Abstract
BACKGROUND:
Diabetic nephropathy is the major cause for chronic renal failure (CRF) and proteinuria is an independent risk factor for end stage renal disease. Hence, early identification and quantification of proteinuria is of prime importance in the diagnosis and management.
METHODS:
This study was conducted amongst 42 diabetic subjects from HSK hospital, Bagalkot. Twenty four-hour urine protein and random urine protein to creatinine ratio (P:C) was determined. Pearson's correlation, sensitivity, specificity, positive and negative predictive values were determined using 24-hour urinary protein as a gold standard for spot urine P:C ratio. ROC curve and area under curve was also determined using SPSS (11.5) software. All the results were expressed in mean±SD.
RESULTS:
Forty two diabetes mellitus patients participated in this study. The average of 24 hour urinary protein was 1.6 ± 1.7 gm/day. The spot urine P:C ratio was 1.27 ± 1.55. There was a positive correlation between 24 hours urinary protein and spot urine P:C ratio (r = 0.925, p < 0.0001). The area under the ROC curve for urine P:C ratio at various cutoff was 0.947 (95% confidence interval: 0.831-0.992, p < 0.0001). The sensitivity and specificity was 80.65% and 100% respectively at P:C ratio cutoff of 0.3.
CONCLUSIONS:
The random urine P:C ratio predicts the amount of 24-hour urinary protein excretion with high accuracy. Hence it can be used as a faster diagnostic substitute for 24-hour urinary protein estimation.
KEYWORDS: Type 2 Diabetes Mellitus, 24-Hour Urine, Urine Protein to Creatinine Ratio
Proteinuria is an independent risk factor for renal diseases and a predictor of end stage renal disease (ESRD).1 Accurate identification and quantification of proteinuria is of prime importance in the diagnosis and management of chronic renal disease. An increased proteinuria is associated with an increased risk of progressive renal failure, cardiovascular diseases and death, and is used as both diagnostic and prognostic values in detection and confirmation of renal diseases, or response to therapy.2
The increase in incidence of type 2 diabetes mellitus worldwide is mainly attributable to the interaction between risk factors like genetic predisposition, behavioral and environmental factors.3 Diabetic nephropathy accounts for about 20% of cases of chronic renal failure and is the single most common cause of ESRD in many countries.4 It is generally said that diabetic nephropathy is viewed as a descending path from normoalbuminuria to ESRD which is marked by intermediate stage microalbu-minuria and overt proteinuria.5
For quantification of proteinuria, timed urine collections (usually performed over 24 hours) were considered as gold standard, but have major limitations like time consumption and error in sample collection. Estimation of total protein in spot urine sample, avoids the 24-hour urine collection, but is largely influenced by the body hydration. This variation can be eliminated by factoring the spot urine total protein concentration by urine creatinine concentration, i.e. the urine protein to creatinine ratio (P:C ratio).6 Random urine sampling for P:C ratio would be more acceptable and less time consuming.7,8 The P:C ratio takes into account the fact that creatinine excretion remains fairly constant in presence of a stable GFR. The protein excretion would also be fairly stable. Therefore, the ratio of the two in a single voided sample would reflect the cumulative protein excretion over the day, as the two stable rates would cancel out the time factor.9 Measurement of total protein to creatinine ratio (TPCR) on random (spot) urine sample correlates well with 24 hours total protein excretion.2
In this context, the present study was undertaken to evaluate the diagnostic value of P:C ratio in spot voided urine sample for detection of proteinuria as compared to those of 24 hours sample in patients with type 2 diabetes mellitus, and also to determine the optimal cut-off value of P:C ratio with best sensitivity and specificity for the prediction of significant proteinuria.
