Abstract
BACKGROUND:
This study aimed to evaluate the accuracy of Euroscore (European System for Cardiac Operative Risk Evaluation) in predicting perioperative mortality after cardiac surgery in Iranian patient population.
METHODS:
Data on 1362 patients undergoing coronary bypass graft surgery (CABG) from 2007 to 2009 were collected. Calibration was assessed by Hosmer-Lemeshow goodness-of-fit. Area under the curve (AUC) was used to assess score validity. Odds ratios were measured to evaluate the predictive value of each risk factor on mortality rate.
RESULTS:
The overall perioperative in hospital mortality was 3.6% whereas the Euroscore predicted a mortality of 3.96%. Euroscore model fitted well in the validation databases. The mean AUC was 66%. Mean length of intensive care unit (ICU) stay was 2.5 ± 2.5 days. Among risk factors, only left ventricular dysfunction, age and neurologic dysfunction were found to be related to mortality rate.
CONCLUSIONS:
Euroscore did not have acceptable discriminatory ability in perioperative in hospital mortality in Iranian patients. It seems that development of a local mortality risk scores corresponding to our patients epidemiologic characteristics may improve prediction of outcome.
Keywords: Euroscore model, hospital, mortality, preoperative, cardiac surgery
As the prevalence of coronary artery disease considerably increases in the world and in our country, the need for choosing effective, safe and reliable methods of treatment is felt more. Patients with coronary artery disease generally are old and suffer from other chronic underlying diseases; therefore, it is difficult to decide about appropriate protocols of treatment.
Today, cardiac surgery methods are developed and become possible in high risk patients but there is an increasing interest for cost-benefit analysis and also risk evaluation by valid risk scores.1–3 In other words, decision making about doing an operation depends on its likely risk and the benefit of it and the surgeon should weigh them up against each other.
Preoperative risk score such as Euroscore guides the surgeon and patients towards deciding whether or not to go ahead with surgery.3–5 Risk models are based on initial patient populations characteristic; therefore, its validity should be tested if it is supposed to be used elsewhere.6–9
Euroscore that was presented in 1995 was derived from specific European cardiac surgery protocols and it is based on epidemiological characteristics of that population.5 Risk models currently used do not adjust with advanced surgical techniques and improved post operation patients care which have been achieved during recent years, thus regularly revalidation of score items seems to be required.10–12 Besides, there are obviously some epidemiological differences between our population and European population, thus its accuracy should be evaluated in our patients’ population.13 Simple additive Euroscore is valuable risk model and gives a useful estimate of risk in individual patients but in high risk patients it may underestimate the risk. The logistic Euroscore can predict the risk more accurately, especially in high risk patients.14 So this study aimed to evaluate the accuracy of logistic Euroscore (European System for Cardiac Operative Risk Evaluation) in predicting perioperative mortality after cardiac surgery in Iranian patient population.
Methods
The present study included 1511 patients undergoing coronary artery bypass graft (CABG) during 2 years from 2007 to 2009 in Sina hospital of Esfahan. The sample size was defined based on previous studies.6 All patients gave their written informed consent before their surgery and entering into study. The study was approved by the Research Ethics Committee of Isfahan University of Medical Sciences, Isfahan Sina Heart Center.
Data for the studied patients including demographics, clinical characteristics, laboratory data, medical treatments, preoperative (patients related factors and cardiac related factors), operative data and length of ICU stay (LOS) were collected by reviewing hospital record files in a computerized database.
Perioperative mortality which was defined as death during 30 days from the operation was asked through telephone. LOS more than 2 days was considered prolonged LOS. Totally, 149 patients were excluded from our study because of not replying to telephone. Euroscore was calculated retrospectively. We used similar methodology previously applied by others with the same variables in the Euroscore.12,13,15 Data were analyzed by logistic regression statistical test.
Accuracy (validation and reliability) of the Euroscore was assessed by the area under the curve (AUC). AUC greater than 0.7 was considered as an acceptable discriminatory ability. Hosmer-lemeshow chi-square test was used to assess the calibration of the Euroscore model.
Data analysis was performed by the SPSS soft ware (version 14, SPSS Inc., Chicago, IL).
Results
Table 1 shows clinical and demographic characteristics of the studied population. Totally, 24.9% (376 patients out of 1511 patients) were female and 74.9% (1103 patients) were male. Mean age was 59.7 ± 10.2. 149 patients were excluded from our study because of not accessibility. Mortality rate in 1362 patients was 3.6%. The logistic Euroscore predicted perioperative in hospital mortality rate of 3.9%. Logistic regression model calibrated well to our sample and gave P value of 0.89 in the Hosmer-lemeshow chi-square test. Table 2 shows predictive value of Euroscore items. Odd ratios calculations revealed that predictive values for well-accepted risk factors such as unstable angina, sex and renal failure were not significant. Left ventricular dysfunction, older age and neurologic dysfunction were significantly related to the mortality rate.
