Abstract
BACKGROUND:
Surgery for hip fractures can be done under general or neuraxial anesthesia. This study aimed to compare these two methods concerning their postoperative complications, duration of operation, hospitalization and the mortality rate within a period of one month after surgery.
METHODS:
400 patients aged more than 30 years old and scheduled for elective operative fixation of fractured hip, randomly enrolled in two equal groups of general (GA) and neuraxial (NA) anesthesia. Hemoglobin level was measured before and 6 hours, 2, 3 and 5 days after the surgery. The intra and postoperative blood loss, duration of surgery, the severity of pain at the time of discharge from recovery and at the 2nd, 3rd and 5th postoperative days were recorded. Statistical analysis was performed using SPSS version 12.0 by Mann-Whitney, chi-square, and t tests. P < 0.05 was considered significant.
RESULTS:
Both groups were similar regarding age, weight, and gender ratio. There was no significant difference in baseline hemoglobin, duration of surgery, length of hospitalization before surgery and the type of surgery. The mean of intraoperative blood loss and visual analogue score (VAS) in recovery and at the 3rd postoperative day, and also the length of hospitalization after surgery were significantly less in neuraxial anesthesia group. Both groups showed a significant decrease in hemoglobin values on the 2nd and 3rd postoperative days comparing to the baseline (p < 0.001).
CONCLUSIONS:
The morbidity and mortality rates of patients undergoing hip surgery were similar in both methods of anesthesia, but postoperative pain, blood loss, and duration of hospitalization were more in patients undergoing general anesthesia.
Keywords: General anesthesia, Neuraxial Anesthesia, Hip Fractures, Morbidity, Mortality
Hip fracture is a common challenging concept especially in the elders.1 Moreover, the patients who are scheduled for hip replacement surgery, usually have a high incidence of complications affect on morbidity and surgery costs.2
Hip fracture operations can be performed under general or neuraxial anesthesia.1,3,4 Over the past decades, these two methods of anesthesia for hip surgery have been compared concerning their complications during and after the surgery. Some studies mentioned the superiority of neuraxial anesthesia to general anesthesia in operative fixation of fractured hip in elderly.5 A retrospective meta-analysis demonstrated that incidence of deep vein thrombosis (DVT), myocardial infarction, hypoxia, and mortality in a period of one month after surgery was lower in patients undergoing neuraxial anesthesia for fractured hip reconstruction; while in patients receiving general anesthesia, the incidence of cerebrovascular accidents and the duration of operation was lower.1 Another retrospective study showed that the neuraxial anesthesia in arthroplasty of hip and knee have a slight protective effect against the thromboembolic events6; but, some others could not demonstrate a significant difference in mortality of patients undergoing fixation of traumatic fractured hip.7–10
Based on the fact that there were some defects in evaluation and comparing of complications and mortality of patients undergoing fixation of fractured hip, this study was designed to compare the two methods of general and neuraxial anesthesia completely.
Methods
In this prospective clinical trial, 400 patients older than 30 years old (in class 1, 2, and 3 of American Society of Anesthesiologists classification) who were scheduled for elective operative fixation of fractured hip, enrolled; all of them were admitted in Al-Zahra and Kashani Hospitals in Isfahan and all of them signed informed consent from. This study was approved by the Ethics Committee of Isfahan University of Medical Sciences.
Patients were included if they had no dementia or cognitive dysfunctions and no history of opioid or psychotic drugs use. Patients with hypersensitivity to blood transfusion, sever reaction to cement implantation, sever bleeding, hypotension needed interventions, prolonged operation changed surgical plan which impressed the study goals, were excluded.
An anesthesiologist visited all the patients a night before surgery and any known history of hematologic, endocrine, cardiovascular, pulmonary, and central nervous system diseases were noted. Also, systolic, diastolic, and mean arterial pressures were recorded.
Patients were randomly assigned into two groups using random-number table: GA (general anesthesia) and NA (neuraxial anesthesia). All patients were infused Ringer's lactate solution (4 ml/kg) on arrival in the operating room and also received low dose of heparin as a DVT prophylaxis. Systolic, diastolic, and mean arterial pressures were recorded before induction of anesthesia by anesthesiologist.