Methods
The study was conducted in diabetic subjects from Hanagal Shri Kumareshwara hospital, Bagalkot. Informed consent was obtained. The study was approved by S.Nijalingappa Medical College ethical committee (Ref No: SNMC/09-10/602). The study was conducted from Jun 2009 to February 2010. The diabetes mellitus type 2 patients attending outpatient department and diagnosed based on American diabetes association, National diabetes data and World health organization diagnostic criteria, were selected for the study.10 Detailed history and clinical examination was carried out by physician. Patients with urinary tract infection, chronic renal failure, glomerular nephritis due to other systemic conditions and hypertensives were excluded from the study. Pregnant women were also excluded from the study. A total number of 74 patients were selected for the study but 24 patients did not turn-up and 50 subjects participated in the present study. Eight participants were excluded from the study, because of improper collection of 24- hour urine, and finally 42 type 2 diabetic patients were studied. Twenty-four hour urine sample was collected by instructing subjects to begin collection immediately after completion of first voiding in morning and to collect all urine into same container having 5mL of 10% thymol in iso-propanol as a preservative for 24 hours, including final void at completion of 24 hour period.11 This was thoroughly mixed and a sample of 2mL was taken for evaluation of proteins. Total volume was noted and calculation was done for 24 hours. The proteinuria ≥ 300mg/dl in 24-hour urine sample was considered as significant proteinuria.6 A random urine sample of 5mL was collected on next day any time just before the analysis and after completion of 24 hour collection. The fasting blood glucose, glycated hemoglobin, urine creatinine, and urine protein were estimated by kit method using semiautomatic analyzer Statfax 3300. The fasting blood glucose and glycated hemoglobin were estimated to know the diabetic status of the patient. P:C ratio was calculated by dividing the urinary protein concentration by urinary creatinine concentration.
Statistical analysis: Statistical package for social science (SPSS for window version; SPSS, 11.5 Inc, Chicago IL) software was used for statistical analysis. Pearson's correlation coefficient was used to show the correlation between the spot urine P:C ratio and 24 hours urine total protein. Sensitivity, specificity, predictive values of random urine P:C ratio at various cut-off values were evaluated using 24 hours urine total protein level as the gold standard. A receiver operator characteristics (ROC) curve was determined. All the results were expressed as mean±SD.
Results
The characteristics of subjects are shown in Table 1. Forty two diabetes mellitus patients were involved in this study, among which 30 were males and 12 were females. The average age was 52.92 ± 12.8 years and the duration of diabetes mellitus was 6.22 ± 4.16 years. The fasting blood glucose was 183.14 ± 75.14 mg/dl and the average glycosylated hemoglobin was 8.25 ± 1.33 percent.
Table 1.
Characteristics of type 2 diabetes mellitus subjects.
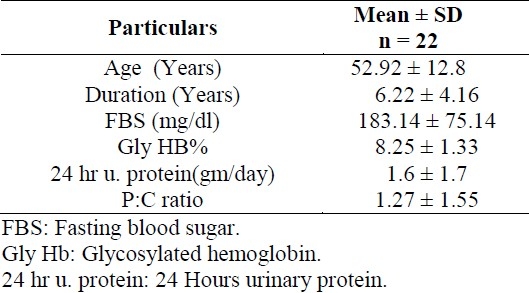
P:C ratio: Urine protein creatinine ratio
The mean 24-hour urinary protein was 1.6 ± 1.7 gm/day. The mean of spot urine P:C ratio was 1.27 ± 1.55. There was a positive correlation between 24-hour urinary protein and spot urine P:C ratio (r = 0.925) (Figure 1).
Figure 1.
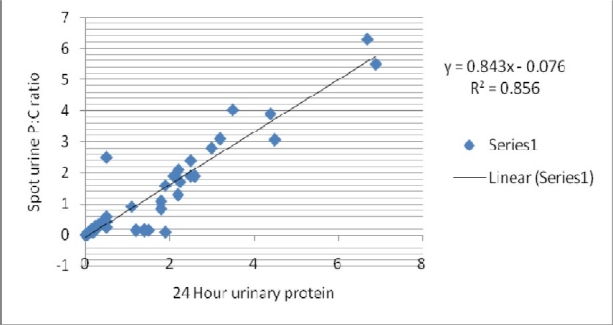
Correlation between 24-hour urinary protein and spot urine P:C ratio in type 2 diabetes mellitus subjects.
P:C ratio: Spot urinary protein to creatinine ratio. 24 hours urinary protein values are in gm/day. R2= 0.856: coefficient of determination r = Square root of R2= 0.925 pearson's correlation co efficient (showing positive correlation).
The area under the ROC curve for random urine P:C ratio at various cut-off was 0.947 (95% confidence interval, 0.831-0.992 ; p < 0.0001) as shown in figure 2. Sensitivity and specificity of P:C ratio to detect proteinuria at various cut-off values is shown in table 2. A sensitivity of 80.65% and specificity of 100% were achieved to detect proteinuria at the P:C ratio greater than 0.3.
Figure 2.
