardiovascular diseases, hormonal sex-secreting neoplasm, diabetes, nervous system disorder and mentally disorders were excluded.
After approval of ethical committee of Isfahan University of Medical Sciences with registry number 388547 and support of vice chancellor of research at this university for the funding, all patients gave their written informed consents. Before any intervention, on the third day of follicular phase of spontaneous or induced menstrual cycle with medroxy progesterone acetate, blood samples as baseline hormonal assessment of dehydroepiandrostrone sulfate (DHEAS), follicle stimulating hormone (FSH), luteinizing hormone (LH), triglyceride (TG), total cholesterol, high density lipoprotein cholesterol (HDL), and low density lipoprotein cholesterol (LDL) were collected and recorded (TG, Total cholesterol Pars Azmoon, Tehran, Iran. FSH, LH, DHEAS with ELISA, Monoband kit).
Then patients were randomly divided into two groups with simple randomization.
The experimental group who received Genistein (Bergamon, Italy) 18 mg twice a day orally and the control group taking similar capsules with cellulose as a placebo for 3 months.
Patients were followed closely for 3 months and were instructed to attend our outpatient clinics if they had any problems. 4 subjects in the experimental group did not continue the study because of gastrointestinal side effects of Genistein, and 5 patients from the placebo group were excluded later because of incomplete data. The remaining 137 subjects completed the study (Figure1).
Figure 1.
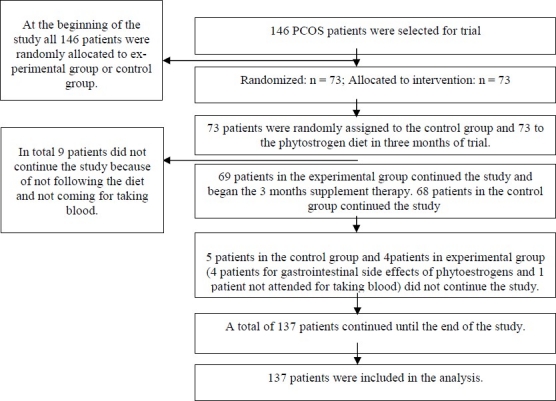
Patients participation diagram
After 3 months of supplementation therapy blood was taken from all subjects on the third day of their follicular phase of menstrual cycle for assessment of reproductive hormones and lipid profiles.
Data analysis was performed using the SPSS version 15.0 (SPSS, Inc., Chicago USA). All data between two groups were compared and analyzed using ANOVA test (Zα = 1.96, Zβ = 0.84) and p value less than 0.05 was considered statically significant.
Results
From 146 patients who enrolled in the study, 4 patients in the experimental group and 5 patients from the placebo group were excluded. So study continued with 69 subjects in the case and 68 in the placebo group (Figure 1). No significant difference was seen between two groups regarding age, weight, and BMI. The mean ± SD age of patients in Genistein group was 27.11 ± 5.76 and in the control group was 27.45 ± 5.77; the difference was not statistically significant.
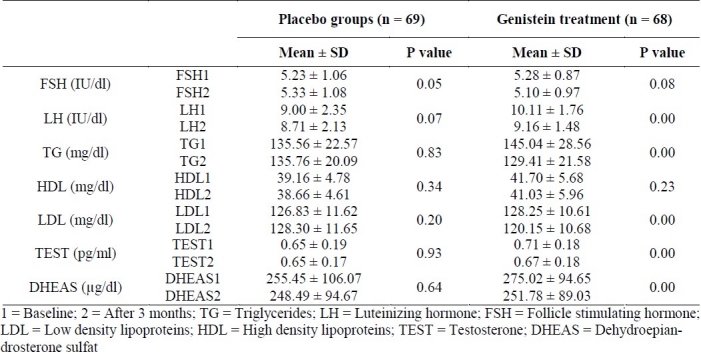
Phytoestrogen supplementation significantly reduced LH (p = 0.000), TG (p = 0.000), LDL (p = 0.000), DHEAS (p = 0.000) and testosterone (p = 0.000) levels in patients after receiving Genistein comparing with before supplementation therapy but in the placebo group they were not different. Finally according to our results only LDL cholesterol was lower significantly after using Genistein compared with placebo (120.15 ± 10.68 vs. 126.61 ± 14.81 mg/dl respectively, p = 0.04). FSH and HDL levels were not significantly different (Table 1).