In the GA group, patients were given Ringer's lactate solution (10 ml/kg) to oppose the vasodilatation and hypotension resulting from intravenous anesthetics during induction of anesthesia. Patients were not pre-medicated. They received a standardized general anesthesia involving pre-oxygenation and induction with fentanyl (2 μg/kg) followed by thiopental (5 mg/kg) until loss of consciousness; then lidocaine (1.5 mg/kg) and pancuronium (0.1 mg/kg) were administered. Anesthesia was maintained using halothane (0.5-1.5%) in oxygen and nitrous oxide (ratio 1:1). Mechanical ventilation with a constant tidal volume of 10 ml/kg and respiratory rate of 12 per minute was maintained throughout the study. At the end of the operation, the volatile anesthetic agents were discontinued and residual neuro-muscular block was antagonized with intravenous prostigmin (0.04 mg/kg) and atropine (0.02 mg/kg). The lungs were ventilated manually with 100% oxygen until spontaneous ventilation resumed. Extubation was performed when the patient was judged to be awake.
In the NA group, patients were given Ringer's lactate solution (15 ml/kg) prior to the induction of anesthesia and received either spinal or epidural anesthesia. After sterile preparation and draping, in spinal anesthesia group, plain bupivacaine 0.5% (3 ml) was injected over 10 seconds into the subarachnoid space at the L3-L4 interspace via 23-G Withacre needle placed midline approach. In the epidural group, anesthesia was performed using an 18-G-Touhy needle at the L3-L4 interspace and after an initial test dose of plain bupivacaine 0.5% (5 ml) with epinephrine (1:200000) was injected followed 5 minutes later by a further 20 ml.
All patients were monitored by non-invasive electrocardiogram, blood pressure, and pulse oxymetry. Additionally, end-tidal carbon dioxide (Etco2) was monitored and maintained within 35-40 mmhg during operation in the GA group.
In both groups, preloading with Ringer's lactate solution prevented sever reduction in blood pressure and kept mean of arterial pressure above 70% of baseline levels in hypertensive patients and above 65 mmhg in normotensive patients.3 Blood pressure was measured every 15 minutes and if it fell to below these limits, halothane was reduced gradually in the GA group and an additional 10 ml/kg Ringer's lactate solution was infused in a period of 10 minutes in the NA group to reestablish the acceptable blood pressure.11 If the blood pressure did not respond after these interventions, 5-10 mg bolus of intravenous ephedrine, according to the degree of hypotension, was administered. The second dose was repeated after 5 minutes if the blood pressure was not normalized. Five minutes after the second dose of ephedrine, if the mean arterial pressure was still less than 70% of its baseline value, further ephedrine boluses were administered, and the case regarded as a failure in the study.
Hemoglobin level was measured before surgery (baseline), 6 hours, and 2, 3, and 5 days after the end of it. The total estimated intraoperative blood loss was recorded at the end of each surgery with bloody gauze counting and measuring volume of suction bottles; also, the amount of postoperative hemorrhage was measured according to its volume in hemovac drain.
The time interval between the induction of anesthesia (GA or NA) and dressing of the site of operation was recorded as the duration of surgery.
Postoperative pain severity was evaluated using a visual analogue scale (VAS) ranging from 0 (no pain) to 10 (worst possible pain). The VAS was evaluated by a nurse at the time of discharge from recovery room and by a second nurse on the ward at the 2nd, 3rd, and 5th day after surgery. Observers were not aware of group assignment. Intravenous morphine (5 mg) was administered to the patients re-quested analgesia and its total amounts were recorded till 5 days after the end of surgery. Cognitive dysfunctions were noted before discharge from recovery room, and at 24 and 48 hours after the end of the surgery based on time, person, and place disorientation.
Postoperative complications such as deep veins thrombosis, congestive heart failure, myocardial infarction, atelectasis, pulmonary infection, and cerebrovascular accidents are diagnosed by the consultant specialist. The number of patients who died over one month period in the hospital or after discharge from it was recorded.
The data were analyzed using SPSS statistical package (version 12, SPSS Inc., Chicago, IL). Frequencies were compared by Mann-Whitney and chi-square tests, as appropriate, and t-test was used to compare the averages. Significance level was set at p < 0.05.
