Abstract
BACKGROUND:
Low Back Pain (LBP) and radicular leg pain (RLP) after lumbar disc surgery are great challenges that prevent patients and neurosurgeons in making a surgical decision. By spinal anesthesia, LBP and RLP diminish up to 2 to 3 hours postoperatively. The aim of this study was to determine the effect of impregnated epidural adipose tissue (EAT) with bupivacaine or methylprednisolone acetate on reduction of late postoperative pain after spinal anesthesia.
METHODS:
This study was performed on lumbar disc herniation surgery under spinal anesthesia. Sixty six patients entered our study who were divided into three groups, EAT impregnated with bupivacaine (group 1), methylprednisolone acetate (group2) and normal saline (control group). The LBP and RLP were evaluated during the first 24 hours postoperatively and 14 days later by visual analogue scale (VAS).
RESULTS:
Of 66 patients, 53% were female and 47% male. The average (SE) LBP in the first 6 hours after surgery based on VAS were 1.59 ± 0.90 in group one, 2.36 ± 2.38 in group 2 and 3.09 ± 1.41 in control group but the VAS for RLP in this period were 1.95 ± 1.13, 1.31 ± 1.39 and 2.40 ± 1.09, respectively. The average LBP and RLP did not show any differences after 14 days postoperatively.
CONCLUSIONS:
According to our data bupivacaine was effective on LBP relief and steroid was effective on RLP relief during the first 12 hours after surgery.
KEYWORDS: Intervertebral Disc Degeneration, Bupivacaine, Prednisolone Acetate, Adipose Tissue
Lumbar disc herniation (LDH) is one of the most common surgical procedures in field of neurosurgery and currently, most centers use general anesthesia.1 Low back pain (LBP) and radicular leg pain (RLP) after Lumbar disc surgery have always been the main problems ahead of surgeons and patients.2 Local corticosteroids and anesthetics drugs have been used to reduce the severity of pain.2,3
The use of epidural fat impregnated with these drugs has shown different results and complications,1,4–7 and decision making to use them is sometimes difficult for the neurosurgeons.2,3 Corticosteroids inhibit A2 phospholipase, which play an important role on pain relief after LDH operation.8 Bupivacaine, as a local anesthetic drug, is highly effective on pain relief few hours after operation.8–10 When used in liquid form, both steroids and bupivacaine fate away very soon but if impregnated in fat tissue, they will be effectively and slowly absorbed from adipose tissue.3,8,10,11 So far, all studies using steroids and topical anesthetics to relieve pain have been done in patients with general anesthesia. Since the pain relief of intervention of drugs wash down in 2 to 3 hours,12,13 we decided to use this method in our patients under spinal anesthesia to increase the duration of analgesic effects and comfortably of the patients.
Methods
This study was a double blind randomized clinical trial on patients with single level LDH admitted and operated at Kashani hospital in a period of six months, March 2009 to September 2009 and supported by research council of Isfahan University of Medical Sciences by registry number 287264. All 66 patients were randomly divided into three groups according to their sequences of operating room adminestration. Autologous adipose tissue impregnated either with bupivocaine (group one), methylprednisolone acetate (group two) or normal saline (group three), (Figure 1).
Figure 1.
