Abstract
BACKGROUND:
Dialysis patients experience psychosocial problems, such as anxiety, depression, social isolation, loneliness, helplessness, and hopelessness. All of these psychosocial problems can increase patients’ need for holistic care, including attention to the person's environment and receiving support from family. If dialysis patients are better supported and cared for, these negative consequences might be prevented or at least decreased. This study was performed to determine the perceived social support from family and depression level of hemodialysis patients.
METHODS:
In this study, descriptive design was used. Data were collected during structured interviews in an outpatient clinic using a questionnaire. The questionnaire aimed to determine the patients’ descriptive characters and the scores of Beck Depression Inventory and Perceived Social Support from Family Scales. In data evaluation, descriptive statistics, Student's t tests, Kruskal Wallis tests, Mann-Whitney U tests and Pearson product moment correlations were used.
RESULTS:
The mean depression score was very high (23.2 ± 10.5). Significant differences were found between employment status and level of depressive symptoms. The mean level of perceived social support from family was 15.23 ± 5.37. There were no statistically significant differences between all the variables for the level of perceived social support from family. Perceived social support from family was negatively correlated with depression.
CONCLUSIONS:
The results of this study indicate that Turkish hemodialysis patients experience depression. However, patients who were dissatisfied with their social relationships had higher depression scores.
KEYWORDS: Depression, Social Support, Family, Kidney Failure, Chronic, Renal Dialysis, Patients
The presence of a chronic illness is a very stressful life event and can create significant psychological problems for patients. The chronic illness can have an impact on patients’ quality of life, potentially affecting their physical and mental health, functional status, independence, general well-being, personal relationships and social functioning.1–4 Patients undergoing dialysis may experience a lack of control over daily life activities and recreational and social activities, loss of independence, early retirement, financial stress, role alterations, disruption in family life, altered self-image, and diminished self-esteem. As a result, they also experience psychosocial problems, such as anxiety, depression, social isolation, loneliness, helplessness, and hopelessness.5–8 Psychosocial problems, such as those related to the extent of social support and depression and patients’ perceptions of their well-being, may also be related to outcome in patients with acute and chronic medical illness9,10 as well as in end stage renal disease (ESRD) patients treated with hemodialysis (HD).11–14 Such factors may affect compliance with treatment regimens.15 All of these psychosocial and physical limitations can increase patients’ need for holistic care, including attention to the person's environment and receiving support from family. If patients undergoing dialysis are better supported and cared for, these negative physio-psychosocial consequences might be prevented or at least decreased.
Patients who are dissatisfied with their social relationships are likely to be depressed.16
Illness or illness-related conditions might strongly affect patients’ perceived social support from family. Social interaction is expected to influence depressive symptoms in such a way that individuals whose network members are understanding, appreciative, and reliable (i.e., providing social support) are expected to experience lower levels of depressive symptoms.16 Conversely, individuals whose network members make them feel tense, make critical remarks, and get on their nerves (i.e., negative interactions) will experience heightened levels of depressive symptoms. In the absence of social support, however, patients are more likely to blame themselves for the event, have ruminating thoughts, and express their feelings in maladaptive ways, such as anger, withdrawal, or depression. Further, social relationships that are strained, involve social friction and isolation, or discourage discussion of illness-related feelings may increase depressive symptoms.16–17
Depression is generally considered the most common psychological problem encountered in patients with ESRD.18,19 The symptoms and signs of depression include low mood, diminished interest or pleasure in activities of daily living, weight change, insomnia, fatigue, restlessness, helplessness, hopelessness, and guilt, many of which are encountered among patients on dialysis. Difficulties in the identification and measurement of depression in patients with ESRD have been attributed to the similarity of depressive symptoms to those of uremia and other co-morbid conditions. The indicator of depression was lower than that reported in the literature for patients with chronic illness, supporting the notion that depression is both underdiagnosed and thus undertreated in patients on HD.20–23
The study of Brown et al on a community-based sample of 927 African Americans found no beneficial effects of close family ties (e.g., social support) on levels of depressive symptoms.24 Brown and Gary found that perceived support buffered the effect of stress on depressive symptoms among women, but not among men.25 In Turkey, few studies were focused on the relationship of family, anxiety, and depression in dialysis patients.5,26–29
Nurses are in a strategic position to provide holistic care for patients’ needs and responsible for assessing the progress of patients with chronic illness and its impact on patients. This care should include psychosocial as well as physical aspects of health. In providing this care, nurse should be aware of a patient's needs and must help patients express their feelings about their family and chronic illness.