Results
During the study period, 400 consecutive patients with the required surgical indication were included. Three patients of the GA group and 10 of the NA group were excluded because of change in anesthetic or surgical plan. Recruitment ended with the completion of the protocol in the 387th patient. One hundred and ninety-seven (50.9%) patients were allocated to the GA group, whereas 190 (49.1%) patients constituted the NA group. Of 190 neuraxial anesthesia patients, 164 (42.4%), 1 (4%) and 22 (5.7%) received spinal, epidural and continuous epidural anesthesia, respectively.
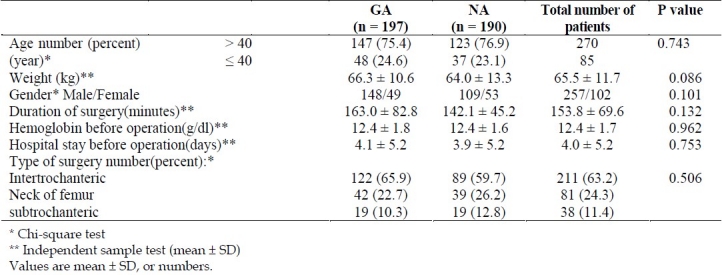
Patients and surgical characteristics, baseline hemoglobin and length of stay in hospital before surgery are listed in table 1. Groups are similar regarding age, weight and gender ratio.
Table 1.
Patient characteristics, preoperative hemoglobin values, duration of hospitalization, and some intraoperative data in the general anesthesia group (GA) and neuroaxial group (NA)
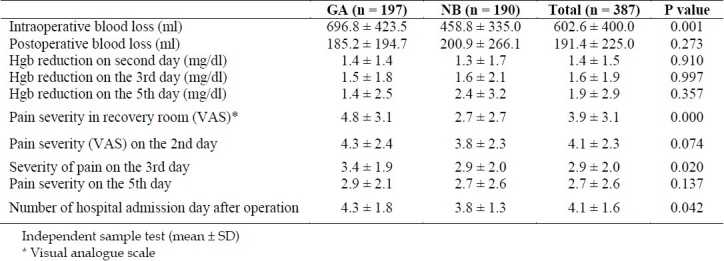
The mean of intraoperative blood loss, mean of VAS scores in recovery and on the 3rd postoperative day, and also the length of stay in hospital after surgery in the NA group were significantly less than the GA group. Both groups showed a significant decrease in hemoglobin values on the 2nd and 3rd postoperative days comparing to the baseline values (p < 0.001) (Table 2).
Table 2.
The mean intra- and post-operative blood loss, hemoglobin changes, pain scores and the duration of hospitalization in both groups
There was no significant difference between two groups regarding the abundance of cardiovascular and respiratory complications (Table 3). No patients in either group suffered from cardiac insufficiency, deep vein thrombosis, or cerebral events. In the NA group, one patient developed pulmonary emboli on the 4th postoperative day.
Table 3.
Frequency of postoperative complications and mortality rate in both groups
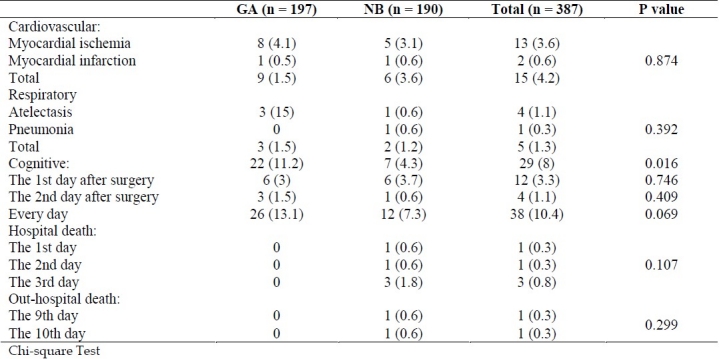
The number of patients who developed cognitive dysfunction in recovery room was signifycantly higher in the GA group compared with the NA group.
Although the number of patients who died was more in the NA group, but no significant difference was found between the two groups for in-hospital and out-hospital mortality.