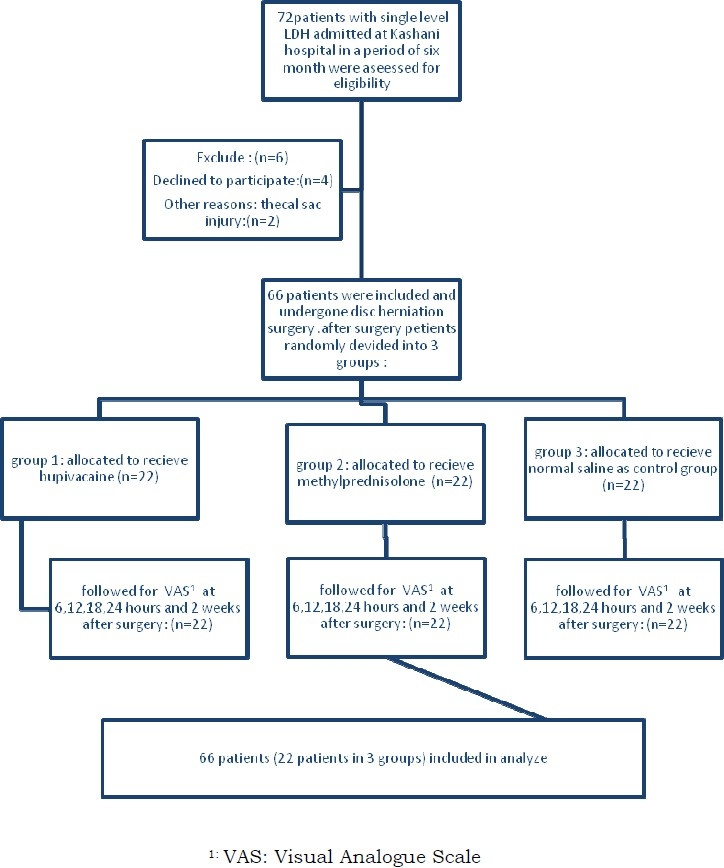
Diagram of research progress
For induction of spinal anesthesia before surgery, 3 cc Marcaine 0.5% was injected intrathecally.1–5 At the time of lumbar puncture and drug injection, we asked the anesthesiologist not to use the same level at which LDH have been occurred. After the full appearance of analgesic effects of drugs and when the patients did not have any pain below the level of surgical intervention, they were transferred to prone position on operating table. While the patients were entirely conscious, a laminectomy was performed. All of the patients were operated by one neurosurgeon with the same technique that was completely aware of the content of harvest adipose tissue but the assistant of neurosurgery who was responsible of follow up and analysis of the data was completely blind to the contents of fat graft. At the end of surgery, one of the assistants who was completely blind to the content of adipose tissue, placed a small autologous fat (1 × 1 × 1 cm) harvested from subcutaneous tissue and impregnated with either bupivacaine (1 cc, 0.5%), steroid (40 mg methylprednisolone acetate) or normal saline (1 cc) at the interested site of operation. The grafts were implanted at the epidural space in contact with thecal sac.
At the end of surgery the patients were transferred to the ward and were evaluated in terms of pain intensity based on VAS by assistant of neurosurgery who had no information about which drug has been used for each patient. VAS scores were evaluated 3 times every 6 hours at the first day before discharge and 14 days later when the patients came back for follow-up.
All of the patients with thecal sac injury at the time of surgery were excluded from the study because this may increase the risk of pain, CSF leakages, infection, and washout phenomenon of intrathecal injection of anesthetic drug. Also, those patients that were not cooperative and/or willing to take part in our study were excluded.
The data were analyzed by repeated measure ANOVA (SPSS version 18) to compare relative frequency of VAS. For qualitative variables chi-square test was used.
Results
Total number of patients assessed in this study was 72 of whom 6 were excluded as they did not accept to participate in study (n = 4) or had thecal sac injury (n = 2) (Diagram 1). Of all 66 patients, the mean age was 45.4 ± 10.33 years and 35 cases (53%) were female. No statistically significant difference in mean age and sex distribution of patients were existed among three groups (p = 0.4 and 0.6, respectively). Other data are shown in Tables 1–3.
Table 1.
Patients frequency distribution of age, sex and urinary retention in three groups according to application of epidural adipose tissue
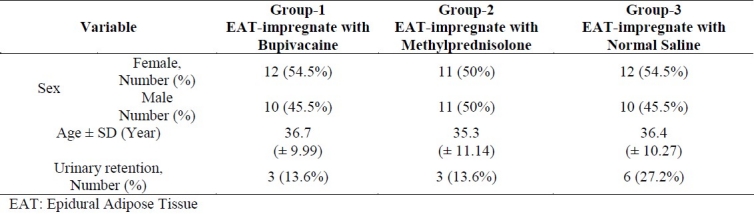
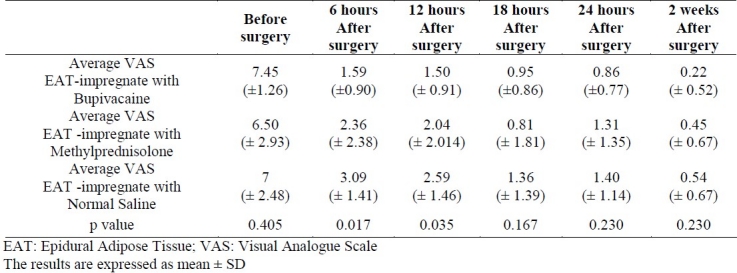
Table 3.