The aim of the current study was to determine the perceived social support from family and depression level of hemodialysis patients.
Methods
Patients and Study Design
Using a descriptive design, this study included 147 subjects (84 female, 63 male) recruited by the researchers from the patients currently treated in three hemodialysis centres in Erzurum, Eastern Turkey. Subjects were informed of the purpose of the research and assured as volunteers of their rights to refuse participation or to withdraw from the study at any time. All of the patients treated by hemodialysis participated in this study. The patients were asked to participate in the study by the researcher. Full informed consent of the patients and ethical committee approval at both a regional and national level were obtained before the study.
The inclusion criterion of this study was being aged over 18 years. Exclusion criteria were using antidepressants at the time of the study. The patients with more than 17 points in Beck Depression Scale were referred to the psychiatry clinic for treatment.
Instruments
Demographic and Clinical Characteristics
Demographic and clinical characters are age, gender, education level, income level, marital status, family type, employment status and number of years since commenced dialysis.
Beck Depression Inventory (BDI)
The BDI was developed by Beck et al30 and was translated into Turkish by Hisli.31 In this study, the BDI was used to assess depressive symptoms. This is a 21-item, 4-point scale ranging from rarely or none of the time (0) to most or all of the time (3), and the highest score is 63; 1-10 is considered normal, 11-16 indicates mild mood disturbance, 17-20 indicates borderline clinical depression, 21-30 indicates moderate depression, 31-40 indicates severe depression, and over 40 indicates extreme depression. The BDI has had high internal consistency, with alpha coefficient of 0.86 and 0.81 for psychiatric and non-psychiatric populations, respectively.30 Reported alpha coefficient for the BDI was 0.74 in a Turkish population.31 In this study, the alpha coefficient for patients was 0.83.
Perceived Social Support Scale
Perceived social support was measured with the Perceived Social Support from Friends and Family Scale (PSS-Fr and PSS-Fa), developed by Procidano and Heller in 1984.32 The scale was translated into Turkish by Eskin, and the reported alpha coefficient in a Turkish population was 0.85 for the PSS-Fa and 0.75 for the PSS-Fr.33 Each scale contains 20 items to mark either true, false, or I do not know. The average score of the PSS-Fr and PSS-Fa for each participant was calculated. The levels of family support and friend support that patients and spouses perceived they had received were further judged as high or low by the average rating scores, based on being below or above the median point of the PSS-Fa and PSS-Fr scale scores. In this study, alpha coefficient of the PSS-Fa for patients was 0.70, because of only using the PSS-Fa.
Data Collection Procedure
The data were collected at the dialysis clinic by the researchers. During data collection, the questions were read to the patients, and their responses were marked on the questionnaires; some participants were poor at basic reading and writing skills. To ensure confidentiality and to enhance reliability, one of the researchers collected the data from patients.
Data Analysis
Statistical procedure was done by Statistical Program for Social Sciences software (SPSS) version 13. Descriptive statistics, Student's t tests, Kruskal Wallis tests, Mann-Whitney U tests and Pearson product moment correlations were used for data analyses. The significance level (p) was set at 0.05. The results are presented as mean ± SD.
Results
The Sample
Table 1 shows descriptive characteristics of the patients. 147 patients treated by hemodialysis participated in this study. The sample con-sisted of 84 (57.1%) female and 63 (42.9%) male patients. The mean age of the patients was 46.2 ± 14.9 years. More than half of the patients (53.1%) were primary school graduates. Most (73.5%) were from a nuclear family. Most of the patients (83.0%) were married. 127 patients (86.4%) were unemployed. Most of the patients (85%) reported that they had low income. 48 (32.7%) had received hemodialysis for 1 year or less; 26 (17.7%) for 1-2 years; 19 (12.9%) for 2-3 years; and 54 (36.7%) for more than 3 years.
Table 1.