Table 1.
Comparison of clinical characteristic of the study subjects at baseline and after 3 months in genistein and placebo groups
Discussion
In the current study treatment with Genistein for 3 months resulted in a significant reduction in LDL cholesterol compared with placebo.
Metabolic syndrome and hormonal disturbances are prevalent findings among PCOS women.
Metabolic syndrome is a group of conditions including obesity, high blood pressure, blood fat abnormality and borderline high blood sugar and insulin levels, which together increase chances of cardio vascular disease and type 2 diabetes.14
In Tehran, Iran, it has been estimated that more than 30% of adults might be affected.15 Some studies have evaluated the effects of nutrients on glycemic control of type 2 diabetes and metabolic syndrome. Their results have shown beneficial effects of soy protein consumption.16,17
Two meta-analysis concluded that isofla-vones content of soy might be responsible for its lipid lowering effect.18,19 But some other studies did not confirm these results.20 Therefore, because of these controversies we decided to evaluate the effect of Genistein on hormonal and metabolic abnormalities in women with PCOS.
Lissin and Cooke suggested that diets containing soy-protein may provide favorable benefits in reducing LDL cholesterol and cardiovascular events.21 Azadbakht et al in a randomized cross over clinical trial which was done on 42 postmenopausal women with metabolic syndrome comparing soy protein with esoy nut and controlled diet, showed that neither soy protein nor soy nut could affect weight and serum leptin levels.22
Wiseman et al in a randomized cross over design compared the effect of a dietary regimen high in isoflavones with a similar product in which all of the soy was removed by alcohol. Their results showed that antioxidant effect of soy may protect against the oxidative lipid damage that is the leading cause of cardiovascular diseases and cancers.23 A study Azadbakht et al indicated that soy compounds like isoflavones, fibers, phospholipids, fatty acids and its other components could have beneficial effects on cardio metabolic abnormalities such as hypercholesterolemia and lipid abnormality.24 Results of our study revealed that administration of Genistein not only reduced LDL cholesterol but also significantly reduced LH, TG, DHEAS and testosterone parameters after 3 months.
Ohno et al also showed that Genistein has a significant role on steroidogenesis in the adrenal gland and testis of rat, and decreasing the testosterone level.25 Romualdi et al performed a pilot prospective study on patients with PCOS, which revealed that treating patients with phytoestrogens result in improvement of lipid assessment, and they suggested that using phytoestrogens may have a possible advantage in improvement of lipid assessment in women with PCOS.26 We also observed the same effect on improvement of lipid assessment. According to the research of Kurzer soy consumption appear to have modest hormonal effects on both pre- and postmenopausal women.27 Consuming 45-200 mg/dl isoflavones in different products like soy milk or soy flour or soy foods would decrease the midcycle FSH and LH. According to our results in Genistein group, LH, testosterone, and DHEAS decreased significantly after treatment but FSH was not significantly different.
Conclusions
In conclusion, results of our study suggest that supplementation therapy with Genistein that is rich of soy phytoestrogen has possible advantages in patients with PCOS and may be chosen as an alternative treatment for these women and may provide favorable advantages in reduction of related complications.
Limitations of the Study
We did not analyze mean of different variables between two groups at the baseline. It seems that LH, testosterone, and DHEAS at the baseline, might have been different between the placebo group and Genistein group. However significant differences that were observed between results of before and after treatment in Genistein group may overcome this limitation.
Measuring weight and body mass index in two groups was not designed in our proposal to see their impact on the results. Therefore we suggest a better randomized clinical trial considering all above limitations.
We may also suggest using different doses of Genistein on reproductive hormonal and lipid profiles.
Authors’ Contributions
BKH, FM and EKH carried out the design and developed the study. EKH was responsible for data analysis, data gathering and interpretation of results and performed clinical follow-ups. AE was responsible for manuscript preparation and scientific writing of the manuscript. All authors have read and approved the content of the manuscript.
