Abstract
BACKGROUND:
Breast cancer has been considered as a major health problem in females, because of its high incidence in recent years. Due to the role of breast self-examination (BSE) in early diagnosis and prevention of morbidity and mortality rate of breast cancer, promoting student knowledge, capabilities and attitude are required in this regard. This study was conducted to evaluation BSE education in female University students using Health Belief Model.
METHODS:
In this semi-experimental study, 243 female students were selected using multi-stage randomized sampling in 2008. The data were collected by validated and reliable questionnaire (43 questions) before intervention and one week after intervention. The intervention program was consisted of one educational session lasting 120 minutes by lecturing and showing a film based on HBM constructs. The obtained data were analyzed by SPSS (version11.5) using statistical paired t-test and ANOVA at the significant level of α = 0.05.
RESULTS:
243 female students aged 20.6 ± 2.8 years old were studied. Implementing the educational program resulted in increased knowledge and HBM (perceived susceptibility, severity, benefit and barrier) scores in the students (p ≤ 0.01). Significant increases were also observed in knowledge and perceived benefit after the educational program (p ≤ 0.05). ANOVA statistical test showed significant difference in perceived benefit score in students of different universities (p = 0.05).
CONCLUSIONS:
Due to the positive effects of education on increasing knowledge and attitude of university students about BSE, the efficacy of the HBM in BSE education for female students was confirmed.
Keywords: Evaluation Studies, Breast Self-Examination, Education, Students
At present, after cardiovascular diseases, cancer is the second cause of death in the world1 and the third in Iran.2,3 Breast cancer is one of the concerns of societies especially for women and is the most prevalent female malignancy.4,5 Prevalence of this disease is varied in different parts of the world. According to the American Cancer Society report, breast cancer is diagnosed in about 1.3 million women annually worldwide and around 465,000 will die from the disease.6 It is estimated that 207,090 new cases of invasive breast cancer are expected to occur among women during 2010 in the US.7 Breast cancer was increasing over the years in Iran and is now ranked as the first among cancers diagnosed in women; comprising 24.4% of all malignancies with a crude incidence rate and agestandardised incidence rates (ASR) of 17.4 and 23.1 per 100,000 population, respectively.8 Results of recent studies in Iran indicated that the age of onset of breast cancer in Iran is about 10 years earlier than developed countries.8,9 Mousavi et al study showed that the most prevalence age of onset of breast cancer in Iranian women is between 40 to 49 years old.10 Breast cancer has an enormous impact on the health of women and remains a major public health concern across the world and in Iran.11
In spite of technical improvements in surgery, chemotherapy and radiotherapy, the mortality rate due to breast cancer is increasing.12 Because of high cost in treatment, health education and prevention of breast cancer is very important.13 The best way for early diagnosis is breast cancer screening, in which breast self-examination (BSE) and clinical examination by a trained doctor and mammography are recommended.14–16 Studies showed that survival rate of women who had early diagnosis was 90% and survival rate in women who had developed breast cancer has been reduced to 60%.17
Because the etiology of cancer has not been recognized yet, early diagnosis is very important to control and care of this disease.18 Therefore, regular BSE is a simple and effective method in early diagnosis of breast cancer.19 Yet, lots of women in Iran do not have enough knowledge and experience about BSE. Individuals’ attitude is a more important factor in preventive behaviors including cancer control behavior than just knowledge about BSE.19–21 One of the best models that have efficiency in studying preventive behaviors in cancer is Health Belief Model (HBM). HBM originally developed in the 1950s and updated in the 1980s. The HBM is a psychosocial model that accounts for health behaviors by identifying factors associated with individuals’ beliefs which influence their behaviors. The components of this model are perceived as severity, susceptibility, threatened, benefits and barriers.22,23 This model aimed personal decisions that are based on perceived susceptibility (believe that women are susceptible to develop breast cancer), perceived severity (believe that breast cancer is a serious disease), perceived benefits and perceived barriers to perform BSE. The HBM has been applied frequently for breast cancer screening.11,14,18,22 At present, educational needs for university students are increasing.24 Therefore, it is necessary to educate university students about health problems especially breast cancer.