Differences in descriptive characteristics of perceived social support from family and depression score (n = 147)
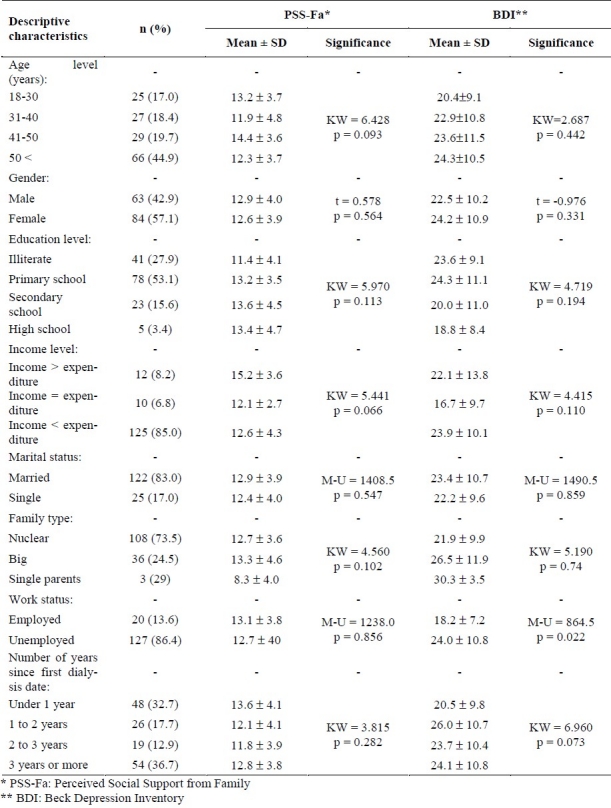
Differences in the Levels of Perceived Social Support
The mean level of perceived social support from family was 15.23 ± 5.37 in hemodialysis patients. There were no statistically significant differences between all the variables for the level of perceived social support from family (p > 0.05, Table 1).
Differences in Depression Levels
The mean of depression score was 23.2 ± 10.5 in hemodialysis patients. No significant differences were found between all the demographic variables for the level of depressive symptoms, however, there was a statistically significant difference between the status of employment and unemployment for depressive symptoms (Table 1).
Relationship between Depression Level and Social Support
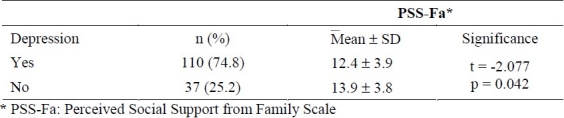
The scores of 110 (74.8%) patients were over the cut-off point of 17 for depressive symptoms (Table 2). 37 patients were below the cutoff point of 17 for depressive symptoms. No significant difference was found between the two groups in their depressive symptoms (t = -2.077, p = 0.042). However, a negative correlation was found between social support and depression in hemodialysis patients (r = -0.169, p < 0.05).
Table 2.
Depression for means and standard deviation of perceived social support from family
Discussion
This study was conducted to determine the depression level and the social support received from family by Turkish patients undergoing dialysis. It was found that none of the demographic variables had an effect on social support from family. Nevertheless, the level of perceived social support from family in hemodialysis patients was 15.23 ± 5.37, which suggested that the relationship between the patients and family was supportive. Previous studies have indicated that people who have experienced negative life events want to find family support.5,26 Informal social support networks are important for health and well-being and can be particularly helpful during difficult times. The common concern occurring among dialysis patients is the fear of losing love and approval from the family.34 Family members were major providers of social support for patients. In Turkey, patients are not cared for and attended by a hired caretaker. Instead, family members themselves provide the care for patients. This is consistent with the traditional culture of Turkish family, which is characterized with high coherence among family members. In view of patients’ good relationships with their families, they probably have assistance from their families when needed. Family support systems may operate through direct and indirect mechanisms. By direct pathways, the emotional and tangible support can promote adherence to treatments, buffering the effects of stress, and improving immune functioning. Assisting in indirect ways, family support may influence perceived quality of life and health status through the provision of tangible aid such as transporta-tion, access to medical services, housekeeping, money and other resources.8
The mean depression score of hemodialysis patients was 23.2 ± 10.5, which is very high. No significant differences were found between all the demographic variables for the level of depressive symptoms, however, there was a statistically significant difference between the status of employment and unemployment for depressive symptoms (Table 1). In this study, 127 (86.4%) were unemployed. Employment is an important aspect of life for many individuals in Turkey. Thus, support for employment should become an important aspect of the holistic care.35 Nurses can provide counseling on opportunities for employment and coping with unemployment. Nurses should also be advisory in matters of social and spare time activities. Nursing interventions include teaching patients about their conditions and community resources. Previous research showed that depression is common in hemodialysis patients.5,36,37 According to the result of studies on HD patients, depression is the most common psychiatric disorder, which causes morbidity and mortality.36,38 Depression frequently results in suicidal thoughts or suicide. Studies from various countries have reported that the prevalence of depression is 5-22% in patients with ESRD who undergo dialysis.5,37 In recent studies from our country, it has been reported that 22.9% of HD patients have at least one psychiatric disorder, the most common of which is depression.36,38 This was strongly supported by findings of the current study, in which 110 (74.8%) patients had high scores of depression. Thus, timely evaluation of the patient for potential mental health problems is important.