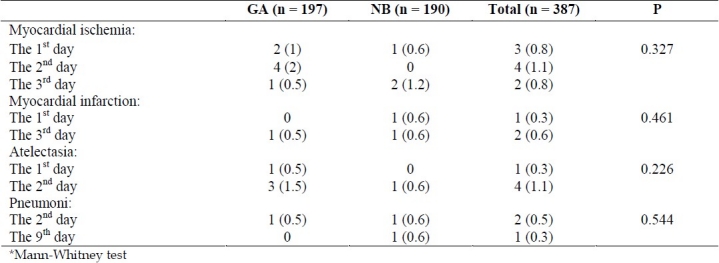
The abundance of the cardiac and respiratory complications is shown in table 4. On the 2nd postoperative day, there was a greater incidence of cardiac ischemic events and respiratory complications in both groups. Also, myocardial infarction was reported more on the 3rd postoperative day, although this difference was not statistically significant. The mean of ephedrine doses (0.8 ± 4.4 vs. 3.2 ± 8.1 mg administered to the GA and NA groups respectively) was statistically significant (p < 0.001). Also, the mean of morphine consumption in the GA group (5.0 ± 6.3 mg) was higher than the NA group (3.4 ± 7.4 mg) (p = 0.004).
Table 4.
Frequency of cardiovascular and respiratory complications on the basis of postoperative days in both groups*
Discussion
This study showed that the mean of blood loss during operation was significantly more in patients receiving general anesthesia than neuraxial anesthesia. In two previous separate meta-analysis assessing the patients undergoing different surgical procedures12 and the candidates of hip and spinal column surgeries, the researchers demonstrated that general anesthesia is accompanied by more hemorrhage compared with neuraxial anesthesia.12,13
In a review article, Macfarlane et al reported that in four out of ten studies, patients receiving GA had significantly more bleeding, and in the other six there was no significant difference between groups considering blood loss.14 They reported that the mean of reduction of blood loss was different from 118 ml to 595 ml, but in our study this value was 238 ml.
In a prospective controlled study, patients undergoing hip surgery under spinal anesthesia had less blood loss than patients receiving general anesthesia.15
Neuraxial anesthesia blocks alpha and beta adrenergic receptors, leads to reduction of heart rates, vascular tone, and blood pressure. The decreased blood pressure acts like controlled hypotension which results in less blood loss.16 In this study, the amount of intraoperative ephedrine consumption to oppose hypotension was significantly more in neuraxial method than in general anesthesia. Thus the established intraoperative hypotension is in an accepted limitation, it can explain the less blood loss in neuraxial anesthesia patients. The other justifying reason can be an increase in venous blood pressure in patients receiving general anesthesia especially with mechanical ventilation.17 In this study there was no difference between the groups regarding postoperative blood loss amount and the hemoglobin changes until the 5th postoperative day; but in both groups the mean of hemoglobin changes was statistically lower on the 2nd and 3rd postoperative days compared to preoperative values.
In our study, the mean of duration of hospitalization was significantly more in patients receiving general anesthesia. Møiniche et al surveyed 42 volunteers of hip surgery undergoing general or continuous epidural anesthesia and found that the duration of hospitalization was similar in both groups.18 The difference may be attributed to their smaller studied population and applying only one method of neuraxial anesthesia which was continuous epidural anesthesia. Sutcliffe and Parker in a retrospective study found no difference in factors of hospitalization in 1333 patients receiving either general or neuraxial anesthesia for hip surgery.19 This contradiction can be due to the different kind of studies. They studied retrospectively while our study was a prospective one.
Vaida et al declared that the beneficial effects of neuraxial analgesia are reduction of stress hormones, inhibition of central hyper sensitization and ultimately shortening the duration of hospitalization. They believed that increase in pain severity and cognitive dysfunction in patients receiving general anesthesia resulted in longer hospitalization.20 Our findings demonstrated that the pain severity, especially at recovery room and on the 3rd aostoperative day was lower in neuraxial group.
