Abstract
BACKGROUND:
This study was performed to compare the outcomes of open surgical procedure and percutaneously peritoneal dialysis catheter (PDC) insertion using laparoscopic needle.
METHODS:
This randomized clinical trial study was conducted in the Nephrology Department in Noor Hospital, Isfahan, Iran between 2009 and 2010. 64 uremic patients were randomized into two study groups using random allocation software. Thirty four catheters were inserted percutaneously (P group) and 30 catheters were placed surgically (S group). Collected information included demographic data, body mass index, and cause of renal disease, duration of operation and length of hospitalization. Outcomes were considered as mechanical and infectious complications.
RESULTS:
There were no significant differences in age, gender, the mean of body mass index, having history of hemodialysis, diabetes mellitus, hypertension, ischemic heart disease, and length of hospitalization. Hemopenitoneom was more frequent in S group than P group (13.3% versus 3.2%; p < 0.0001). There was no significant difference between two groups in early peritonitis, early leakage, hernia, hollow viscous perforation, catheter obstruction, and malpositioning and the time of peritoneal dialysis onset. Outflow failure and the exit site infection were more frequent in S group than P group (p < 0.0001). Mean of the operative time was longer in S group than P group (27.70 ± 2.79 minutes versus 10.48 ± 1.91 minutes, p < 0.001).
CONCLUSIONS:
Percutaneous catheter insertion has fewer rate of complications and is less time consuming in comparison with surgical method.
KEYWORDS: Laparoscopy, Needles, Catheter Ablation, Peritoneal Dialysis
Peritoneal dialysis is one of the modalities in renal replacement therapy.1 Peritoneal dialysis catheter (PDC) is usually inserted by a surgeon, by laparoscopic or surgical method.2 In many centers, laparoscopic PDC placement is an acceptable method. It has many advantages such as safety, low rate of complications, catheter dysfunction and longer catheter survival in spite of surgical procedure.3,4 There are well-known important causes of morbidity which are catheter related complications such as leakage, tunnel and exit site infection, tip malposition, hernia and peritonitis.5 Surgical placement of PDC is started by a laparotomy or a laparoscopy procedure. Percutaneous PDC placement can be performed by an interventional nephrologist or surgeon to provide a fast, safe, and reliable peritoneal access.6
Henderson et al have reported that the insertion of the catheter by percutaneous method was easy and PDC was inserted successfully with a very low complication rate, and there was not any need for general anesthesia.7 Therefore this study was performed to compare the outcomes of open surgical procedure and percutaneously peritoneal dialysis catheter (PDC) insertion using laparoscopic needle.
Methods
This randomized trial study was conducted in the Department of Nephrology at Noor University Hospital, Isfaha, Iran during 2009 and 2010. The Ethics Committee of Isfahan University of Medical Sciences approved the study protocol (Research project number 288132). 64 uremic patients were randomized into two study groups by random allocation software. All subjects signed a consent form permitting catheter use.
Collected information for this study included demographic data, body mass index (BMI), and having history of hemodialysis, diabetes mellitus, hypertension, and ischemic heart disease, selection cause of peritoneal dialysis (PD), duration of operation (minute) and duration of hospitalization (day). Data were extracted from a check list included history, clinical assessment and treatment given to patients. Outcome was considered as infectious and mechanical complications. Exit site infection confirmed by redness, purulent discharge and peritonitis. Mechanical complications were considered as PDC out flow failure, fluid leak from, hemopenitoneom, hollow viscous perforation, and incisional site hernia. Patients were followed for two months with respect to mechanical and infectious complications. Inclusion criteria were having stage 5 chronic kidney disease (according to national kidney foundation guideline) which needed renal replacement therapy; self-care ability, patient's consent and having family support for choosing Continuous Ambulatory Peritoneal Dialysis (CAPD) as a choice of therapeutic modality,8 and being aged over 18 years old. Exclusion criteria were having morbid obesity (BMI more than 35 kg/m2), ventral or inguinal hernia,9 or any history of abdominal surgery.
Thirty of the 64 inserted PDCs were placed surgically (S group) and 34 were placed percutaneously (P group).
For the percutaneous placement, under aseptic condition and local anesthesia with lidocaine 2% installation and mild sedation (5 mg midazolam, intravenous), 2 cm transverse incision was made on the skin, 2 cm below the umbilicus.10 Linea Alba was sutured by vicrill 0-2, and pulled up; Veress laparoscopic needle (spring-loaded needle generally used for creating pneumoperitoneum in laparoscopic surgery) was inserted in peritoneal cavity through linea Alba.11 One liter of normal saline was infused in the abdominal cavity through laparoscopic needle.