Acknowledgments
We are appreciative to the staffs of Beheshti and Al-Zahra Hospitals for their help in clinical follow-ups.
Footnotes
Conflict of Interests Authors have no conflict of interests.
References
- 1.Mehrabian F, Khani B, Kelishadi R, Ghanbari E. The prevalence of polycystic ovary syndrome in Iranian women based on differentdiagnostic criteria 2011. Polish journal of endocrinology. 2011 [In Press] [PubMed] [Google Scholar]
- 2.Speroff L, Fritz MA. 7th ed. Philadelphia: Lippincott Williams and Wilkins; 2004. Clinical gynecologic endocrinology and infertility; pp. 470–83. [Google Scholar]
- 3.Erdman JW., Jr AHA Science Advisory: soy protein and cardiovascular disease, a statement for healthcare professionals from the Nutrition Committee of the AHA. Circulation. 2000;102(20):2555–9. doi: 10.1161/01.cir.102.20.2555. [DOI] [PubMed] [Google Scholar]
- 4.DeUgarte CM, Bartolucci AA, Azziz R. Prevalence of insulin resistance in the polycystic ovary syndrome using the homeostasis model assessment. Fertil Steril. 2005;83(5):1454–60. doi: 10.1016/j.fertnstert.2004.11.070. [DOI] [PubMed] [Google Scholar]
- 5.Legro RS, Kunselman AR, Dunaif A. Prevalence and predictors of dyslipidemia in women with polycystic ovary syndrome. Am J Med. 2001;111(8):607–13. doi: 10.1016/s0002-9343(01)00948-2. [DOI] [PubMed] [Google Scholar]
- 6.Rotterdam ESHRE/ASRM-Sponsored PCOS Consensus Workshop Group. Revised 2003 consensus on diagnostic criteria and long-term health risks related to polycystic ovary syndrome. Fertil Steril. 2004;81(1):19–25. doi: 10.1016/j.fertnstert.2003.10.004. [DOI] [PubMed] [Google Scholar]
- 7.Ehrmann DA. Polycystic ovary syndrome. N Engl J Med. 2005;352(12):1223–36. doi: 10.1056/NEJMra041536. [DOI] [PubMed] [Google Scholar]
- 8.Azziz R. Diagnostic criteria for polycystic ovary syndrome: a reappraisal. Fertil Steril. 2005;83(5):1343–6. doi: 10.1016/j.fertnstert.2005.01.085. [DOI] [PubMed] [Google Scholar]
- 9.McCartney CR, Prendergast KA, Chhabra S, Eagleson CA, Yoo R, Change RJ, et al. The association of obesity and hyperandrogenemia during the pubertal transition in girls: obesity as a potential factor in the genesis of postpubertal hyperandrogenism. J Clin Endocrinol Metab. 2006;91(5):1714–22. doi: 10.1210/jc.2005-1852. [DOI] [PubMed] [Google Scholar]
- 10.Botros R, Rizk MB. Cambridge: Cambridge University Press; 2001. Infertility and assisted reproduction; pp. 246–7. [Google Scholar]
- 11.Yildiz F. 1st ed. Oxford: CRC Press; 2005. Phytoestrogens in functional foods; pp. 210–1. [Google Scholar]
- 12.Bhathena SJ, Velasquez MT. Beneficial role of dietary phytoestrogens in obesity and diabetes. Am J Clin Nutr. 2002;76(6):1191–201. doi: 10.1093/ajcn/76.6.1191. [DOI] [PubMed] [Google Scholar]
- 13.Jayagopal V, Albertazzi P, Kilpatrick ES, Howarth EM, Jennings PE, Hepburn DA, et al. Beneficial effect of Soy phytoestrogen intake in postmenopausal women with type 2 diabetes. Diabetes Care. 2002;25(10):1709–14. doi: 10.2337/diacare.25.10.1709. [DOI] [PubMed] [Google Scholar]