Moreover, Gonano et al studied 40 volunteers of hip and knee surgeries and reported that spinal anesthesia accompanied by less postoperative pain compared to general anesthesia.21 Furthermore, a meta-analysis on 1362 patients reported that neuraxial anesthesia or peripheral nerve block leads to less postoperative pain.22 Additionally, a review article reported that in ten of eleven studies, patients receiving epidural anesthesia significantly suffered less pain than general anesthesia groups.14 The reduction in pain severity at recovery room can be attributed to the residual effects of sensory block of neuraxial anesthesia. Also, the lower pain on postoperative days may be due to the beneficial effects of preemptive analgesia in neuraxial anesthesia application.
In our study, the frequency of postoperative events, including cardiovascular and respiratory complications, were similar in both groups. In fact, there was no statistically deference in the incidence of myocardial ischemia, myocardial infarction, atelectasia, and pulmonary infection between groups. Our results were different from the results of Urwin et al study1; in their study, incidence of DVT and myocardial infarction in patients undergoing correction of fractured hip surgery under neuraxial anesthesia was lower than general anesthesia patients. Meanwhile, the incidence of cerebrovascular accidents and intraoperative hypotension were lower in patients receiving general anesthesia.1 The reasons for differences in findings might be due to the difference in sample size and the kind of the study. In other words, they evaluated 2161 patients retrospectively while we studied 387 patients prospectively.
In a meta-analysis, a lower incidence of DVT and pulmonary emboli in patients receiving neuraxial anesthesia for hip surgery was showed.15 However, O’Hara et al reported no significant difference in incidence of postoperative myocardial infarction, congestive heart failure (CHF), and mental dysfunction between both groups receiving either general or neuraxial anesthesia in a retrospective study.9 This finding was similar to the present study. We also found no statistical difference in mental dysfunction on the 2nd and 3rd postoperative days between the groups. This was in similarity to the findings of some previous studies.9,23
Our results revealed that patients receiving general anesthesia had more mental dysfunction in recovery room. This difference might be due to the remaining effect of anesthetic drugs at recovery room.
In our study, there was no difference in the abundance of death during hospital stay and out of hospital till 30 days after surgery. In one study on 425 patients in a primary investigation, they reported that the anesthetic technique has a role in morbidity and mortality of patients. But, after controlling the differences of the studied groups, they revealed that there is no difference in morbidity and mortality rate between the groups.16 Thus, the authors concluded that the major reasons for morbidity and mortality of these patients are their coexisting disease (e.g. diabetes, cardiovascular disease, etc), elderly, and undesirable physical condition and not an anesthetic technique. In limited studies, the difference in the incidence of mortality and morbidity after neuraxial and general anesthesia was reported. For example, in one study, 53 high risk patients were evaluated and the results showed a lower incidence of morbidity and mortality after epidural anesthesia compared to general anesthesia.24 In another clinical trial, the effect of anesthetic techniques was not proved.25 But in another study, the effect of neuraxial anesthesia on short term mortality was drawn but it had not differ from general anesthesia considering long term mortality.26 In fact, in a majority of the studies, we may not be able to rely on the results due to the small sample size and a low study power.
As in our study, the sample size was calculated according to the major postoperative complications, the absence of significant difference in mortality might be attributed to small sample size. This would be possibly considered as a weakness of this study. Moreover, due to the limitation in performance of some specific diagnostic tests or the mildness of some clinical signs of diseases, there is a possibility that some postoperative complications might be undiagnosed. Therefore, this issue might be considered as a limitation of this study. Also, one of the limitations of our study was lack of some predictors such as sickness at admission scale or acute physiologic score from the APPACHE I and ASA; so we cannot conclude that mortality is due to anesthetic techniques or coexisting diseases.
Conclusions
In conclusion, this clinical investigation demonstrated that general and neuraxial anesthesia have a similar incidence of postoperative complications and mortality in candidates of hip surgery. We believe that because of the less intraoperative hemorrhage, shorter hospital stay, and lower postoperative pain in patients undergoing neuraxial anesthesia for hip surgery, this technique is superior as compared to general anesthesia.
In a summary, the results suggest that more controlled studies with larger sample size and more precise diagnostic tests, in multiple centers are needed to eliminate the limitations of our study.
Authors’ Contributions
SMH collected the data and helped to write the manuscript. HS was one of the members of reaserch team and also helped to write the manuscript. SJH was one of the members of reaserch team, also helped to write the manuscript, and corrected the manuscript according to reviewers’ comments. RT was one of the members of reaserch team and also helped to write the manuscript. BS did statistical analysis. All authors have read and approved the content of the manuscript.