A guide wire was inserted through the needle, and the needle was removed. A 18 French dilator and split sheath was inserted over the guide wire then the dilator and guide wire removed and swan neck coil peritoneal dialysis catheter with 2 felt cuffs was inserted and advanced through the sheath. Then two parts of sheath were divided and removed (Figure 1). First cuff fixed on linea Alba with absorbable suture (vicrill 2-0). Thereafter a tunnel was constructed with the exit site caudally 1-2 cm distal to the subcutaneous cuff.5 Then with plain radiography we ensured the pelvic positioning of catheter.
Figure 1.
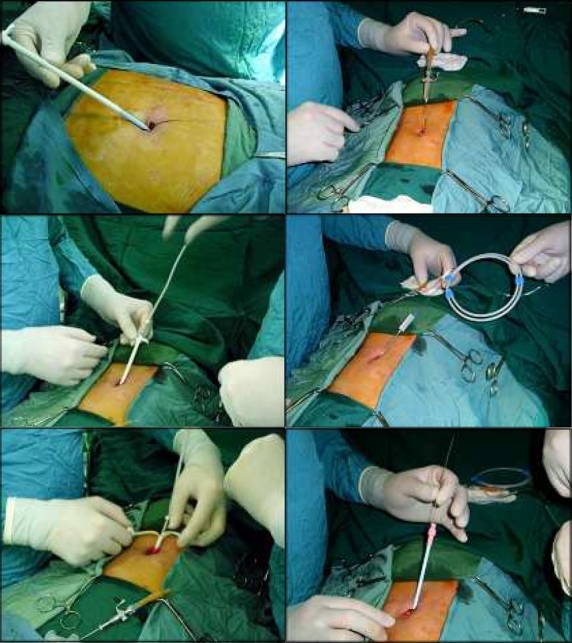
Sequencial pictures of percutaneous peritoneal dialysis catheter insertion
Figure 2.
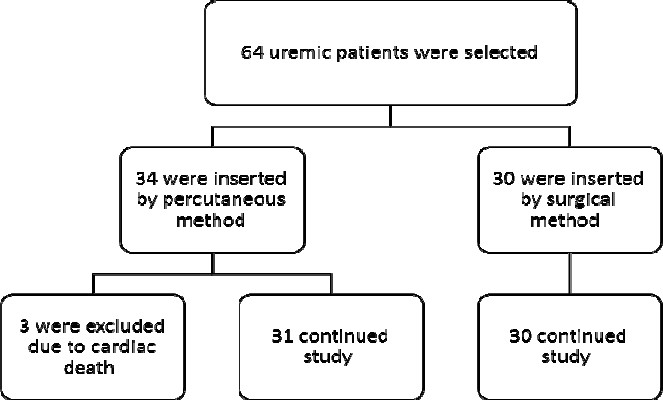
Study design flow chart
All data were analyzed by PASW 18 (IBM Corporation Company, USA). Chi square, Student-t, and Fisher exact tests were used for analysis. P values less than 0.01 were considered significant.
Results
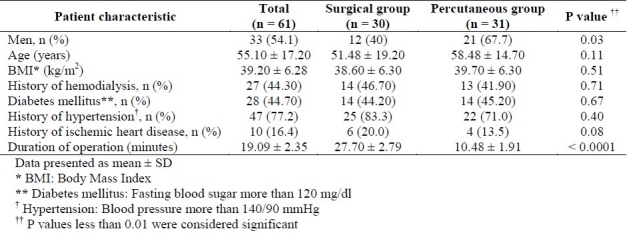
61 of 64 selected patients were enrolled in this study. Patients’ characteristics of both groups are shown in table 1. There were no significant differences in age, gender, the mean of BMI, having history of hemodialysis, diabetes mellitus (fasting blood sugar more than 126 mg/dl), ischemic heart disease,12 hypertension (blood pressure more than 140/90 mmHg), and selection cause of peritoneal dialysis (PD), and duration of hospitalization.
Table 1.
Demographic features and clinical details of two study groups
Three patients, in which the PDCs were placed percutaneously, were dead unrelated to procedure and due to myocardial infarction and were excluded from the study. Mechanical and infectious complications were encountered during the two month follow-up period (Table 2). Hemopenitoneom was more frequent in S group rather than P group (13.3% versus 3.2%, p < 0.0001). There were no cases of incisional hernia and hollow viscous perforation in both groups during two month follow-up study. Catheter malposition was seen in four patients (2 in each group) and they needed correction of the tip of catheter site (p = 0.36).
Table 2.