The average visual analogue scale (VAS) of radicular leg pain (RLP) after operation in Bupivacaine, Methylprednisolone acetate and Normal saline groups
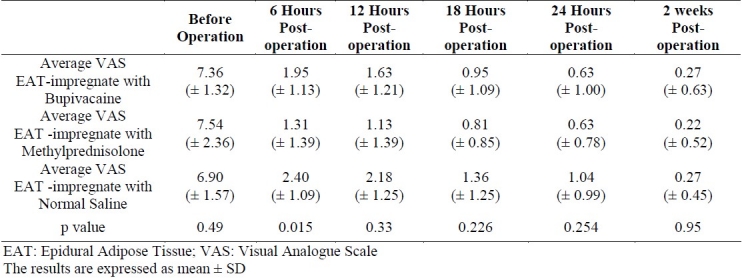
Table 2.
The average of visual analogue scale (VAS) of low back pain (LBP) in patients with lumbar disc herniation in Bupivacaine, Methylprednisolone acetate and Normal saline groups
All patients were discharged from hospital 24 hours after their operations. No local or systemic infections were detected during 14 days follow-up. Urinary retention after surgery occurred in 12 patients, 3 cases in groups one and two and 6 cases in normal saline group, all relieved by bladder catheter.
Discussion
LBP and RLP after lumbar disc surgery have been always the main problems ahead of neurosurgeons2 and for patients accounted for a large quantity of lost productivity in the workforce. Although surgical treatment is technically simple and professionally gratifying for the neurosurgeons, still many patients who need surgical intervention have intense irrational fear from post-operation pain. As a consequence, LDH can generate distrust of neurosurgeons on the part of patients and vice versa.
To overcome postoperation pain, different techniques have been presented.2,3,9,14–16 Local corticosteroids and analgesic drugs have been used to ameliorate the severity of pain2,3 with different results and complications.2,9 When these drugs are used with fat, it seems that the duration of their efficacy could be longer8 although some data have shown that EAT may induce some complications.2,4–7,9,17
Most of the neurosurgeons prefer general anesthesia instead of spinal anesthesia for LDH surgery.12,13 Others have their excellent experiences on lumbar anesthesia.12,13 Meanwhile, the duration of painless interval is approximately 2 to 3 hours, then most of the patients suffer from severe LBP and RLP.12
After spinal anesthesia, LBP and RLP begin in about 2 to 3 hours post-operatively when anesthetic effect of Marcaine fate away.12 During general anesthesia, the use of impregnated fat with bupivacaine and steroid could diminish pain as a consequence of manipulation of sensitive structures.3 In our study, we decided to apply bupivacaine and steroid to decrease postoperative pain after spinal anesthesia. According to our experiences at 6 and 12 hours postoperatively, the average VAS for LBP was 1.59 (± 0.90) and 1.50 (± 91), respectively for bupivacaine and 2.36 ± 2.38 to 2.04 ± 2.01, respectively for methylprednisolone. The 6 and 12 hours postoperative average VAS for RLP were 1.95 ± 1.13 and 1.63 ± 1.21, respectively for bupivacaine and 1.31 ± 1.39 and 1.13 ± 1.39, respectively for methylprednisolone; so EAT with bupivacaine was effective on LBP and methylprednisolone was more effective on RLP, but after 24 hours of operation, none of them were effective on pain relief.