There are few studies about BSE on university students in Iran, for example Hadizadeh et al study showed that 13.5% of students carried out regular BSE.25 Thus, not only should young students learn more about BSE, but they also have an important role in teaching their mothers to examine their breasts. Therefore, the aim of this study was to evaluate BSE education in female university students using HBM.
Methods
In this semi-experimental study of before and after type, female students of Birjand universities recruited by multi-stage randomized sampling. At first, new students of Birjand universities, including Medical Sciences University, Sciences University, Islamic Azad University and Technical School, were considered in four classes. Then, in each class, two clusters included students of academic fields were randomly selected. Based on sample size formula with α = 0.05, β = 0.1, δ = 3.88, and d = 2.5 on the basis of Mazloomy et al study,26 primary sample size equal to 126.4 was estimated. Following the adjustment coefficient 2 for clustered sampling, final sample size (253 students) was obtained. Those students, who were not willing to participate or discontinue the study, were excluded. For 253 students, primary questionnaire was completed before educational intervention. Of those who initially completed primary questionnaire, 10 dropped out due to their absence and did not complete secondary questionnaire. Therefore 243 questionnaires were finally analyzed.
For gathering data, we first designed a questionnaire on the base of planned objectives. Then, asked experienced colleagues (2 assistant professors in health education, 1 gynecologist, 2 instructors in midwifery and 2 instructors in society health nursing) for revising its content and construct validity. Reliability analysis was conducted for testing the reliability of knowledge and HBM components (perceived susceptibility, severity, benefits and barriers). Internal consistency of these sections of the questionnaire was calculated using Chronbach's alpha technique (0.84 for knowledge, 0.78 for susceptibility, 0.74 for severity, 0.69 for benefits and 0.78 for barriers).
The questionnaire included questions regarding the socio-demographic characteristics of students (such as age, Menarche at age, marital status), history of breast problems, history of BSE, and sources of breast cancer information. To assess knowledge, we used 11 items on knowledge about breast cancer and BSE with yes/no response options. Then, each correct response was scored one point and each wrong response was scored zero.
HBM questions consisted of perceived susceptibility (4 items), severity (5 items), benefits (4 items) and barriers (5 items) to breast cancer and BSE. We scored the items on a 3-point Likert scale ranging from agree to disagree; agree, not decided and disagree responses gained 3, 2, and 1 scores, respectively.
A pre-test was performed for determination of knowledge, perceived susceptibility, severity, benefits and barriers in university students about breast cancer and BSE. The researcher (MSc of health education) was the educator and instructed the students on how to perform BSE at home. The intervention program was consisted of one educational session lasting 120 minutes. During educational session, teaching methods such as lecturing using Power Point presentation, question and answer, BSE educational film and Pamphlets were used based on HBM constructs.
The education content involved the prevalence of breast cancer among women, its morbidity and mortality rate, definition, risk factors and signs of breast cancer, importance of breast cancer screening methods in early detection and how to perform BSE at home.
One week after performing education,24 post-test was done with the same questionnaire. The obtained data were analyzed by SPSS (version11.5, Chicago IL) using statistical paired t-test and one-way variance analysis at the significant level of α = 0.05.
Results
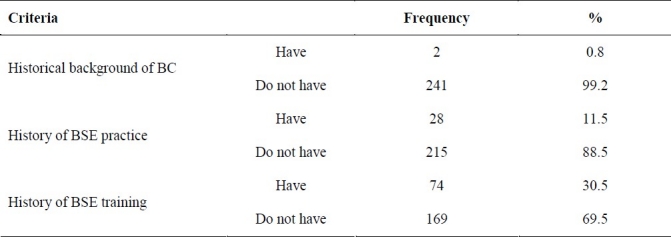
243 female students aged 20.6 ± 2.8 years old were studied, of which 87.2% were unmarried. A small number of subjects (28, 11.5%) had background of performing BSE. Among them 7% had done BSE once or twice and the others practiced it more than two times per year. Nearly one third (30.5%) had previously been trained about how to perform BSE (Table 1). The most important sources of information were doctors and other health professionals (48.6%). The educational program resulted in a significant increase (p ≤ 0.01) in knowledge, perceived susceptibility, severity, benefits and barriers in university students as described in table 2.