Footnotes
Conflict of Interests Authors have no conflict of interests.
References
- 1.Urwin SC, Parker MJ, Griffiths R. General versus regional anesthesia for hip fracture surgery: a meta-analysis of randomized trials. BJA. 2000;84(4):450–5. doi: 10.1093/oxfordjournals.bja.a013468. [DOI] [PubMed] [Google Scholar]
- 2.Morand EF, Littlejohn GO. Medical problems in joint replacement patients: a retrospective study of 243 total hip arthroplasties. Med J Aust. 1990;152(8):408–13. doi: 10.5694/j.1326-5377.1990.tb125267.x. [DOI] [PubMed] [Google Scholar]
- 3.Rushman GB, Davies NJH, Cashman JN. 12th ed. Oxford: Butterworth-Heinemann; 1999. Lee's synopsis of anaesthesia; pp. 469–272. [Google Scholar]
- 4.Stoelting RK, Dierdorf SF. 4th ed. New York: Churchill Livingstone; 2002. Anesthesia and co-existing disease; p. 747. [Google Scholar]
- 5.Davis FM, Woolner DF, Frampton C, Wilkinson A, Grant A, Harrison RT, et al. Prospective, multi-centre trial of mortality following general or spinal anaesthesia for hip fracture surgery in the elderly. Br J Anaesth. 1987;59(9):1080–8. doi: 10.1093/bja/59.9.1080. [DOI] [PubMed] [Google Scholar]
- 6.Goméz Navalón L, Marín Morales L, Zorrilla Ribot P, Martínez Delgado C, Salido Valle J. Spinal anesthesia: a protective factor in thromboembolic disease.A retrospective cohort study of 484 arthroplasties. Rev Esp Aneste-siol Reanim. 2001;48(3):113–6. (Spanish) [PubMed] [Google Scholar]
- 7.Sorenson RM, Pace NL. Anesthetic techniques during surgical repair of femoral neck fractures.A meta-analysis. Anesthesiology. 1992;77(6):1095–104. doi: 10.1097/00000542-199212000-00009. [DOI] [PubMed] [Google Scholar]
- 8.Breen P, Park KW. General anesthesia versus regional anesthesia. Int Anesthesiol Clin. 2002;40(1):61–71. doi: 10.1097/00004311-200201000-00006. [DOI] [PubMed] [Google Scholar]
- 9.O’Hara DA, Duff A, Berlin JA, Poses RM, Lawrence VA, Huber EC, et al. The effect of anesthetic technique on postoperative outcomes in hip fracture repair. Anesthesiology. 2000;92(4):947–57. doi: 10.1097/00000542-200004000-00011. [DOI] [PubMed] [Google Scholar]
- 10.Gilbert TB, Hawkes WG, Hebel JR, Hudson JI, Kenzora JE, Zimmerman SI, et al. Spinal anesthesia versus general anesthesia for hip fracture repair: a longitudinal observation of 741 elderly patients during 2-year follow-up. Am J Orthop (Belle Mead NJ) 2000;29(1):25–35. [PubMed] [Google Scholar]
- 11.Kirby RR, Gravenstein N, Lobato EB, Gravenstein JS. 2nd ed. Philadelphia: W.B. Saunders; 2002. Clinical anesthesia practice; p. 584. [Google Scholar]
- 12.Guay J. The effect of neuraxial blocks on surgical blood transfusion requirements: a meta-analysis. J Clin Anesth. 2006;18(2):124–8. doi: 10.1016/j.jclinane.2005.08.013. [DOI] [PubMed] [Google Scholar]
- 13.Richman JM, Rowlingson AJ, Maine DN, Courpas GE, Weller JF, Wu CL. Does neuraxial anesthesia reduce intraoperative blood loss? A meta-analysis. J Clin Anesth. 2006;18(6):427–35. doi: 10.1016/j.jclinane.2006.02.006. [DOI] [PubMed] [Google Scholar]
- 14.Macfarlane AJ, Prasad GA, Chan VW, Brull R. Does regional anaesthesia improve outcome after total hip arthroplasty? A systematic review. Br J Anaesth. 2009;103(3):335–45. doi: 10.1093/bja/aep208. [DOI] [PubMed] [Google Scholar]
