Abstract
BACKGROUND:
Toxoplasmosis is a worldwide infection. Most studies on toxoplasmosis are in women in child bearing ages. We conducted an epidemiological survey on the population of the Isfahan Province to identify characteristics of the individuals associated with seropositivity.
METHODS:
In a cross sectional study, 599 serum samples were randomly collected for seroepidemiology of Hepatitis A and E, and were also used for titration of IgG anti-toxoplasma gondii antibody by a commercial enzyme-linked immunosorbent assay (ELISA) kit. Data were analyzed using SPSS software15. Chi square and Fisher exact tests were employed to examine antibody status in different age, gender, education and residency groups.
RESULTS:
The overall prevalence was 41.4% (248/599). There was a statistical significant association between seroprevalence with age, education, and gender (p < 0.05) but not with residency state. The peak age for acquisition of the infection in females was 20-29 and in males 20-39 years old.
CONCLUSIONS:
Results of current study showed a moderate prevalence of toxoplasma gondii infection. However higher seroconversion rate in active social and reproductive ages, females and low educated individuals necessitate active preventive programs in these high risk groups.
KEYWORDS: Epidemiology, Toxoplasmosis, Isfahan, Iran, Population based study, Immunoassay
Toxoplasmosis is a worldwide infection, which is primarily acquired through the ingestion of tissue cysts in poorly cooked meat or inadvertent intake of sporulated oocysts excreted in cat feces.1 The infection is mainly asymptomatic in immunocompetent humans, but it can arise to cervical lymphadenopathy, mononucleosis-like syndrome or chorioretinitis in up to 20%.1 Association to behavioral disorders like schizophrenia, mood disorders, personality changes and cognitive impairment has recently been affirmed.2 Consequences of primary infection in pregnant women with normal immunity include abortion, blindness, deafness, mental retardation, microcephalus, hydrocephalus and other neurological diseases in the fetus.3 In immune deficient individuals, primary or reactivated infection can result in encephalitis, pneumonia, myocarditis and disseminated infection.1 Considerable variation in seroprevalence of the infection have been reported in diverse regions and different individuals and various times and are chiefly related to factors that expose the population to the infected cysts.4 Age, sex, ethnicity, sanitary conditions, geographic climate, cat or soil contact, patterns of work and behavior, and location and configuration of the community have been main determinant of these dissimilarities.5 There are many researches about the prevalence of anti-Toxoplasma gondii antibody among Iranian women. Seropositivity have been reported as 48-74.6 in northern areas,6–8 33-44% in northwest,9–13 22-37% in south5,14,15 and 27-54% in central parts of Iran.16–19 Nearly all of these surveys have been performed on females, mainly pregnant women, and based on laboratory, hospital or clinic samples that lack the statistical illustration of the whole population. Therefore, we performed a population based cross-sectional study to determine the prevalence of T. gondii infection in all inhabitants of the Isfahan province and identify the seroprevalence in different age, gender, residence, and educational groups. This provides valuable information about epidemiology of the infection and may be useful for implementing preventive measures in the community.
Methods
Ethical considerations
Before enrolment in the study, detailed information about epidemiological studies was given to the assigned individuals or their parents and written informed consent was obtained.20,21 According to the research design, if the assigned subjects reject the participation in the survey, next neighbor family was offered to partake in the study. The results of performed tests were posted to participants for further follow ups. The study was approved by the regional bioethics committee of the Research Department of Isfahan University of Medical Sciences.
Study area
Isfahan is a large province that covers an area of 107,027 km2 in the central part of Iran. The area has a dry and moderate climate with average temperature of 5.7°C in winter to 27.2 °C in summer and annual rainfall of 122.7 mm. Total population at the time of survey was 4,165,319 inhabitants, 51.3% of them were male and 48.7% were female; 84.9% of them resided in urban area and 15.1% in rural districts.
Study population
For estimation of the seroprevalence of toxoplasma infection in Isfahan province, we tested serum samples which previously reserved in a seroepidemiological study on Hepatitis A and E in 2008.20,21 The above mentioned serums have been collected randomly by multistage cluster sampling method from the whole population of the Isfahan province. Briefly in a random pattern, twenty subjects from each of 41 (nine rural and 32 urban) clusters were randomly selected from the provincial health center census list and were distributed to six age groups of 6-9, 10-19, 20-29, 30-39, 40-49 and >50 years old. After providing written informed consent, 5mL venous blood sample were collected and send to healthcare center in less than 3 hours and centrifuged at 3000 rpm for 15 minutes. Isolated sera were frozen by Alicot method and were stored at -70°C until assays. Additional frozen sera were reserved for further surveys. Simultaneously, a questionnaire including demographic and educational characteristics of the subjects was filled and coded by trained interviewers at the participants’ homes.20,21
Sample size was calculated based on an estimated anti-toxoplasma seroprevalence of 40% in the province with 96% confidence level and 90% power. While 570 samples were required, 600 out of 816 previously collected serum samples20,21 were randomly selected for more accurate estimation in accordance to age distribution of the population in the year of the study.