Table 1.
Frequent distribution of different criteria for historical backgrounds of breast cancer (BC) and breast self examination (BSE) in 243 female students of Birjand universities
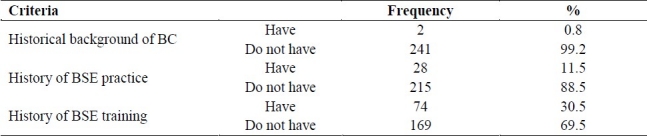
Table 2.
Frequent distribution of different criteria for historical backgrounds of breast cancer (BC) and breast self examination (BSE) in 243 female students of Birjand universities
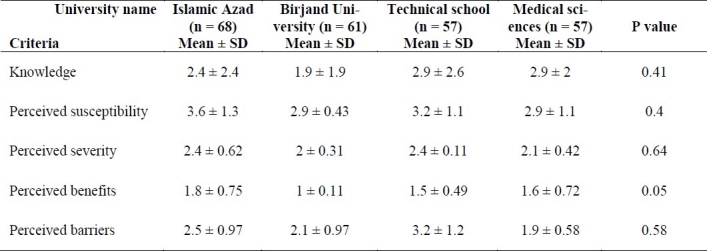
Independent student t-test on variations between pre- and post-tests in knowledge (p = 0.05) and perceived benefits (p = 0.01) based on subjects’ BSE backgrounds revealed significant changes as explained in table 3. ANOVA test on variations between pre- and post-tests in different universities showed significant difference only in perceived benefits. No statistical significant differences were found on other criteria (Table 4).
Table 3.
Comparing the mean of differences of before and after scores of knowledge, perceived susceptibility, severity, benefits and barriers in 243 female students of Birjand universities based on their BSE background
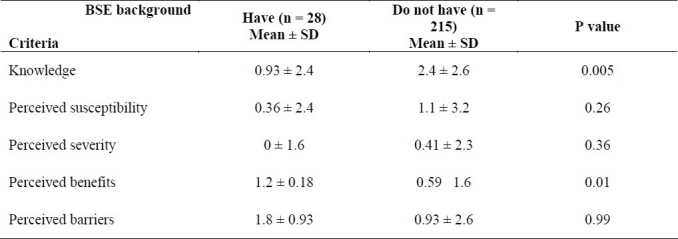
Table 4.
Comparing the mean of differences of before and after scores of knowledge, perceived susceptibility, severity, benefits and barriers in 243 female students of different universities
Discussion
BSE is one of the most important methods for early diagnosis of breast cancer. About 95% of all breast cancers can be diagnosed in primary stage by BSE.27
Based on our results, 11.5% of university students had history of performing BSE. In the study of Karimi et al 13.5% of 149 studied women in Ramsar had performed BSE at least once.28 According to Choudhry et al in Canada study 49% of studied individuals had at least performed BSE once during their lives29 and this rate was even higher (58%) in the USA.30 These differences might be related to time of education, as in Canada and the US early education regarding BSE in school ages was highly emphasized.
In this study 30.5% of the students had been trained for performing BSE in which the most important source of their information were doctors and other health professionals (48.6%). In Karimi et al study 69.1% of the studied women had gained information about BSE from different sources before training, mostly from radio and television.28 Public educations on screening and prevention methods in Iran especially on BSE have limitation due to the cultural and religious beliefs and so interventions in small groups, particularly university students are vital.
Education intervention on BSE in our university students increased their knowledge in this respect. The results of this study are similar to the reports of Aliyari et al who studied 98 women in army families,31 Ghanbari et al who studied 50 nursing and midwifery students in Rasht,24 Hadizadeh et al who studied 84 female students in Iran,25 Tahvildary et al who studied 600 staff of an educational office in Tehran,32 and Mazloomy et al who studied 140 female teachers in Yazd intermediate schools.26 However, they studied different females with different ages and places. Thus, this type of grouped health interventional education can be effective in different situations in Iran.