Two weeks after operation the statistic results were not different among three groups; the average VAS for LBP was 0.22 ± 0.52 for bupivacaine and 0.45 ± 0.67 for methylprednisolone. On the other hand, these findings for RLP were 0.27 (± 0.63) for bupivacaine and 0.22 ± 0.52 for methylprednisolone. Fortunately, after this period the average VAS of all three groups was between 0.22 to 0.54 for LBP and 0.22 to 0.27 for RLP, so that most of the patients even didn’t need any more pain killer medication. The main point that was absolutely different in our study in relation to other studies was that we tried to control the pain post-operatively by spinal anesthesia versus general anesthesia, so the whole painless period could be increased up to a few hours which is not possible in general anesthesia.
On the other hand, the mean period that most patients suffer from severe pain after operation is during the first 24 hours of intervention, therefore the application of the combination of methylprednisolone and bupivacaine could diminish the severity of pain.
Consequently, by combination of spinal anesthesia and EAT impregnated with either bupivacaine and/or methylprednisolone, it is possible to diminish the post-operation pain free interval.
Conclusion
After spinal anesthesia, the painless period is approximately 2 to 3 hours and then LBP and RLP appear. The use of EAT may have a protective effect on late adhesive irritating scar tissue and when impregnated with bupivacaine or methylprednisolone acetate could increase the duration of painless interval. According to our data bupivacaine, was effective on LBP relief and steroid was effective on RLP relief during the first 12 hours after surgery.
Authors’ Contributions
SA and ARR participated in the design and conduct of the study, drafted and edited the manuscript; MS, SM, NE, GB, PR, and HT participated in the design and conduct of the study; AH, and MT helped to draft and edit the manuscript. All authors read and approved the final manuscript.
Acknowledgment
We are pleased to thank the research council of Isfahan University of Medical Sciences for acceptance of the primary proposal and all necessary revisions needed.
Footnotes
Conflict of Interests
Authors have no conflict of interests.
References
- 1.Jensen TT, Asmussen KH, Rose-Hansen EB, Lauritsen BU, Manniche C, Vinterberg H, et al. Lumbar disk prolapse surgery with or without free fat transplantation.A prospective triple-blind randomized study. Ugeskr Laeger. 1997;159(14):2091–5. [In Danish] [PubMed] [Google Scholar]
- 2.Park CH, Lee SH, Kim BI. Comparison of the effectiveness of lumbar transforaminal epidural injection with particulate and nonparticulate corticosteroids in lumbar radiating pain. Pain Med. 2010;11(11):1654–8. doi: 10.1111/j.1526-4637.2010.00941.x. [DOI] [PubMed] [Google Scholar]
- 3.Jirarattanaphochai K, Jung S, Thienthong S, Krisanaprakornkit W, Sumananont C. Peridural methylprednisolone and wound infiltration with bupivacaine for postoperative pain control after posterior lumbar spine surgery: a randomized double-blinded placebo-controlled trial. Spine (Phila Pa 1976) 2007;32(6):609–16. doi: 10.1097/01.brs.0000257541.91728.a1. discussion 617. [DOI] [PubMed] [Google Scholar]
- 4.Murata Y, Kato Y, Miyamoto K, Takahashi K. Clinical study of low back pain and radicular pain pathways by using l2 spinal nerve root infiltration: a randomized, controlled, clinical trial. Spine (Phila Pa 1976) 2009;34(19):2008–13. doi: 10.1097/BRS.0b013e3181b1fb96. [DOI] [PubMed] [Google Scholar]
- 5.Slipman CW, Chow DW. Therapeutic spinal corticosteroid injections for the management of radiculopathies. Phys Med Rehabil Clin N Am. 2002;13(3):697–711. doi: 10.1016/s1047-9651(02)00004-9. [DOI] [PubMed] [Google Scholar]