- 14.Lau DC, Yan H, Dhillon B. Metabolic syndrome: a marker of patients at high cardiovascular risk. Can J Cardiol. 2006;22(Suppl B):85B–90B. doi: 10.1016/s0828-282x(06)70992-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Azizi F, Salehi P, Etemadi A, Zahedi-Asl S. Prevalence of the metabolic syndrome in an urban population: Tehran Lipid and Glucose Study. Diabetes Res Clin Pract. 2003;61(1):29–37. doi: 10.1016/s0168-8227(03)00066-4. [DOI] [PubMed] [Google Scholar]
- 16.Lukaczer D, Liska DJ, Lerman RH, Darland G, Schiltz B, Tripp M, et al. Effect of a low glycemic index diet with soy protein and phytosterols on CVD risk factors in postmenopausal women. Nutrition. 2006;22(2):104–13. doi: 10.1016/j.nut.2005.05.007. [DOI] [PubMed] [Google Scholar]
- 17.Szkudelska K, Nogowski L. Genistein--a dietary compound inducing hormonal and metabolic changes. J Steroid Biochem Mol Biol. 2007;105(1-5):37–45. doi: 10.1016/j.jsbmb.2007.01.005. [DOI] [PubMed] [Google Scholar]
- 18.Taku K, Umegaki K, Sato Y, Taki Y, Endoh K, Watanabe S. Soy isoflavones lower serum total and LDL cholesterol in humans: a meta-analysis of 11 randomized controlled trials. Am J Clin Nutr. 2007;85(4):1148–56. doi: 10.1093/ajcn/85.4.1148. [DOI] [PubMed] [Google Scholar]
- 19.Zhuo XG, Melby MK, Watanabe S. Soy isoflavone intake lowers serum LDL cholesterol: a meta-analysis of 8 randomized controlled trials in humans. J Nutr. 2004;134(9):2395–400. doi: 10.1093/jn/134.9.2395. [DOI] [PubMed] [Google Scholar]
- 20.Weggemans RM, Trautwein EA. Relation between soy-associated isoflavones and LDL and HDL cholesterol in humans: a meta-analysis. Eur J Clin Nutr. 2003;57(8):940–6. doi: 10.1038/sj.ejcn.1601628. [DOI] [PubMed] [Google Scholar]
- 21.Lissin LW, Cooke JP. Phytoestrogens and cardiovascular health. J Am Coll Cardiol. 2000;35(6):1403–10. doi: 10.1016/s0735-1097(00)00590-8. [DOI] [PubMed] [Google Scholar]
- 22.Azadbakht L, Esmaillzadeh A. A randomized cross-over trial on soy intake and serum leptin levels in postmenopausal women with metabolic syndrome. J Res Med Sci. 2010;15(6):317–23. [PMC free article] [PubMed] [Google Scholar]
- 23.Wiseman H, O’Reilly JD, Adlercreutz H, Mallet AI, Bowey EA, Rowland IR, et al. Isoflavone phytoestrogens consumed in soy decrease F(2)-isoprostane concentrations and increase resistance of low density lipoprotein to oxidation in humans. Am J Clin Nutr. 2000;72(2):395–400. doi: 10.1093/ajcn/72.2.395. [DOI] [PubMed] [Google Scholar]
- 24.Azadbakht L, Esmaillzadeh A. Soy and cardio-metabolic abnormalities: an update. 2008;13(2):88–96. [Google Scholar]
- 25.Ohno S, Nakajima Y, Inoue K, Nakazawa H, Nakajin S. Genistein administration decreases serum corticosterone and testosterone levels in rats. Life Sci. 2003;74(6):733–42. doi: 10.1016/j.lfs.2003.04.006. [DOI] [PubMed] [Google Scholar]
- 26.Romualdi D, Costantini B, Campagna G, Lanzone A, Guido M. Is there a role for soy isoflavones in the therapeutic approach to polycystic ovary syndrome? Results from a pilot study. Fertil Steril. 2008;90(5):1826–33. doi: 10.1016/j.fertnstert.2007.09.020. [DOI] [PubMed] [Google Scholar]
- 27.Kurzer MS. Hormonal effects of soy isoflavones: studies in premenopausal and postmenopausal women. J Nutr. 2000;130(3):660S–1S. doi: 10.1093/jn/130.3.660S. [DOI] [PubMed] [Google Scholar]