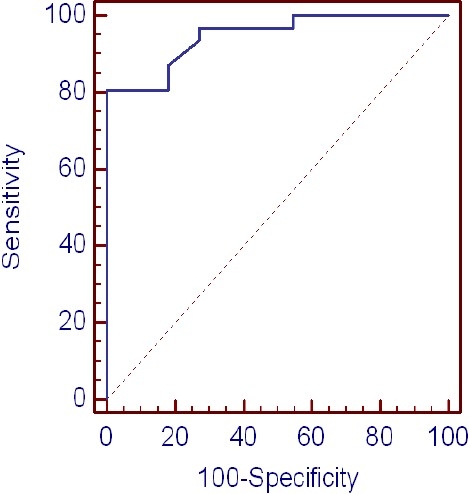
ROC curve at various cutoff points for the spot random urinary protein creatinine ratio.
Table 2.
Criterion values and coordinates of the ROC curve.
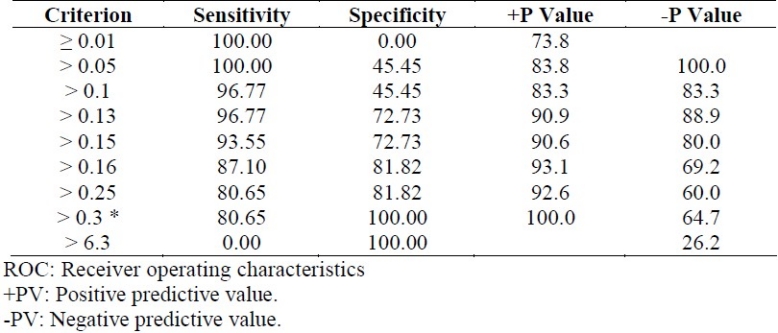
At cut-off value of greater than 0.05, sensitivity was 100% but specificity reduced to 45.45%, whereas for more than 6.3, specificity was 100% but sensitivity fell to 0.00%.
Discussion
The present study showed a positive correlation between the random urine P:C ratio and 24-hour urinary protein in type 2 diabetes mellitus patients. Yadav BK et al have also shown the similar results.5 However, the urinary protein excretion over a 24-hour period is the gold standard method. Most of the times, it appears impracticable, especially in outpatient department and female patients to collect 24-hour urine. The high degree of variation in the urinary protein concentration during the day can be attributed to variation in intake of water, rate of diuresis, exercise, recumbency and diet.1 Proteinuria is a cardinal manifestation of glomerular or tubular disease that requires meticulously timed (usually 24 hours) urine collection for its evaluation. Complete collection can be assured by indwelling Foley's catheter or extreme awareness of the completeness of urine collection.
The plasma levels of endothelin -1, an important vasoconstrictor, progressively increases with the severity of diabetic nephropathy. This early defect in autoregulation of renal perfusion makes it easier for albumin to leak from capillaries of renal glomerulus. Albumin activates various inflammatory pathways. In addition, the mechanical stress resulting from renal hyperperfusion induces the release of cytokines, growth factors, cholesterol and triglycerides that induce the accumulation of proteins from extracellular matrix leading to glomerulosclerosis.12
The increased expression of vascular endothelial growth factors due to hyperglycemia in podocytes causes increased vascular permeability. The non enzymatic glycation of proteins is also influenced by hyperglycemia, which bind to collagen and proteins that constitute glomerular basement membrane and make glomerular barrier more permeable to proteins.12 The independent risk factor such as hypertension, together with intrinsic renal toxicity caused due to proteins filtered through glomerular vessels, may contribute to the progression of renal damage.13
Ruggenenti P et al13 showed that P:C ratio predicted the rate of decline even more accurately than 24-hour urinary protein excretion, which suggests that the random urine P:C ratio is more accurate index of kidney traffic of plasma proteins compared to 24-hour urinary total proteins. The spot morning urine P:C ratio is independent of errors and it is also very minimally affected by wide variations in urinary protein excretion rate which is associated with changes in posture, physical activity and hemodynamic factors.13
Significance of P:C ratio was shown in various conditions like type 1 diabetes mellitus14, non diabetic renal failure15, pregnancy16, pree-clampsia17,18, renal transplantation19, lupus nephritis20 etc. Seyed-Ali and Navin Jaipaul21 found that the random urine P:C ratio is a reliable and practical way of estimating and following proteinuria, but its precision and accuracy may be affected by the level of patient physical activity. Jiunn-Min Wang et al22 concluded that P:C ratio or albumin to Creatinine ratio, which was obtained by dipstick, can be used to monitor the potential risk of renal diseases in outpatients, hypertensive and diabetic patients. Ayman M. Wohbeh et al23 reported that P:C ratio in spot urine specimens is a more precise, accurate, convenient and reliable method to evaluate proteinuria. However, only when protein is at reasonably low levels, the P:C ratio is likely to be within acceptable limits.