- 6.Chuang TY, Chen WJ, Chen LH, Niu CC, Shih CH. Acute postoperative aggravation of radiculopathy as a complication of free fat transplantation in lumbar disc surgery: case report. Changgeng Yi Xue Za Zhi. 1999;22(3):498–502. [PubMed] [Google Scholar]
- 7.Prusick VR, Lint DS, Bruder WJ. Cauda equina syndrome as a complication of free epidural fat-grafting.A report of two cases and a review of the literature. J Bone Joint Surg Am. 1988;70(8):1256–8. [PubMed] [Google Scholar]
- 8.Jensen TT, Asmussen K, Berg-Hansen EM, Lauritsen B, Manniche C, Vinterberg H, et al. First-time operation for lumbar disc herniation with or without free fat transplantation.Prospective triple-blind randomized study with reference to clinical factors and enhanced computed tomographic scan 1 year after operation. Spine (Phila Pa 1976) 1996;21(9):1072–6. doi: 10.1097/00007632-199605010-00016. [DOI] [PubMed] [Google Scholar]
- 9.Kalkan E, Torun F, Tavlan A, Cengiz SL, Kaya B. The effect of meperidine-impregnated autogenous free fat grafts on postoperative pain management in lumbar disc surgery. J Spinal Disord Tech. 2008;21(2):92–5. doi: 10.1097/BSD.0b013e31805f6d54. [DOI] [PubMed] [Google Scholar]
- 10.Kanamori M, Kawaguchi Y, Ohmori K, Kimura T, Tsuji H, Matsui H. The fate of autogenous free-fat grafts after posterior lumbar surgery: part 2.Magnetic resonance imaging and histologic studies in repeated surgery cases. Spine (Phila Pa 1976) 2001;26(20):2264–70. doi: 10.1097/00007632-200110150-00019. [DOI] [PubMed] [Google Scholar]
- 11.Kanamori M, Kawaguchi Y, Ohmori K, Kimura T, Md HT, Matsui H. The fate of autogenous free-fat grafts after posterior lumbar surgery: part 1.A postoperative serial magnetic resonance imaging study. Spine (Phila Pa 1976) 2001;26(20):2258–63. doi: 10.1097/00007632-200110150-00018. [DOI] [PubMed] [Google Scholar]
- 12.McLain RF, Kalfas I, Bell GR, Tetzlaff JE, Yoon HJ, Rana M. Comparison of spinal and general anesthesia in lumbar laminectomy surgery: a case-controlled analysis of 400 patients. J Neurosurg Spine. 2005;2(1):17–22. doi: 10.3171/spi.2005.2.1.0017. [DOI] [PubMed] [Google Scholar]
- 13.Demirel CB, Kalayci M, Ozkocak I, Altunkaya H, Ozer Y, Acikgoz B. A prospective randomized study comparing perioperative outcome variables after epidural or general anesthesia for lumbar disc surgery. J Neurosurg Anesthesiol. 2003;15(3):185–92. doi: 10.1097/00008506-200307000-00005. [DOI] [PubMed] [Google Scholar]
- 14.Gorgulu A, Simsek O, Cobanoglu S, Imer M, Parsak T. The effect of epidural free fat graft on the outcome of lumbar disc surgery. Neurosurgical Review. 2004;27(3):181–4. doi: 10.1007/s10143-003-0310-9. [DOI] [PubMed] [Google Scholar]
- 15.Bernsmann K, Kramer J, Ziozios I, Wehmeier J, Wiese M. Lumbar micro disc surgery with and without autologous fat graft.A prospective randomized trial evaluated with reference to clinical and social factors. Arch Orthop Trauma Surg. 2001;121(8):476–80. doi: 10.1007/s004020100277. [DOI] [PubMed] [Google Scholar]
- 16.Mackay MA, Fischgrund JS, Herkowitz HN, Kurz LT, Hecht B, Schwartz M. The effect of interposition membrane on the outcome of lumbar laminectomy and discectomy. Spine. 1995;20(16):1793–6. doi: 10.1097/00007632-199508150-00008. [DOI] [PubMed] [Google Scholar]
- 17.Cobanoğlu S, Imer M, Ozylmaz F, Memiş M. Complication of epidural fat graft in lumbar spine disc surgery: case report. Surg Neurol. 1995;44(5):479–81. doi: 10.1016/0090-3019(95)00222-7. discussion 481-2. [DOI] [PubMed] [Google Scholar]
- 18.Abrishamkar S, Aminmansour B, Arti H. The effectiveness of computed tomography scans versus magnetic resonance imaging for decision making in patients with low back pain and radicular leg pain. Journal of Research in Medical Sciences. 2006;11(6):351–4. [Google Scholar]