Table 1.
Clinical and demographic characteristics of the studied population
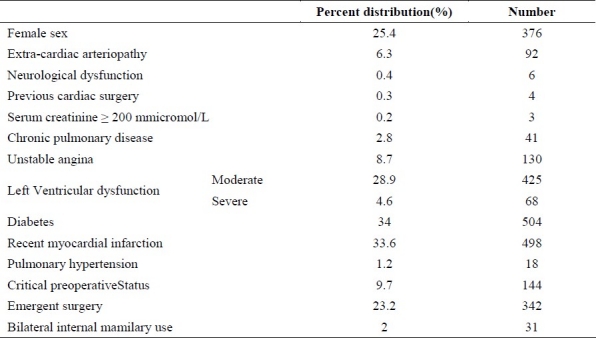
Table 2.
Association of Euroscore risk factors of study population and occurrence of death by multivariate logistic regression analysis
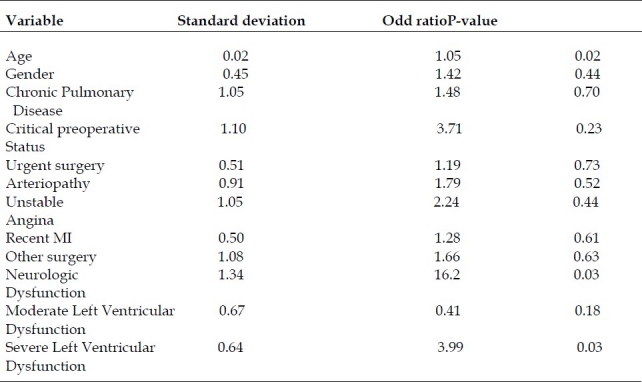
Figure 1 shows percent distribution of risk factors among the patients. Mean LOS, ranging from 0 - 49 days, was 2.5 ± 2.5 days, and median was 2 days. Prolonged LOS occurred in 18.3% of the patients. The AUC for the logistic Euroscore was 0.66 (95% CI) [Figure 2]. Using the receiver operating characteristics (ROC) curve analysis, we found an optimal cut off point with 66% sensitivity and 62% specificity that corresponded to the score of 0.028 (in logistic Euroscore) being able to separate death probability from surviving probability. It means we can correctly predict 66% of the death (sensitivity) and 62% of the surviving (specificity).
Figure 1.
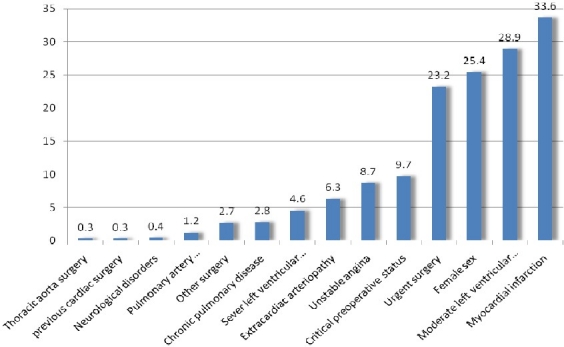
Percent distribution of risk factors in the study population
Figure 2.
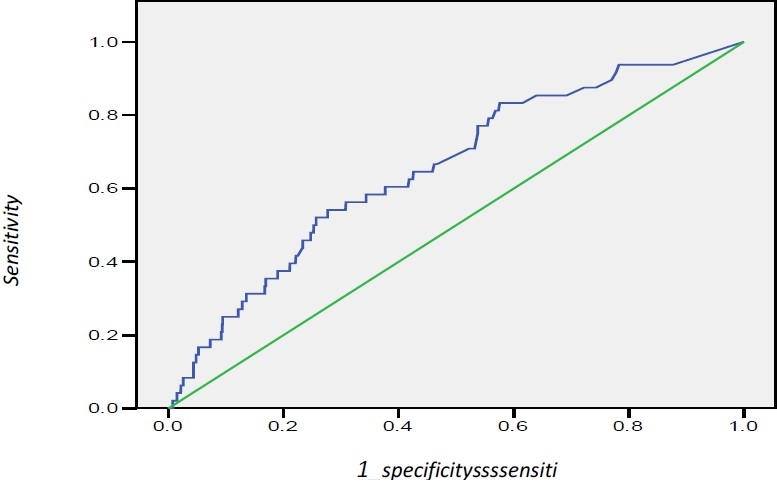
Receiver operating characteristics (ROC) curve of Euroscore for mortality prediction
Discussion
Observed unadjusted preoperative mortality in our CABG patients was 3.6% almost equal to that of the other similar studies.4,15,16 We concluded that Euroscore would be relatively incapable of accurate prediction of perioperative mortality in our patients’ population and the most important target of our study was to confirm this assumption.