Laboratory method
After selection of the required samples, the frozen sera were liquefied in room temperature and tested for the presence of IgG anti-T. gondii antibody using a commercial enzyme-linked immunosorbent assay (ELISA) kit (Dia-Pro, Milan, Italy). According to the recommendation of the kit, absorbance levels below 9 was considered as negative, 9-11 assumed as equivocal and above 11 was positive. The samples with equivocal results were retested and were accordingly accepted as negative or positive. If the second test result was equivocal, the sample was excluded from the study.
Statistical analysis
Finally, the collected data were coded and analyzed using the Statistical Package for Social Sciences SPSS for Windows version 15 (SPSS Inc., Chicago IL.). Chi-square and Fisher exact tests were employed to examine antibody status in different age, gender, education and residency groups in the studied population. A P-value of less than 0.05 was considered significant.
Results
Out of 600 serums, which were selected for the study, one sample was excluded due to inadequate volume. Out of 599 samples enrolled, 248 cases were positive, 339 were negative and 12 samples had equivocal results. All samples with equivocal results became negative in repeat of the test.
The overall prevalence of toxoplasma gondii infection in studied population was 41.4 % (248/599). Table 1 shows the distribution of the subjects and seroprevalence of them in various age, gender and residence groups. The distribution of age, gender and residence was similar to that of the whole population in Isfahan province in the year of the study.
Table 1.
Distribution of the enrolled subjects and their T. gondii seroprevalence by age, sex and residence groups in Isfahan province, Iran.
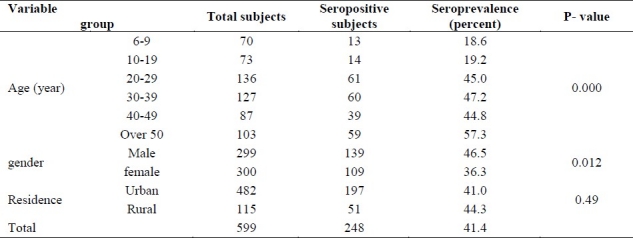
There was a statistically significant association of toxoplasmosis seroprevalence with age and gender (p < 0.05), but the association was not significant with residency groups (p > 0.05).
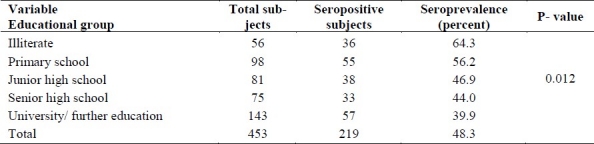
Since the association of the seroprevalence with education could be misleading in ages of less than 20 years old, we assessed this in ages over 20 years old (Table 2). The results show that statistical significance decreases in seropositivity as the level of the education increases (p < 0.05).
Table 2.
Distribution of the enrolled subjects and their T. gondii seroprevalence by educational groups in over 20 years subjects in Isfahan province, Iran.
The seroprevalence of T. gondii infection in different age and gender groups is showed in Figure 1. The rate of positive female subjects rose sharply between the groups aged 10-19 and 20-29 (19.0% and 56.5%, respectively), while in male subjects the seroprevalence was specifically increased slowly between ages of 10-19, 20-29 and 20-39 years (19.4%, 32.8% and 41.0%, respectively) (p < 0.05).
Figure 2 shows the T. gondii seroprevalence in different age and residence groups. It elucidates that the peak age of T. gondii acquisition in urban areas was less than rural districts (20-29 and 30-39 year old, respectively).
Discussion
This study showed a moderate infection (41.4%) with T. gondii protozoa in Isfahan Province, central area of Iran in comparison with other countries and other provinces in Islamic Republic of Iran. Most of the studies on toxoplasmosis have been conducted on subgroups at risk of transmitting infection to offspring mainly pregnant women, women in child-bearing ages or premarriage women.5–10,13–19 Different investigations throughout the world show a wide spectrum of seropositivity. While high prevalences about 75-85% have been reported from Latin America,22 central23,24 and east Europe25 and South-east Asia,26 lower prevalences near 20-30% are found in North America27 and northern Europe.28 In Iran, higher prevalences near 60-75% have been reported in the northern parts of the country.7,8 Lower seropositivity as 20-35% has been reported in the north-west,9,10 central16 and southern5,22 regions. These differences may be related to the climate condition, nutritional behavior and possessing cat, but enrolled subjects, assay and sampling methods and the year of the study may involve in differences between seroprevalence in different areas and same areas in different studies.