The levels of perceived social support from family and depression scores of the HD patients in this study showed an inverse relationship. Thus, people who are satisfied with relationships were less likely to be depressed. The results in this study are similar to the results of earlier studies.26,39 Tan et al showed that if the interfamily relationships of the patients were good, depression scores were low.26 Elal and Krepsi found that social support was associated with the level of depression.39 Likewise, Do an and Do an reported a negative correlation between depression and family relations of hemodialysis patients in a Turkish sample.5 The results of our study cannot be generalized to HD patients beyond the sample. Future studies with larger samples from different regions of Turkey are recommended to investigate whether the correlation between depression and perceived social support from family changes over time. Future study is recommended also to explore whether depression and perceived social support from family change over time by using regression model.
Conclusion
The study was performed to determine the social support and depression level of hemodi-alysis patients. In this study, the mean depression score was very high. The results of this study indicate that Turkish hemodialysis patients experience depression. However, patients who were dissatisfied with their social relationships had higher depression scores. The results indicate that nurses should know the signs and symptoms of depression, identify these signs and symptoms, and intervene appropriately to alleviate the conditions. Nurses must also be alert to possible sources of negative feelings, which may be either the illness or the life situation. Nurses should also be aware that family members are significant providers of social support for patients. Interventions, therefore, should include efforts to strengthen social networks and thus to relieve or reduce the stress of family burdens. Education programs for nurses should emphasize the importance of a holistic approach to care rather than overemphasizing technological aspects. In addition, nurses should encourage patients to express their feelings about their family and assist families in establishing a pattern of function that addresses the needs of family members, particularly of those who are chronically ill. Such interventions have the potential to enhance the satisfaction of life for these patients.
Additional research is needed regarding the relationship of social support and depression, which may only hold with short-term predictions. Studies on large numbers of severely depressed patients will contribute.
Authors’ Contributions
All the authors have carried out the study, participated in the design of the study and acquisition of data performed the statistical analysis and wrote the manuscript. All authors read and approved the final manuscript.
Footnotes
Conflict of Interests
Authors have no conflict of interests.
References
- 1.Lok P. Stressors, coping mechanisms and quality of life among dialysis patients in Australia. J Adv Nurs. 1996;23(5):873–81. doi: 10.1046/j.1365-2648.1996.00893.x. [DOI] [PubMed] [Google Scholar]
- 2.Blake C, Codd MB, Cassidy A, O’Meara YM. Physical function, employment and quality of life in end-stage renal disease. J Nephrol. 2000;13(2):142–9. [PubMed] [Google Scholar]
- 3.Suet-Ching WL. The quality of life for Hong Kong dialysis patients. J Adv Nurs. 2001;35(2):218–27. doi: 10.1046/j.1365-2648.2001.01839.x. [DOI] [PubMed] [Google Scholar]
- 4.Bakewell AB, Higgins RM, Edmunds ME. Quality of life in peritoneal dialysis patients: decline over time and association with clinical outcomes. Kidney Int. 2002;61(1):239–48. doi: 10.1046/j.1523-1755.2002.00096.x. [DOI] [PubMed] [Google Scholar]