In the present study, the ROC curve analysis showed an area under the curve of 0.947 indicating that the urinary P:C ratio is sufficiently acceptable to predict significant proteinuria. At the optimal cut-off point of 0.3, the sensitivity was 80.65 % and specificity was 100 %. Hence, the random P:C ratio is a good predictor of significant proteinuria in diabetic nephropathy. In concordance with our findings, B K Yadav et al5 found that area under the ROC curve was 0.88. Price et al1 reviewed 16 studies and the area under the curve was in the range of 0.70 to 0.90, suggesting that the P:C ratio can predict the amount of protein excreted in the urine. Hence, it is important for each laboratory to determine the cut-off value of P:C ratio which has maximum sensitivity and specificity to be used in those settings.
The limitations of the present study were the low sample size, and the difficulties in collection of 24 hours urine sample in the female patients. Further study is required with large sample size to emphasize the hypothesis.
In conclusion, the present study suggests that a random urine P:C ratio predicts the amount of 24-hour urine protein excretion with high accuracy. This test could be the reasonable alternative to the 24-hour urine sample collection for the detection of significant proteinuria in type 2 diabetes mellitus patients.
Authors’ Contributions
SVK and GSK carried out the design and coordinated the study, participated in most of the experiments and prepared the manuscript. SBB and SVK provide assistance in the design of the study, coordinated and carried out all the experiments and participated in manuscript preparation. MR and RR provided assistance for all experiments. All authors have read and approved the content of the manuscript.
Footnotes
Conflict of Interests
Authors have no conflict of interests.
References
- 1.Price CP, Newall RG, Boyd JC. Use of protein:creatinine ratio measurements on random urine samples for prediction of significant proteinuria: a systematic review. Clin Chem. 2005;51(9):1577–86. doi: 10.1373/clinchem.2005.049742. [DOI] [PubMed] [Google Scholar]
- 2.Methven S, MacGregor MS, Traynor JP, O’Reilly DJ, Deighan CI. Assessing proteinuria in chronic kidney disease: protein-creatinine ratio versus albumin–creatinine ratio. Nephrol Dial Transplant. 2010;25(9):2991–6. doi: 10.1093/ndt/gfq140. [DOI] [PubMed] [Google Scholar]
- 3.Tuomilehto J, Lindstrom J, Eriksson JG, Valle TT, Hamalainen H, Ilanne-Parikka P, et al. Prevention of type 2 diabetes mellitus by changes in lifestyle among subjects with impaired glucose tolerance. N Engl J Med. 2001;344(18):1343–50. doi: 10.1056/NEJM200105033441801. [DOI] [PubMed] [Google Scholar]
- 4.Refaat HA, Mady GE, Abdel Ghany MM, Abou Seif KH, El Hadidi ES, Elshahawy Y. Correlation between tumor necrosis factor alpha and proteinuria in type -2 diabetic patients. Arab Journal of Nephrology and Transplantation. 2010;3(1):33–8. [Google Scholar]
- 5.Yadav BK, Adhikari S, Gyawali P, Shrestha R, Poudel B, Khanal M. Use of protein: creatinine ratio in a random spot urine sample for predicting significant proteinuria in diabetes mellitus. Nepal Med Coll J. 2010;12(2):100–5. [PubMed] [Google Scholar]
- 6.Stevens LA, Levey AS. Current status and future perspectives for CKD testing. American Journal of Kidney Diseases. 2009;53(3):S17–S26. doi: 10.1053/j.ajkd.2008.07.047. [DOI] [PubMed] [Google Scholar]
- 7.Cirillo M. Evaluation of glomerular filtration rate and of albuminuria/proteinuria. J Nephrol. 2010;23(2):125–32. [PubMed] [Google Scholar]
- 8.Al RA, Baykal C, Karacay O, Geyik PO, Altun S, Dolen I. Random urine protein-creatinine ratio to predict proteinuria in new-onset mild hypertension in late pregnancy. Obstet Gynecol. 2004;104(2):367–71. doi: 10.1097/01.AOG.0000134788.01016.2a. [DOI] [PubMed] [Google Scholar]