AUC in our study was measured 66%. Roque et al. assessing predictive value of Euroscore in six countries of European Union concluded that additive Euroscore model works well across European countries.17 Geissler et al. compared 6 risk models and found the greatest AUC for Euroscore (78%).4 In Nashef et al. study in North America, AUC for Euroscore was75%.16 Other similar studies also reported near results.1,18
Since the least AUC for Euroscore model in most of the studies was 75% and the AUC >70% usually demonstrates a good predictive value, it seems that Euroscore risk model has less discriminatory power in predicting preoperative morality in our patients. In fact, according to the results, this risk model did not accurately predict preoperative mortality; therefore, it may not be suitable for use in our patients’ population.
In our study, 18.3% of patients had prolonged ICU stay. This was almost similar to Wong et al. study result in which 17% of CABG patients stayed more than 2 days in the ICU.19 Although, Pitkanen et al. reported 4.8% and 6.5% prolonged ICU stay in their results, but mean LOS was 1.9% ± 1.9% and 1.4 ± 1.9 days that was close to our results.20 Although, it is obvious that reliable conclusion about the quality of care in individual hospital would require more information collection with validity assessment and we don’t argue about that in the present article, the quality of care provided in our hospital have been comparable with that of Europeans countries.
Among risk factors, only 3 ones, age (P < 0.02), poor left ventricular dysfunction (P < 0.03) and neurological dysfunction (P < 0.03), were found to be associated to mortality rate. Other previously published studies claimed that all or most of these predictors had significant effects on morality rate.
Limitation
Because of time limitation, the sample size of this study was smaller than similar studies.
Conclusion
Since these models were developed for specific patient population and they should not be applied elsewhere without appropriate validation for respective patient population, we recommend developing a risk model that can accurately predict perioperative mortality in our patient population waiting for CABG surgery with due attention to regional demographic and epidemiologic variables.
Authors’ Contributions
MMS designed the study and drafted this manuscript; MA carried out the study and drafted the tables; MG drafted the manuscript; PN carried out the study and drafted the tables; HSH helped in designing the study; FMS carried out the study; AK helped in designing and carried out the study; PMS did the data analysis, and NF helped in Data collection. All authors have read and approved the final manuscript.
Acknowledgments
This program was supported by Sina Heart Center, Delasa Research Center.
Footnotes
Conflict of Interests Authors have no conflict of interests.
References
- 1.Higgins TL. Quantifying risk and assessing outcome in cardiac surgery. J Cardiothorac Vasc Anesth. 1998;12(3):330–40. doi: 10.1016/s1053-0770(98)90018-0. [DOI] [PubMed] [Google Scholar]
- 2.Asimakopoulos G, Al Ruzzeh S, Ambler G, Omar RZ, Punjabi P, Amrani M, et al. An evaluation of existing risk stratification models as a tool for comparison of surgical performances for coronary artery bypass grafting between institutions. Eur J Cardiothorac Surg. 2003;23(6):935–41. doi: 10.1016/s1010-7940(03)00165-9. [DOI] [PubMed] [Google Scholar]
- 3.Nilsson J, Algotsson L, Hoglund P, Luhrs C, Brandt J. Comparison of 19 pre-operative risk stratification models in open-heart surgery. Eur Heart J. 2006;27(7):867–74. doi: 10.1093/eurheartj/ehi720. [DOI] [PubMed] [Google Scholar]
- 4.Geissler HJ, Holzl P, Marohl S, Kuhn-Regnier F, Mehlhorn U, Sudkamp M, et al. Risk stratification in heart surgery: comparison of six score systems. Eur J Cardiothorac Surg. 2000;17(4):400–6. doi: 10.1016/s1010-7940(00)00385-7. [DOI] [PubMed] [Google Scholar]
- 5.Roques F, Nashef SA, Michel P, Gauducheau E, de Vincentiis C, Baudet E, et al. Risk factors and outcome in European cardiac surgery: analysis of the EuroSCORE multinational database of 19030 patients. Eur J Cardiothorac Surg. 1999;15(6):816–22. doi: 10.1016/s1010-7940(99)00106-2. [DOI] [PubMed] [Google Scholar]