Comparison of complications in both study groups
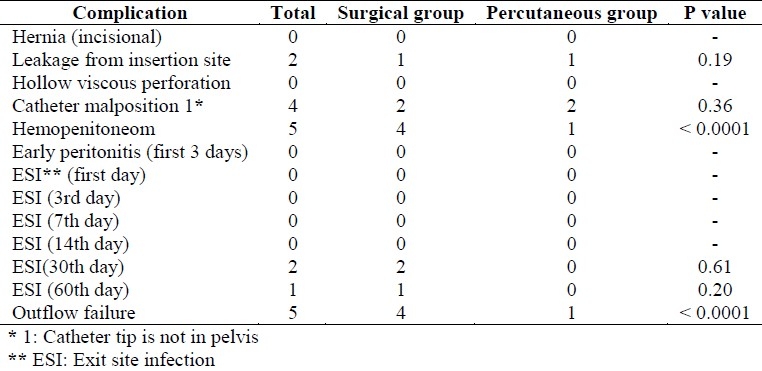
Fluid leakage was seen in one patient in each group. In our series, the total of 5 cases complicated by wrapped omentom and they needed surgical omentectomy (four in the S and one in the P group, p < 0.0001).
There were no cases of site infection and early peritonitis in either groups at the 1st, 3rd, 7th, 14th day of follow-up. Although no exit site infection was observed in P group after two months, it was not a statistically significant difference (p = 0.2). Mean of operation duration was longer in S group rather than P group 27.70 ± 2.79 minutes versus 10.48 ± 1.91 minutes, p < 0.0001).
Discussion
Varughese et al reported their experience in 34 percutaneous PD catheter insertions. Duration of hospitalization for these patients was approximately 3 days in comparison to 7-10 days in those for whom laparotomy and surgical placement were used. There was no fluid leakage. One patient had an injury to the hollow viscous and mesenteric artery. They needed emergency laparotomy and ligation of the bleeding vessel. Another patient had bloody drain fluid which managed conservatively. In three patients, the drain of peritoneal fluid was inadequate, presumably due to omental wrapping around the in-dwelling catheter, and needed surgical omentectomy. Percutaneous catheter insertion is extremely simple to perform and, in comparison to laparotomy, reduces the duration of hospitalization.13 In our series there were no significant differences in hospitalization time in both groups. In addition there was not any serious complication like visceral or vascular perforation. Also fluid leakage was the same in both groups.
Ozener et al suggested that in comparison to surgical technique, percutaneous insertion of PDC has the same catheter-related mechanical and infectious complications.14 This study showed that there is no significant difference between two methods of catheter insertion, however some of complications (hemopenito-neom and outflow failure) were seen more common in surgical method than percutaneous method.
Mellotte et al retrospectively reviewed the clinical outcomes of 230 PDC insertions, fifty were placed percutaneously and 180 were placed through surgical techniques. Inserted percutaneous PDC was non-elective in a procedure room beside the nephrology ward. Percutaneous group were older (p < 0.001) and had increased early mortality (p < 0.005) due to cause of renal disease. They concluded that percutaneous PDC placement provides a safe, reliable access for peritoneal dialysis and is especially suitable for critically ill patients.15 In this study there were 3 deaths in P group and they were not related to catheter insertion method, but due to underlying coronary artery events. We excluded them and there is no statistical analysis in this manner, but it seems we are the same in this complication.
Tiong et al showed that, 31% of percutaneous inserted catheters had early complications, which most of them were wound infections and catheter malfunctions. Catheter insertion for peritoneal dialysis is associated with remarkable surgical morbidity. Also, surgical time is prolonged and patients with previous abdominal surgery are at increased risk of morbidity and complication.16 Yang PJ et al reported their results in mini laparotomy for PDC insertion in which exit site and tunnel infection were the most common complication (11.8%), in expert surgeon hand with a good post-operative care.17 They did not compare their series with percutaneous method. In our series percutaneous method is less time consuming with fewer complications so it can be done faster even in an emergency situation.
This study was done on a small group of uremic patients in an elective situation; further studies should be performed on larger groups in both elective and urgent situations to evaluate this method of PDC insertion in acute renal dysfunction.
Conclusions
Percutaneous catheter insertion has fewer rate of complications and is less time consuming in comparison with surgical method.
Authors’ Contributions
All the authors have carried out the study, participated in the design of the study and acquisition of data performed the statistical analysis and wrote the manuscript. All authors read and approved the final manuscript.
Acknowledgments
This paper is a part of research project with Isfahan Kidney Disease Research Center. Authors wish to thank a group of respected experts in Universities of medical sciences and locals for their assistance in data collection.
Footnotes
Conflict of Interests
Authors have no conflict of interests.