- 15.Mauermann WJ, Shilling AM, Zuo Z. A comparison of neuraxial block versus general anesthesia for elective total hip replacement: a meta-analysis. Anesth Analg. 2006;103(4):1018–25. doi: 10.1213/01.ane.0000237267.75543.59. [DOI] [PubMed] [Google Scholar]
- 16.Barbier-Böhm G, Desmonts JM, Couderc E, Moulin D, Prokocimer P, Olivier H. Comparative effects of induced hypotension and normovolaemic haemodilution on blood loss in total hip arthroplasty. Br J Anaesth. 1980;52(10):1039–43. doi: 10.1093/bja/52.10.1039. [DOI] [PubMed] [Google Scholar]
- 17.Modig J. Regional anesthesia and blood loss. Acta Anaesthesiol Scand. 1988;32(Suppl s89):44–8. doi: 10.1111/j.1399-6576.1988.tb02842.x. [DOI] [PubMed] [Google Scholar]
- 18.Møiniche S, Hjortsø NC, Hansen BL, Dahl JB, Rosenberg J, Gebuhr P, et al. The effect of balanced analgesia on early convalescence after major orthopaedic surgery. Acta Anaesthesiol Scand. 1994;38(4):328–35. doi: 10.1111/j.1399-6576.1994.tb03902.x. [DOI] [PubMed] [Google Scholar]
- 19.Sutcliffe AJ, Parker M. Mortality after spinal and general anaesthesia for surgical fixation of hip fractures. Anaesthesia. 1994;49(3):237–40. doi: 10.1111/j.1365-2044.1994.tb03430.x. [DOI] [PubMed] [Google Scholar]
- 20.Vaida SJ, Ben David B, Somri M, Croitoru M, Sabo E, Gaitini L. The influence of preemptive spinal anesthesia on postoperative pain. J Clin Anesth. 2000;12(5):374–7. doi: 10.1016/s0952-8180(00)00174-4. [DOI] [PubMed] [Google Scholar]
- 21.Gonano C, Leitgeb U, Sitzwohl C, Ihra G, Weinstabl C, Kettner SC. Spinal versus general anesthesia for orthopedic surgery: anesthesia drug and supply cost. Anesth Analg. 2006;102(2):524–9. doi: 10.1213/01.ane.0000194292.81614.c6. [DOI] [PubMed] [Google Scholar]
- 22.Liu SS, Strodtbeck WM, Richman JM, Wu CL. A comparison of regional versus general anesthesia for ambulatory anesthesia: a meta-analysis of randomized controlled trials. Anesth Analg. 2005;101(6):1634–42. doi: 10.1213/01.ANE.0000180829.70036.4F. [DOI] [PubMed] [Google Scholar]
- 23.Singh N, Sidawy AN, Dezee K, Neville RF, Weiswasser J, Arora S, et al. The effect of the type of anesthesia on outcomes of lower extremity infrainguinal bypass. J Vasc Surg. 2006;44(5):964–8. doi: 10.1016/j.jvs.2006.06.035. Discussion 968-70. [DOI] [PubMed] [Google Scholar]
- 24.Rodgers A, Walker N, Schug S, McKee A, Kehlet H, van Zundert A, et al. Reduction of postoperative mortality and morbidity with epidural or spinal anaesthesia: results from overview of randomised trials. BMJ. 2000;321(7275):1493. doi: 10.1136/bmj.321.7275.1493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Barbosa FT, Cavalcante JC, Jucá MJ, Castro AA. Neuraxial anaesthesia for lower-limb revascularization. Cochrane Database Syst Rev. 2010;(1):CD007083. doi: 10.1002/14651858.CD007083.pub2. [DOI] [PubMed] [Google Scholar]
- 26.Parker MJ, Handoll HH, Griffiths R. Anaesthesia for hip fracture surgery in adults. Cochrane Database Syst Rev. 2001;(4):CD000521. doi: 10.1002/14651858.CD000521. [DOI] [PubMed] [Google Scholar]