- 6.Nashef SA, Roques F, Michel P, Cortina J, Faichney A, Gams E, et al. Coronary surgery in Europe: comparison of the national subsets of the European system for cardiac operative risk evaluation database. Eur J Cardiothorac Surg. 2000;17(4):396–9. doi: 10.1016/s1010-7940(00)00380-8. [DOI] [PubMed] [Google Scholar]
- 7.Ivanov J, Tu JV, Naylor CD. Ready-made, recalibrated, or Remodeled? Issues in the use of risk indices for assessing mortality after coronary artery bypass graft surgery. Circulation. 1999;99(16):2098–104. doi: 10.1161/01.cir.99.16.2098. [DOI] [PubMed] [Google Scholar]
- 8.Akar AR, Kurtcephe M, Sener E, Alhan C, Durdu S, Kunt AG, et al. Validation of the EuroSCORE risk models in Turkish adult cardiac surgical population. Eur J Cardiothorac Surg. 2011 doi: 10.1016/j.ejcts.2011.01.002. [DOI] [PubMed] [Google Scholar]
- 9.Malik M, Chauhan S, Malik V, Gharde P, Kiran U, Pandey RM. Is EuroSCORE applicable to Indian patients undergoing cardiac surgery? Ann Card Anaesth. 2010;13(3):241–5. doi: 10.4103/0971-9784.69082. [DOI] [PubMed] [Google Scholar]
- 10.Ribera A, Ferreira-Gonzalez I, Cascant P, Pons JM, Permanyer-Miralda G. The EuroSCORE and a local model consistently predicted coronary surgery mortality and showed complementary properties. J Clin Epidemiol. 2008;61(7):663–70. doi: 10.1016/j.jclinepi.2006.10.025. [DOI] [PubMed] [Google Scholar]
- 11.Li Y, Zheng Z, Hu S. The Chinese coronary artery bypass grafting registry study: analysis of the national multicentre database of 9248 patients. Heart. 2009;95(14):1140–4. doi: 10.1136/hrt.2008.146563. [DOI] [PubMed] [Google Scholar]
- 12.Yap CH, Reid C, Yii M, Rowland MA, Mohajeri M, Skillington PD, et al. Validation of the EuroSCORE model in Australia. Eur J Cardiothorac Surg. 2006;29(4):441–6. doi: 10.1016/j.ejcts.2005.12.046. [DOI] [PubMed] [Google Scholar]
- 13.Ferraris V A, Ferraris S P. Risk stratification and comorbidity. In: Cohn LH, Edmunds LH Jr, editors. Cardiac Surgery in the Adult. 2nd ed. New York: McGraw-Hill; 2003. pp. 187–224. [Google Scholar]
- 14.van Straten AH, Tan EM, Hamad MA, Martens EJ, van Zundert AA. Evaluation of the EuroSCORE risk scoring model for patients undergoing coronary artery bypass graft surgery: a word of caution. Neth Heart J. 2010;18(7-8):355–9. doi: 10.1007/BF03091791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Nashef SA, Roques F, Michel P, Gauducheau E, Lemeshow S, Salamon R. European system for cardiac operative risk evaluation (EuroSCORE) Eur J Cardiothorac Surg. 1999;16(1):9–13. doi: 10.1016/s1010-7940(99)00134-7. [DOI] [PubMed] [Google Scholar]
- 16.Nashef SA, Roques F, Hammill BG, Peterson ED, Michel P, Grover FL, et al. Validation of European System for Cardiac Operative Risk Evaluation (EuroSCORE) in North American cardiac surgery. Eur J Cardiothorac Surg. 2002;22(1):101–5. doi: 10.1016/s1010-7940(02)00208-7. [DOI] [PubMed] [Google Scholar]
- 17.Roques F, Nashef SA, Michel P, Pinna PP, David M, Baudet E. Does EuroSCORE work in individual European countries? Eur J Cardiothorac Surg. 2000;18(1):27–30. doi: 10.1016/s1010-7940(00)00417-6. [DOI] [PubMed] [Google Scholar]
- 18.Antunes PE, Eugenio L, Ferrao dO, Antunes MJ. Mortality risk prediction in coronary surgery: a locally developed model outperforms external risk models. Interact Cardiovasc Thorac Surg. 2007;6(4):437–41. doi: 10.1510/icvts.2007.152017. [DOI] [PubMed] [Google Scholar]
- 19.Wong DT, Cheng DC, Kustra R, Tibshirani R, Karski J, Carroll-Munro J, et al. Risk factors of delayed extubation, prolonged length of stay in the intensive care unit, and mortality in patients undergoing coronary artery bypass graft with fast-track cardiac anesthesia: a new cardiac risk score. Anesthesiology. 1999;91(4):936–44. doi: 10.1097/00000542-199910000-00012. [DOI] [PubMed] [Google Scholar]
- 20.Pitkanen O, Niskanen M, Rehnberg S, Hippelainen M, Hynynen M. Intra-institutional prediction of outcome after cardiac surgery: comparison between a locally derived model and the EuroSCORE. Eur J Cardiothorac Surg. 2000;18(6):703–10. doi: 10.1016/s1010-7940(00)00579-0. [DOI] [PubMed] [Google Scholar]