Results of the present study showed a significant increasing rate of seropositivity with age (Table 1), which is predictable, because older individuals have more chances for exposure to infectious form of parasite. The most interesting finding of current study was the difference between the peak age for gaining the infection in rural (20-29 years) and urban areas (30-39 years old) of the province (Figure 2). In studies conducted in Venezuela and Croatia, peak age of acquisition of the infection was ages less than 15 years.29–31 In another study in twelve provinces in Iran, most people acquired the infection for 30 years and the seroconversion rate was slightly more in 10-19 years age group, which is compatible with our results.32 The difference in peak age of acquisition in various regions could be due to different climate conditions, dissimilar nutritional and behavioural patterns of life, which expose the population to the infective form of parasite in different ages. The highest acquisition of the infection in active social ages in Iran is alarming which necessitates preventive programs from toxoplasmosis in these high risk age groups.
In studies conducted in pregnant or premarriage women in Cuba, Denmark and Sweden and in northwest and north of Iran no significant statistical difference was established between rural and urban inhabitants.6,8,10,33–35 These are similar with our results (Table 1). However, some researchers found significant differences between children in rural and urban areas.36
Although some researchers did not find significant relationship between infection and gender,32,37 our results elucidate higher rate of seropositivity in female subjects after adolescence. Different sampling method and also diverse lifestyle of women and men in different communities could explain this discrepancy.
The study revealed that the peak age of acquisition of the infection is different for men and women, specifically 20-30 years in females (3.76% in each year) and 20-40 years in males (2.2% in each year). The high rate of seroconversion in the peak of child bearing ages in females and active social ages in both genders is noteworthy.
Like other reports, education has inverse relation with seropositivity of T. gondii infection.5,8,10,11 Increased knowledge through higher education and its consequence on patterns of life and behaviours may lead to a decrease in T. gondii infection, and may have an indirect effect on environmental and cultural factors involved in T. gondii infection.
Conclusion
This study suggests a moderate prevalence of T. gondii infection in the province. The seroconversion was higher in the age group of 20-39 year old, in females and in low educated individuals, which necessitates active preventive programs in these high risk groups to control the burden of active and chronic infection in the community.
Authors’ Contributions
SNM contributed to the study design and prepared the first draft of the manuscript. BA, ZN, MY carried out the design of the study and contributed to collection of data. AB was involved in data analysis and interpretation of the results. All authors have read and approved the content of the manuscript.
Acknowledgments
This study was performed by a grant from Isfahan University of medical sciences with research project number of 287281. The authors are grateful to Mr. Ahmad Reza Pahlevan and Ms Parisa Shoaei for their unsparing assistance in laboratory performance of the research.
Footnotes
Conflict of Interests
Authors have no conflict of interests.
References
- 1.Montoya JG, Boothroyd JC, Kovaks JA. Principles and practice of infectious diseases. In: Mandell GL, Bennett JE, Dolin R, editors. Toxoplasma gondii. Philadelphia: Churchill Livingstone; 2010. pp. 3495–526. [Google Scholar]