- 5.Doğan S, Doğan O. Adana: Çukurova Üniversitesi; 1992. Hemodialize giren hastalarda depresyon, anksiyete ve aile ilişkilerinin değerlendirilmesi. Proceedings of III Ulusal Hemşirelik Kongresi Kitabı; 1992 Jun 24-26; Sivas, Turkey; pp. 495–500. [In Turkish] [Google Scholar]
- 6.Levy NB. Psychiatric considerations in the primary medical care of the patient with renal failure. Adv Ren Replace Ther. 2000;7(3):231–8. doi: 10.1053/jarr.2000.8132. [DOI] [PubMed] [Google Scholar]
- 7.Peters VJ, Hazel LA, Finkel P, Colls J. Rehabilitation experiences of patients receiving dialysis. (457).ANNA J. 1994;21(7):419–26. discussion 427. [PubMed] [Google Scholar]
- 8.Tell GS, Mittelmark MB, Hylander B, Shumaker SA, Russell G, Burkart JM. Social support and health related quality of life in black and white dialysis patients. ANNA J. 1995;22(3):301–8. discussion 309-10. [PubMed] [Google Scholar]
- 9.Frasure-Smith N, Lespérance F, Talajic M. Depression and 18-month survival after myocardial infarction. Circulation. 1995;91(4):999–1005. doi: 10.1161/01.cir.91.4.999. [DOI] [PubMed] [Google Scholar]
- 10.Cohen S, Doyle WJ, Skoner DP, Rabin BS, Gwaltney JM., Jr Social ties and susceptibility to the common cold. JAMA. 1997;277(24):1940–4. [PubMed] [Google Scholar]
- 11.Kimmel PL, Weihs K, Peterson RA. Survival in hemodialysis patients: the role of depression. J Am Soc Nephrol. 1993;4(1):12–27. doi: 10.1681/ASN.V4112. [DOI] [PubMed] [Google Scholar]
- 12.Christensen AJ, Wiebe JS, Smith TW, Turner CW. Predictors of survival among hemodialysis patients: effect of perceived family support. Health Psychol. 1994;13(6):521–5. doi: 10.1037//0278-6133.13.6.521. [DOI] [PubMed] [Google Scholar]
- 13.Peterson RA, Kimmel PL, Sacks CR, Mesquita ML, Simmens SJ, Reiss D. Depression, perception of illness and mortality in patients with end-stage renal disease. Int J Psych Med. 1991;21(4):343–54. doi: 10.2190/D7VA-FWEU-JN5Y-TD3E. [DOI] [PubMed] [Google Scholar]
- 14.Devins GM, Mann J, Mandin H, Paul LC, Hons RB, Burgess ED, et al. Psychosocial predictors of survival in end-stage renal disease. J Nerv Ment Dis. 1990;178(2):127–33. doi: 10.1097/00005053-199002000-00008. [DOI] [PubMed] [Google Scholar]
- 15.Lamping DL, Campbell KA. Hemodialysis compliance: assessment, prediction, and intervention: part I. Semin Dial. 1990;3(1):52–6. [Google Scholar]
- 16.Miller JF. Assessment of loneliness and spiritual well-being in chronically ill and healthy adults. J Prof Nurs. 1985;1(2):79–85. doi: 10.1016/s8755-7223(85)80010-7. [DOI] [PubMed] [Google Scholar]
- 17.Nolen-Hoeksema S, Davis CG. “Thanks for sharing that”: ruminators and their social support networks. J Pers Soc Psychol. 1999;77(4):801–14. doi: 10.1037//0022-3514.77.4.801. [DOI] [PubMed] [Google Scholar]
- 18.Finkelstein FO, Finkelstein SH. Depression in chronic dialysis patients: assessment and treatment. Nephrol Dial Transplant. 2000;15(12):1911–3. doi: 10.1093/ndt/15.12.1911. [DOI] [PubMed] [Google Scholar]
- 19.Kimmel P, Levy NB. Psychology and rehabilitation. In: Daugirdas JT, Blake PG, Ing TS, editors. Handbook of dialysis. 3rd ed. Philadelphia: Lippincott Williams & Wilkins; 2004. pp. 413–9. [Google Scholar]
- 20.Lopes AA, Bragg J, Young E, Goodkin D, Mapes D, Combe C, et al. Depression as a predictor of mortality and hospitalization among hemodialysis patients in the United States and Europe. Kidney Int. 2002;62(1):199–207. doi: 10.1046/j.1523-1755.2002.00411.x. [DOI] [PubMed] [Google Scholar]
- 21.Kutner NG, Fair PL, Kutner MH. Assessing depression and anxiety in chronic dialysis patients. J Psychosom Res. 1985;29(1):23–31. doi: 10.1016/0022-3999(85)90005-4. [DOI] [PubMed] [Google Scholar]