Sensiba and Stewart expressed in their research that the most important factor for not doing cancer screening tests is lack of knowledge. Thus, giving right information about cancer and screening methods to the high risk group may reduce their wrong believes.33 Patistea et al also showed that 34.7% of studied women had done BSE monthly. Those individuals who had done BSE also had more knowledge than the others.34 Kati□ et al also concluded that BSE educational program is effective and thus is necessary for all women.35 This should be implemented as much as possible at regular bases for all women older than 20 years old. In addition to the knowledge, believe and attitude about a disease are important factors in doing or not doing a preventive behavior particularly on BSE.36 Burnett et al suggested that factors causing changes in attitude must be strengthened.37
In this study, the HBM mean scores were increased in all components (perceived susceptibility, severity, benefits and barriers) after educational intervention which is in accordance with the results of Hadizadeh et al study.38
Fung's report on Chinese women expressed that the individual's attitude about BSE especially perceived susceptibility and barriers to breast cancer are important.39 Wardle also reported that the individual's attitude about the BSE benefits is related to performing BSE.40
Conclusions
On the bases of our research and the above mentioned reports, it is very important to survey the person's attitude and perceived susceptibility, severity, benefits and barriers of a preventive behavior. Thus, educational programs should be designed with the emphasis on positive aspects of BSE and with the aim of raising knowledge, attitude and practice level of individuals.
Authors’ Contributions
MM carried out the design and coordinated the study, participated in all of the stages and prepared the manuscript. GRSH and MBM and HSH provided assistance in the design of the study and participated in manuscript preparation. GRSHZ provided assistance in the design of the study and analysis of the data. All authors have read and approved the content of the manuscript.
Acknowledgments
Financial support of Birjand University of Medical Sciences (Grant No. 271) is acknowledged. The authors would like to thank all the students who participated in this study.
Footnotes
Conflict of Interests Authors have no conflict of interests.
References
- 1.Jemal A, Siegel R, Xu J, Ward E. Cancer statistics, 2010. CA Cancer J Clin. 2010;60(5):277–300. doi: 10.3322/caac.20073. [DOI] [PubMed] [Google Scholar]
- 2.Mousavi SM, Gouya MM, Ramazani R, Davanlou M, Hajsadeghi N, Seddighi Z. Cancer incidence and mortality in Iran. Ann Oncol. 2009;20(3):556–63. doi: 10.1093/annonc/mdn642. [DOI] [PubMed] [Google Scholar]
- 3.Emami Razavi SH, Aghajani H, Haghazali M, Nadali F, Ramazani R, Dabiri E, et al. The Most Common Cancers in Iranian Women. Iranian Journal of Public Health. 2009;38(Suppl 1):109–12. [Google Scholar]
- 4.Secginli S, Nahcivan NO. The effectiveness of a nurse-delivered breast health promotion program on breast cancer screening behaviours in non-adherent Turkish women: a randomized controlled trial. Int J Nurs Stud. 2011;48(1):24–36. doi: 10.1016/j.ijnurstu.2010.05.016. [DOI] [PubMed] [Google Scholar]
- 5.Pecorelli S, Favalli G, Zigliani L, Odicino F. Cancer in women. Int J Gynecol Obstet. 2003;82(3):369–79. doi: 10.1016/s0020-7292(03)00225-x. [DOI] [PubMed] [Google Scholar]
- 6.The Women's Health Resource. Breast cancer: statistics on incidence, survival, and screening. [citeted 2008 Jan 23]. Available from URL: http://www.imaginis.com/breast-health/breast-cancer-statistics-on-incidence-survival-andscreening-1 .