- 2.Fekadu A, Shibre T, Cleare AJ. Toxoplasmosis as a cause for behavior disorders- overview of evidence and mechanisms. Folia Parasitol (Praha) 2010;57(2):105–13. doi: 10.14411/fp.2010.013. [DOI] [PubMed] [Google Scholar]
- 3.Boyer KM, Remington JS, McLeod R. Toxoplasmosis. In: Feigin RD, Cherry JD, Demmler GJ, Kaplan Sheldan, editors. Textbook of Pediatric Infectious Diseases. Philadelphia, PA: Saunders; 2004. pp. 2755–61. [Google Scholar]
- 4.Jones JL, Dargelas V, Roberts J, Press C, Remington JS, Montoya JG. Risk factors for Toxoplasma gondii infection in the United States. Clin Infect Dis. 2009;49(6):878–84. doi: 10.1086/605433. [DOI] [PubMed] [Google Scholar]
- 5.Sharifi Mood B, Hashemi Shahri M, Salehi M, Naderi M, Naser poor T. Seroepidemiology of Toxoplasma Infection in the Pregnant Women in Zahedan, Southeast of Iran. J Res Health Sci. 2006;6(1):1–3. [Google Scholar]
- 6.Saeedi M, Veghari GR, Marjani A. Seroepidemiologic evaluation of anti-toxoplasma antibodies among women in North of Iran. Pak J Biol Sci. 2007;10:2359–62. doi: 10.3923/pjbs.2007.2359.2362. [DOI] [PubMed] [Google Scholar]
- 7.Youssefi MR, Sefidgar AA, Mostafazadeh A, Omran SM. Serologic evaluation of toxoplasmosis in matrimonial women in Babol Iran. Pak J Biol Sci. 2007;10(9):1550–2. doi: 10.3923/pjbs.2007.1550.1552. [DOI] [PubMed] [Google Scholar]
- 8.Sharif M, Ajami A, Daryani A, Ziaei H, Khalilian A. Serological survey of toxoplasmosis in women referred to medical health laboratory before marriage northern Iran 2003-2004. Int J Mol Med Adv Sci. 2006;2(2):134–7. [Google Scholar]
- 9.Fallah M, Rabiee S, Matini M, Taherkhani H. Seroepidemiology of toxoplasmosis in primigravida women in Hamadan Islamic Republic of Iran 2004. East Mediterr Health J. 2008;14:163–71. [PubMed] [Google Scholar]
- 10.Hashemi HJ, Saraei M. Seroprevalence of Toxoplasma gondii in unmarried women in Qazvin Islamic Republic of Iran. East Mediterr Health J. 2010;16(1):24–8. [PubMed] [Google Scholar]
- 11.Fallah M, Rabiee S, Matini M, Taherkhani H. Seroepidemiology of Toxoplasma infection in women aged 15–45 years in Hamadan west of Iran. Journal of research in health sciences. 2003;3(1):9–12. [Google Scholar]
- 12.Mansoori Fl. Seroepidemiology of toxoplasmosis in Kermanshah province west of Iran 2002. Behboud. 2004;7(2):12–9. [Google Scholar]
- 13.Abdi J, Shojaee S, Mirzaee A, Keshavarz H. Seroprevalence of Toxoplasmosis in Pregnant Women in Ilam Province Iran. Iranian J Parasitol. 2008;3(2):34–7. [Google Scholar]
- 14.Fouladvand M, Barazesh A, Naeimi B, Zandi K, Tajbakhsh S. Seroprevalence of toxoplasmosis in high school girls in Bushehr city South-west of Iran 2009. Afr J Microbiol Res. 2010;4(11):1117–21. [Google Scholar]
- 15.Foladvand M, Jaafary SM. Seroprevalence of Anti-Toxoplasma antibodies in pregnant women in Bushehr. S Med. 1998;3(2):113–6. [Google Scholar]
- 16.Manouchehri Naeini K, Deris F, Zebardast N. The immunity status of the rural pregnant women in Chaharmahal and Bakhtyari province against Toxoplasma infection 2001–2002. Journal of Shahrekord University of Medical Sciences. 2004;6(3):63–72. [Google Scholar]
- 17.Keshavarz valian H, Nateghpour M, Zibaee M. Seroepidemiology of toxoplasmosis in Karaj Iran in 1998. Iranian J Publ health. 1998;27(3-4):73–8. [Google Scholar]
- 18.Keshavarz valian H, Mamishi S, Daneshvar H. Prevalevce of toxplasmosis in hospitalized patient of Kerman hospitals Iran. J Med Sci Kerman. 2000;7(2):126–39. [Google Scholar]
- 19.Arbabi M, Talari SA. Seroprevalence of Toxoplasma infection in pregnant women in Kashan Iran. Feiz J. 2001;22:28–38. [Google Scholar]
- 20.Ataei B, Nokhodian Z, Javadi AA, Kassaeian N, Shoaei P, Farajzadegan Z, et al. Hepatitis E virus in Isfahan province a population-based study. Int J Infect Dis. 2009;13:67–71. doi: 10.1016/j.ijid.2008.03.030. [DOI] [PubMed] [Google Scholar]