- 9.Agarwal I, Kirubakaran CH. Quantitation of proteinuria by spot urine sampling. Indian Journal of Clinical Biochemistry. 2004;19(2):45–7. doi: 10.1007/BF02894256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Powers AC. Diabetes mellitus. In: Fauci AS, Braunwald E, Kasper DL, Hauser SL, editors. Harrison's Principles of Internal Medicine. 17th ed. Philadelphia: McGraw-Hill Professional; 2008. [Google Scholar]
- 11.Varley H, Gowenlock AH. Collection of specimens and some general techniques. In: Varley H, editor. Practical clinical biochemistry: general topics and commoner tests. 5th ed. London: Butterworth-Heinemann Ltd; 1980. pp. 379–80. [Google Scholar]
- 12.Zelmanovitz TH, Gerchman F, Balthazar A, Thomazelli F, Matos J, Canani LH. Diabetic nephropathy. Diabetology & Metabolic Syndrome. 2009;1:10. doi: 10.1186/1758-5996-1-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ruggenenti P, Gaspari F, Perna A, Remuzzi G. Cross sectional longitudinal study of spot morning urine protein:creatinine ratio, 24 hour urine protein excretion rate, glomerular filtration rate, and end stage renal failure in chronic renal disease in patients without diabetes. BMJ. 1998;316(7130):504–9. doi: 10.1136/bmj.316.7130.504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rodby RA, Rohde RD, Sharon Z, Pohl MA, Bain RP, Lewis EJ The Collaborative Study Group. The urine protein to creatinine ratio as a predictor of 24-hour urine protein excretion in type 1 diabetic patients with nephropathy. Am J Kidney Dis. 1995;26(6):904–9. doi: 10.1016/0272-6386(95)90054-3. [DOI] [PubMed] [Google Scholar]
- 15.Saxena SK, Dwivedi RN, Alam SM, Chandra R, Singh SN, Kumar A, et al. Prognostic predictors in non-diabetic CRF with special reference to proteinuria. Journal, Indian Academy of Clinical Medicine. 2001;2(4):276–80. [Google Scholar]
- 16.Rodriguez-Thompson D, Lieberman ES. Use of a random urinary protein-to-creatinine ratio for the diagnosis of significant proteinuria during pregnancy. Am J Obstet Gynecol. 2001;185(4):808–11. doi: 10.1067/mob.2001.117349. [DOI] [PubMed] [Google Scholar]
- 17.Taherian AA, Dehbashi S, Baghban M. The Relationship between random urinary protein-to-creatinine ratio and 24-hours urine protein in diagnosis of proteinuria in mild preeclampsia. Journal of Research in Medical Sciences. 2006;11(1):6–12. [Google Scholar]
- 18.Shahbazian N, Hosseini-Asl F. A comparison of spot urine protein-creatinine ratio with 24-hour urine protein excretion in women with preeclampsia. Iran J Kidney Dis. 2008;2(3):127–31. [PubMed] [Google Scholar]
- 19.Torng S, Rigatto C, Rush DN, Nickerson P, Jeffery JR. The urine protein to creatinine ratio (P/C) as a predictor of 24-hour urine protein excretion in renal transplant patients. Transplantation. 2001;72(8):1453–6. doi: 10.1097/00007890-200110270-00021. [DOI] [PubMed] [Google Scholar]
- 20.Leung YY, Szeto CC, Tam LS, Lam CW, Li EK, Wong KC, et al. Urine protein-to-creatinine ratio in an untimed urine collection is a reliable measure of proteinuria in lupus nephritis. Rheumatology (Oxford) 2007;46(4):649–52. doi: 10.1093/rheumatology/kel360. [DOI] [PubMed] [Google Scholar]
- 21.Sadjadi SA, Jaipaul N. Correlation of random urine protein creatinine (P-C) ratio with 24-hour urine protein and P-C ratio, based on physical activity: a pilot study. Therapeutics and Clinical Risk Management. 2010;6(351):7. doi: 10.2147/tcrm.s12298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Min Wang J, Yu-Lin C, An Tsai F, Yi Chen J, Chen Koa Y. Test dipstick for determination of urinary protein, creatinine and protein / creatinine ratio. J Biomed Lab Sci. 2009;21(1):23–8. [Google Scholar]
- 23.Wahbeh AM, Ewais MH, Elsharif ME. Comparison of 24-hour urinary protein and protein-to-creatinine ratio in the assessment of proteinuria. Saudi J Kidney Dis Transpl. 2009;20(3):443–7. [PubMed] [Google Scholar]