References
- 1.Bar-Zohar D, Sagie B, Lubezky N, Blum M, Klausner J, bu-Abeid S. Laparoscopic implantation of the Tenckhoff catheter for the treatment of end-stage renal failure and congestive heart failure: experience with the pelvic fixation technique. Isr Med Assoc J. 2006;8(3):174–8. [PubMed] [Google Scholar]
- 2.Al-Hashemy AM, Seleem MI, Al-Ahmary AM, Bin-Mahfooz AA. A two-port laparoscopic placement of peritoneal dialysis catheter: a preliminary report. Saudi J Kidney Dis Transpl. 2004;15(2):144–8. [PubMed] [Google Scholar]
- 3.Schmidt SC, Pohle C, Langrehr JM, Schumacher G, Jacob D, Neuhaus P. Laparoscopic-assisted placement of peritoneal dialysis catheters: implantation technique and results. J Laparoendosc Adv Surg Tech A. 2007;17(5):596–9. doi: 10.1089/lap.2006.0162. [DOI] [PubMed] [Google Scholar]
- 4.Haggerty SP, Zeni TM, Carder M, Frantzides CT. Laparoscopic peritoneal dialysis catheter insertion using a Quinton percutaneous insertion kit. JSLS. 2007;11(2):208–14. [PMC free article] [PubMed] [Google Scholar]
- 5.Banli O, Altun H, Oztemel A. Early start of CAPD with the Seldinger technique. Perit Dial Int. 2005;25(6):556–9. [PubMed] [Google Scholar]
- 6.Sampathkumar K, Mahaldar AR, Sooraj YS, Ramkrishnan M, Ajeshkumar, Ravichandran R. Percutaneous CAPD catheter insertion by a nephrologist versus surgical placement: A comparative study. Indian J Nephrol. 2008;18(1):5–8. doi: 10.4103/0971-4065.41280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Henderson S, Brown E, Levy J. Safety and efficacy of percutaneous insertion of peritoneal dialysis catheters under sedation and local anaesthetic. Nephrol Dial Transplant. 2009;24(11):3499–504. doi: 10.1093/ndt/gfp312. [DOI] [PubMed] [Google Scholar]
- 8.Whittaker AA, Albee BJ. Factors influencing patient selection of dialysis treatment modality. ANNA J. 1996;23(4):369–75. discussion 376-7. [PubMed] [Google Scholar]
- 9.Wuerth DB, Finkelstein SH, Schwetz O, Carey H, Kliger AS, Finkelstein FO. Patients’ descriptions of specific factors leading to modality selection of chronic peritoneal dialysis or hemodialysis. Perit Dial Int. 2002;22(2):184–90. [PubMed] [Google Scholar]
- 10.National Kidney Foundation. NKF-DOQI clinical practice guidelines for peritoneal dialysis adequacy. Am J Kidney Dis. 1997;30(Suppl 2):S67–136. doi: 10.1016/s0272-6386(97)70028-3. [DOI] [PubMed] [Google Scholar]
- 11.Bridgewater FH, Mouton WG. Rationale and intended use for the Veress needle: a translation of the original descriptive article. Surg Laparosc Endosc Percutan Tech. 1999;9(4):241–3. [PubMed] [Google Scholar]
- 12.Hadaegh F, Fahimfar N, Khalili D, Sheikholeslami F, Azizi F. New and known type 2 diabetes as coronary heart disease equivalent: results from 7.6 year follow up in a Middle East population. Cardiovasc Diabetol. 2010;9:84. doi: 10.1186/1475-2840-9-84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Varughese S, Sundaram M, Basu G, Tamilarasi V, John GT. Percutaneous continuous ambulatory peritoneal dialysis (CAPD) catheter insertion--a preferred option for developing countries. Trop Doct. 2010;40(2):104–5. doi: 10.1258/td.2010.090370. [DOI] [PubMed] [Google Scholar]
- 14.Ozener C, Bihorac A, Akoglu E. Technical survival of CAPD catheters: comparison between percutaneous and conventional surgical placement techniques. Nephrol Dial Transplant. 2001;16(9):1893–9. doi: 10.1093/ndt/16.9.1893. [DOI] [PubMed] [Google Scholar]
- 15.Mellotte GJ, Ho CA, Morgan SH, Bending MR, Eisinger AJ. Peritoneal dialysis catheters: a comparison between percutaneous and conventional surgical placement techniques. Nephrol Dial Transplant. 1993;8(7):626–30. [PubMed] [Google Scholar]
- 16.Tiong HY, Poh J, Sunderaraj K, Wu YJ, Consigliere DT. Surgical complications of Tenckhoff catheters used in continuous ambulatory peritoneal dialysis. Singapore Med J. 2006;47(8):707–11. [PubMed] [Google Scholar]
- 17.Yang PJ, Lee CY, Yeh CC, Nien HC, Tsai TJ, Tsai MK. Mini-laparotomy implantation of peritoneal dialysis catheters: outcome and rescue. Perit Dial Int. 2010;30(5):513–8. doi: 10.3747/pdi.2009.00033. [DOI] [PubMed] [Google Scholar]