- 21.Ataei B, Javadi AA, Nokhodian Z, Kassaeian N, Shoaei P, Farajzadegan Z, et al. HAV in Isfahan province a population-based study. Trop Gastroenterol. 2008;29(3):160–2. [PubMed] [Google Scholar]
- 22.Spalding SM, Amendoeira MR, Klein CH, Ribeiro LC. Serological screening and toxoplasmosis exposure factors among pregnant women in South of Brazil. Rev Soc Bras Med Trop. 2005;38:173–7. doi: 10.1590/s0037-86822005000200009. [DOI] [PubMed] [Google Scholar]
- 23.Jeannel D, Niel G, Costagliola D, Danis M, Traore BM, Gentilini Epidemiology of toxoplasmosis among pregnant women in the Paris area. Int J Epidemiol. 1989;17:595–602. doi: 10.1093/ije/17.3.595. [DOI] [PubMed] [Google Scholar]
- 24.Ruiz Fons F, Vicente J, Vidal D, Hofle U, Villanua D. Seroprevalence of six reproductive pathogens in European wild boar (Sus scrofa) from Spain The effect on wild boar female reproductive performance. Theriogenology. 2006;65:731–43. doi: 10.1016/j.theriogenology.2005.07.001. [DOI] [PubMed] [Google Scholar]
- 25.Bobic B, Jevremovic I, Marinkovic J, Sibalic D, Djuerkovic-Djakovic O. Risk factors for Toxoplasma infection in a reproductive age female population in the area of Belgrade Yugoslavia. Europ J Epidem. 1998;14:605–10. doi: 10.1023/a:1007461225944. [DOI] [PubMed] [Google Scholar]
- 26.Song KJ, Shin JC, Shin HJ, Nam HW. Seroprevalence of toxoplasmosis in Korean pregnant women of congenital toxoplasmosis. Korean J Parasitol. 2005;43(2):69–71. doi: 10.3347/kjp.2005.43.2.69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Jones JL, Ogunmodede F, Scheftel J, Kirkland E, Lopez A, Schulkin J, et al. Toxoplasmosis related knowledge and practices among pregnant women in the United States. Infect Dis Obstet Gynecol. 2003;11:139–45. doi: 10.1080/10647440300025512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Cunningham FG, Macdonald FC, Gan NF. Williams Obstetrics. 20th ed. Stamford UK: Appleton and Lange; 1997. pp. 1309–10. [Google Scholar]
- 29.Bonilla LC, Chavez YS, Estevez J, Larreal Y, Molero E. Prevalence of human toxoplasmosis in San Carlos Island Venezuela. Interciencia. 2003;28(8):457–62. [Google Scholar]
- 30.Diaz Suárez O, Estevez J. Seroepidemiology of toxoplasmosis in women of child bearing age from a marginal community of maracaibo venezuela. Rev Inst Med trop S Paulo. 2009;51(1):13–7. doi: 10.1590/s0036-46652009000100003. [DOI] [PubMed] [Google Scholar]
- 31.Punda Polic V, Tonkic M, Capkun V. Prevalence of antibodies to Toxoplasma gondii in the female population of the Country of Split Dalmatia Croatia. Europ J Epidem. 2000;16:875–77. doi: 10.1023/a:1007606501923. [DOI] [PubMed] [Google Scholar]
- 32.Assmar M, Amirkhani A, Piazak N, Hovanesian A, Kooloobandi A, Etessami R. Toxoplasmosis in Iran Results of a seroepidemiological study. Bull Soc Pathol Exot. 1997;90(1):19–21. [PubMed] [Google Scholar]
- 33.Martinez SR, Bacallo GR, Amador EA, Affanso LB. Prevalence of toxoplasmosis in pregnant women of the province of La Habana. Rev Inst Med Trop Sao paulo. 1994;36:445–50. [PubMed] [Google Scholar]
- 34.Lebech M, Larson SO, Peterson E. Occurrence of toxoplasmosis in pregnant women in Denmark A study of 5402 pregnant women. Ugeskar Laeger. 1995;157:5242–45. [PubMed] [Google Scholar]
- 35.Ljungstrom I, Gille E, Nokes J, Linder E, Forsgren M. Seroepidemiology of Toxoplasma gondii among pregnant women in different parts of Sweden. Eur J Epidemiol. 1995;11:149–56. doi: 10.1007/BF01719480. [DOI] [PubMed] [Google Scholar]
- 36.Tayler MR, Lennon B, Holland CV, Cafferkey M. Community study of toxoplasma antibodies in urban and rural school children aged 4 to 18 years. Arch Dis Child. 1997;77:406–9. doi: 10.1136/adc.77.5.406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Jones JL, Muccioli C, Belfort RJ, Holland GN, Roberts JM, Silveira C. Recently acquired Toxoplasma gondii infection Brazil. Emerg Infect Dis. 2006;12:582–7. doi: 10.3201/eid1204.051081. [DOI] [PMC free article] [PubMed] [Google Scholar]