- 7.Cancer facts & figures 2010. Atlanta: American Cancer Society; 2010. American Cancer Society; pp. 9–10. [Google Scholar]
- 8.Kolahdoozan S, Sadjadi A, Radmard AR, Khademi H. Five common cancers in Iran. Arch Iran Med. 2010;13(2):143–6. [PubMed] [Google Scholar]
- 9.Farshbaf Khalili A, Shahnazi M, Ghahvechi A, Torabi Sh. Performance conditions of breast cancer screening methods and its efficient factors among women referring to health centers of Tabriz. Iranian J Nurs Res. 2009;4(12-13):27–38. (Persian) [Google Scholar]
- 10.Mousavi SM, Montazeri A, Mohagheghi MA, Jarrahi AM, Harirchi I, Najafi M, et al. Breast cancer in Iran: an epidemiological review. Breast J. 2007;13(4):383–91. doi: 10.1111/j.1524-4741.2007.00446.x. [DOI] [PubMed] [Google Scholar]
- 11.Hatefnia E, Niknami S, Bazargan M, Mahmoodi M, Lamyianm M, Alavi N. Correlates of mammography utilization among working Muslim Iranian women. Health Care Women Int. 2010;31(6):499–514. doi: 10.1080/07399331003725507. [DOI] [PubMed] [Google Scholar]
- 12.Marinho LAB, Costa-Gurgel MS, Cecatti JG, Osis MJD. Knowledge, attitude and practice of breast self-examination in health centers. Revista de Saúde Pública. 2003;37(5):576–82. doi: 10.1590/s0034-89102003000500005. (Spanish) [DOI] [PubMed] [Google Scholar]
- 13.Ferlay J, Bray F, Pisani P, Parkin D. GLOBOCAN 2002: cancer incidence, mortality and prevalence worldwide. IARC Cancerbase. 2004;5:20. [Google Scholar]
- 14.Dündar PE, Özmen D, Öztürk B, Haspolat G, Akyıldız F, Çoban S, et al. The knowledge and attitudes of breast self-examination and mammography in a group of women in a rural area in western Turkey. BMC Cancer. 2006;6:43. doi: 10.1186/1471-2407-6-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tabár L, Dean P. Mammography and breast cancer: the new era. Int J Gynaecol Obstet. 2003;82(3):319–26. doi: 10.1016/s0020-7292(03)00262-5. [DOI] [PubMed] [Google Scholar]
- 16.Gözüm S, Karayurt O, Kav S, Platin N. Effectiveness of peer education for breast cancer screening and health beliefs in eastern Turkey. Cancer Nurs. 2010;33(3):213–20. doi: 10.1097/NCC.0b013e3181cb40a8. [DOI] [PubMed] [Google Scholar]
- 17.Harris R, Leininger L. Clinical strategies for breast cancer screening: weighing and using the evidence. Ann Intern Med. 1995;122(7):539–47. doi: 10.7326/0003-4819-122-7-199504010-00011. [DOI] [PubMed] [Google Scholar]
- 18.Canbulat N, Uzun Ö. Health beliefs and breast cancer screening behaviors among female health workers in Turkey1. Eur J Oncol Nurs. 2008;12(2):148–56. doi: 10.1016/j.ejon.2007.12.002. [DOI] [PubMed] [Google Scholar]
- 19.Azizmohammadi S, Vakili MM, Mousaei Nasab N, Kiani K, Vaziri K. Survey on knowledge, attitude and student's skill about breast cancer in women Tarbiat Moallem Center of Zanjan (1999-2000) The Scientific Journal of Zanjan University of Medical Sciences. 2001;9(34):15–9. (Persian) [Google Scholar]
- 20.Avci IA. Factors associated with breast self-examination practices and beliefs in female workers at a Muslim community. Eur J Oncol Nurs. 2008;12(2):127–33. doi: 10.1016/j.ejon.2007.11.006. [DOI] [PubMed] [Google Scholar]
- 21.Parsa P, Kandiah M, Mohd Nasir MT, Hejar AR, Nor Afiah MZ. Reliability and validity of Champion's Health Belief Model Scale for breast cancer screening among Malaysian women. Singapore Med J. 2008;49(11):897–903. [PubMed] [Google Scholar]
- 22.Glanz K, Rimer BK, Lewis FM. 3rd ed. New Jersey: Jossey-Bass; 2002. Health behavior and health education: theory, research, and practice. [Google Scholar]
- 23.Sharifirad GR, Entezari MR, Kamran A, Azadbakht L. The effectiveness of nutritional education on the knowledge of diabetic patients using the health belief model. J Res Med Sci. 2009;14(1):1–6. [PMC free article] [PubMed] [Google Scholar]