- 22.Mollaoglu M. Depression and health-related quality of life in hemodialysis patients. Dial Transplant. 2004;33(9):544–55. [Google Scholar]
- 23.Walters BA, Hays RD, Spritzer KL, Fridman M, Carter WB. Health-related quality of life, depressive symptoms, anemia, and malnutrition at hemodialysis initiation. Am J Kidney Dis. 2002;40(6):1185–94. doi: 10.1053/ajkd.2002.36879. [DOI] [PubMed] [Google Scholar]
- 24.Brown DR, Gary LE, Greene AD, Milburn NG. Patterns of social affiliation as predictors of depressive symptoms among urban blacks. J Health Soc Behav. 1992;33(3):242–53. [PubMed] [Google Scholar]
- 25.Brown DR, Gary LE. Stressful life events, social support networks and the physical and mental health of urban black adults. J Human Stress. 1987;13(4):165–74. doi: 10.1080/0097840X.1987.9936810. [DOI] [PubMed] [Google Scholar]
- 26.Tan M, Engin R, Özer H. Erzurum: Ulusal Hemşirelik Kongresi Bildilireli; 1999. Hemodiyalize giren hastalarda depresyon ve aile ilişkilerinin değerlendirilmesi; pp. 415–20. [Google Scholar]
- 27.Fallon M, Gould D, Wainright SP. Stress and quality of life in the renal transplant patient: a preliminary investigation. J Adv Nurs. 1999;25(3):562–70. doi: 10.1046/j.1365-2648.1997.1997025562.x. [DOI] [PubMed] [Google Scholar]
- 28.Lincoln KD, Chatters LM, Taylor RJ. Social support, traumatic events, and depressive symptoms among African Americans. J Marriage Fam. 2005;67(3):754–66. doi: 10.1111/j.1741-3737.2005.00167.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Gençöz T, Astan G. Social support, locus of control, and depressive symptoms in hemodialysis patients. Scand J Psychol. 2006;47(3):203–8. doi: 10.1111/j.1467-9450.2006.00508.x. [DOI] [PubMed] [Google Scholar]
- 30.Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Arch Gen Psychiatry. 1961;4:561–71. doi: 10.1001/archpsyc.1961.01710120031004. [DOI] [PubMed] [Google Scholar]
- 31.Hisli N. The reliability and validity study of the Beck Depression Inventory in a Turkish sample. Psikoloji Dergisi. 1988;6:118–22. [Google Scholar]
- 32.Procidano ME, Heller K. Measures of perceived social support from friends and from family: Three validation studies. Am J Community Psychol. 1983;11(1):1–24. doi: 10.1007/BF00898416. [DOI] [PubMed] [Google Scholar]
- 33.Eskin M. Reliability of the Turkish version of the Perceived Social Support from Friends and Family scales, Scale for Interpersonal Behaviour, and Suicide Probability Scale. J Clin Psychol. 1993;49(4):515–22. doi: 10.1002/1097-4679(199307)49:4<515::aid-jclp2270490408>3.0.co;2-k. [DOI] [PubMed] [Google Scholar]
- 34.Milde FK, Hart LK, Fearing MO. Sexuality and fertility concern of dialysis patients. ANNA J. 1996;23(3):307–315. discussion 314-5. [PubMed] [Google Scholar]
- 35.Chan CLW. Hong Kong: The Hospital Authority; 1997. Application of quality of life scales for persons with chronic illness.Proceedings of the Quality of Life Symposium; pp. 96–127. [Google Scholar]
- 36.Özkan S. Psychiatric morbidity in chronic renal failure and dialysis. Psychiatric Medicine: Consultation Liaison Psychiatry. 1993;1:187–90. [Google Scholar]
- 37.Rustomjee S, Smith GC. Consultation-liaison psychiatry to renal medicine: work with an inpatient unit. Aust N Z J Psychiatry. 1996;30(2):229–37. doi: 10.3109/00048679609076099. [DOI] [PubMed] [Google Scholar]
- 38.Sağduyu A, Erten Y. Psychiatric disorders in patients with end stage renal disease treated with hemodialysis. The Turkish Journal of Psychiatry. 1998;9(1):13–22. [Google Scholar]
- 39.Elal G, Krespi M. Life events, social support and depression in haemodialysis patients. J Community Appl Soc Psychol. 1999;9(1):23–33. [Google Scholar]