- 24.Ghanbari A, Atrkar Roshan Z. A comparison between education by compact disc and booklet on learning outcome in nursing and midwifery students about breast self-examination. Journal of Guilan University of Medical Sciences. 2004;12(48):33–9. (Persian) [Google Scholar]
- 25.Hadizadeh Talasaz F, Latif Nejad R, Shamaian Razavi N. The effect of a training intervention on knowledge and practice of female students on breast self examination (BSE) Ofogh-e-danesh, Journal of Gonabad University of Medical Sciences and Health Services. 2002;8(2):67–74. (Persian) [Google Scholar]
- 26.Mazloomy SS, Zare M, Feisal M, Maleki F, Servat F, Ahmadieh MH. Effects of health education on knowledge, attitude and practice of female teachers in Yazd intermediate schools on breast cancer. Journal of Birjand University of Medical Sciences. 2006;13(1):12–8. (Persian) [Google Scholar]
- 27.Sørensen J, Hertz A, Gudex C. Evaluation of a Danish teaching program in breast self-examination. Cancer Nurs. 2005;28(2):141–7. [PubMed] [Google Scholar]
- 28.Karimi H, Sam SH. Effect of breast self-examination (BSE) education on increasing women's knowledge and practice, Ramsar. Journal of Babol University of Medical Sciences. 2004;7(3):61–8. (Persian) [Google Scholar]
- 29.Choudhry UK, Srivastava R, Fitch MI. Breast cancer detection practices of south Asian women: knowledge, attitudes, and beliefs. Oncol Nurs Forum. 1998;25(10):1693–701. [PubMed] [Google Scholar]
- 30.Vietri V, Poskitt S, Slaninka SC. Enhancing breast cancer screening in the university setting. Cancer Nurs. 1997;20(5):323–9. doi: 10.1097/00002820-199710000-00003. [DOI] [PubMed] [Google Scholar]
- 31.Aliyari SH, Zamaninejad A. Comparison of knowledge of women in army families from breast cancer screening methods pre and post education. Journal of Army University of Medical Sciences of The I.R.Iran. 2005;3(2):559–64. (Persian) [Google Scholar]
- 32.Tahvildary S, Shojaeizadeh D, Mohammad K, Mohagheghi M. The role of educating women for breast self-examination on women's awareness. Tehran University Medicine Journal. 1999;57(3):79–83. (Persian) [Google Scholar]
- 33.Sensiba ME, Stewart DS. Relationship of perceived barriers to breast self-examination in women of varying ages and levels of education. Oncol Nurs Forum. 1995;22(8):1265–8. [PubMed] [Google Scholar]
- 34.Patistea E, Chliaoutakis J, Darviri C, Tselika A. Breast self-examination.Knowledge and behavior of Greek female health care professionals working in primary health care centers. Cancer Nurs. 1992;15(6):415–21. [PubMed] [Google Scholar]
- 35.Katić M, Lang S, Budak A. Evaluation of the general practice program of women education for breast self-examination. Acta Med Croatica. 1996;50(4-5):185–91. [PubMed] [Google Scholar]
- 36.Ghazanfaree Z, Alemzadeh B, Nikian Y. An investigation on the knowledge and attitude of school teachers in Kerman city about breast self examination. Journal of Kerman University of Medical Sciences. 1995;2(2):76–80. (Persian) [Google Scholar]
- 37.Burnett CB, Steakley CS, Tefft MC. Barriers to breast and cervical cancer screening in underserved women of the district of columbia. Oncol Nurs Forum. 1995;22(10):1551–7. [PubMed] [Google Scholar]
- 38.Hadizadeh Talasaz F, Latif Nejad R. The effect of a training curriculum on attitude of female students about breast self-examination by using Health Belief Model (HBM) Journal of Birjand University of Medical Sciences. 2004;12(1-2):25–30. (Persian) [Google Scholar]
- 39.Fung SY. Factors associated with breast self-examination behaviour among Chinese women in Hong Kong. Patient Educ Couns. 1998;33(3):233–43. doi: 10.1016/s0738-3991(98)00023-8. [DOI] [PubMed] [Google Scholar]
- 40.Wardle J, Steptoe A, Smith H, Groll-Knapp E, Koller M, Smith D, et al. Breast self-examination: attitudes and practices among young women in Europe. Eur J Cancer Prev. 1995;4(1):61–8. [PubMed] [Google Scholar]


