Abstract
BACKGROUND:
Recent epidemiologic studies have found that self-reported sleep duration is associated with components of metabolic syndrome (MS) such as obesity, diabetes and hypertension. This relation may be under influence of regional factors in different regions of the world. The association of sleep duration and MS in a sample of Iranian people in the central region of Iran was investigated in this study.
METHODS:
This cross-sectional study was conducted as a part of the Isfahan Healthy Heart Program (IHHP). A total of 12492 individuals aged over 19 years, 6110 men and 6382 women entered the study. Definition of National Cholesterol Education Program was used to define MS. Sleep duration was reported by participants. Relation between sleep duration with MS was examined using categorical logistic regression in two models; unadjusted and adjusted for age and sex.
RESULTS:
In our study, 23.5 % of participants had MS. Compared with sleep duration of 7-8 hours per night; sleep duration of less than 5 hours was associated with a higher odds ratio for MS. This association remained significant even after adjustment for age and sex (OR: 1.52; 95%CI: 1.33-1.74). However, sleep duration of 9 hours or more showed a protective association with MS (OR: 0.79; 95%CI: 0.68-0.94).
CONCLUSIONS:
There was a positive relation between sleep deprivation and MS and its components. This relation was slightly affected by sex and age.
Keywords: Sleep, Metabolic Syndrome, Heart, Population
Metabolic syndrome (MS) consists of a constellation of metabolic abnormalities that presents increased risk of cardiovascular disease (CVD).1 The criteria for the MS have evolved since the original definition by the World Health Organization in 1998, reflecting growing clinical evidence and analysis by a variety of consensus conferences and professional organizations.2 The major features of the MS include central obesity, hypertriglyceridemia, low HDL cholesterol, hyperglycemia, and hypertension. According to Adult Treatment Panel (ATP III), three of these criteria characterize MS.3
The prevalence of obesity and type 2 diabetes is increasing worldwide. The causes of this pandemic are not fully explained by changes in traditional lifestyle factors such as diet and physical activity.4 Concurrent with these rises, there has been a similar epidemic of chronic sleep deprivation.5 According to the study of Sarrfzadegan et al, age-adjusted prevalence of MS in the central region of Iran was 23.3%. The prevalence was higher among women and urban individuals.6
Recent epidemiologic studies have found that self-reported habitual sleep duration is associated with obesity, diabetes, hypertension, and higher mortality.7–21 Both cross-sectional and prospective epidemiologic studies have linked sleep durations of 6 hours or less per night with increased prevalence and incidence of hypertension.5,16 Moreover, it has been shown that mid life adults who are short sleepers are at increased risk for CVD.19–22
Studies on the association between sleep and health are relatively new in Iran. This study aimed to assess the association of MS components with sleep duration in a sample of Iranian men and women.
Methods
Study population
This cross-sectional study was conducted as a part of the Isfahan Healthy Heart Program (IHHP). IHHP was a six year comprehensive integrated community based program for CVD prevention and control via reducing CVD risk factors and improvement of cardiovascular healthy behaviors.23
Participants were 12514 individuals aged over 19 years, that 12492 of them (6110 men and 6382 women) had lipid profile measurements. After signing informed written consent, sociodemographic characteristics such as age, sex, marital status, occupation, education and income were recorded. Sleep time was obtained by the question “how many hours of sleep do you usually get?”.23 This study was approved in Research Council of Isfahan Cardiovascular Research Center.
Height, weight, waist circumference (WC) and blood pressure were measured by trained health professionals. Weight was measured with calibrated scale in the standing position and with light cloths. Height was measured in the standing position with the subject bare-foot.24 Body mass index (BMI) was calculated as weight/height2 (kg/m2). Waist circumference was measured at the part of the trunk located midway between the lower costal margin (bottom of lower rib) and the iliac crest (top of pelvic bone) while the person was standing, with feet about 25-30 cm apart.24 Blood pressure was measured twice on the right arm, in sitting position and after 15 minutes rest. The mean of two recordings was reported. The first and 5th Korotkoff sounds were considered as systolic and diastolic blood pressure, respectively.25
Metabolic syndrome were defined as subjects who had three or more of the following criteria as defined by the National Cholesterol Education Program:26 (1) Central obesity as the waist circumference > 102 cm in men and > 88 cm in women; (2) Fasting plasma triglycerides ≥ 150 mg/dl; (3) low HDL cholesterol with fasting HDL cholesterol < 40 mg/dl in men and < 50 mg/dl in women; (4) hypertension with systolic blood pressure ≥ 130 mmHg and/or diastolic blood pressure 85 mmHg and/or antihypertensive agents (5) hyperglycemia with fasting plasma glucose ≥ 100 mg/dl and/or hypoglycemic medications.
Data was recorded and analyzed using SPSS for Windows (version 15.0; SPSS Inc., Chicago, IL, USA). Chi-square and ANOVA test were used to compare qualitative and quantitative data, respectively. The relation between sleep duration with MS was examined using multinomial logistic regression in two models, in the first model adjusted by age separated in sex group. In the second one, the model was adjusted by sex based on age groups.
Results
The study population included 49.9% men and 51.1% women with a mean age of 38.89 ± 14.93 years. In our study, 23.5 % of participants had MS. Of all participants, 61% reported sleeping 7-8 hours per night, 11.6% reported sleeping 5 hours or less and 8.7% reported sleeping 9 hours or more. Subjects with lower sleep duration were older and had a higher BMI and WC (P < 0.01) (Table 1).
Table 1.
Characteristic of the study participants
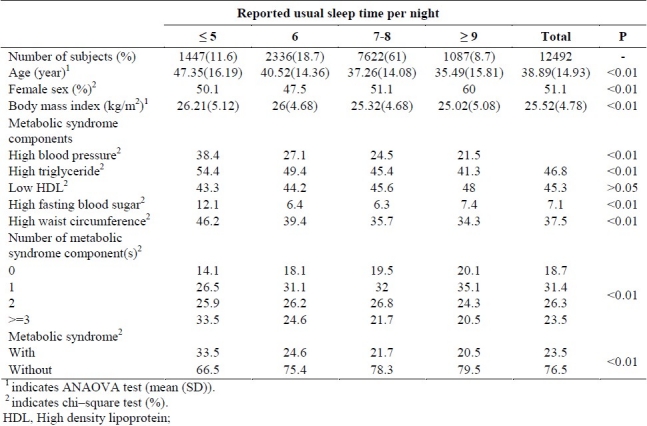
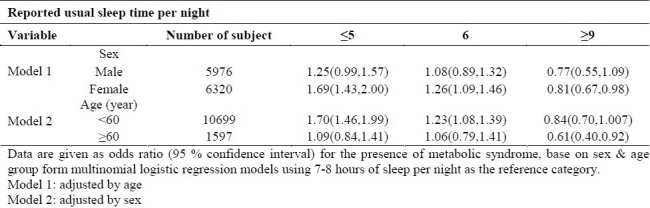
Compared with sleep duration of 7-8 hours per night, sleep duration < 5 hours was associated with a higher odds ratio for MS. This association remained significant even after adjustment for age and sex. However, sleep duration of 9 hours or more showed a protective effect on MS (Table 2).
Table 2.
Odds ratio of metabolic syndrome in different usual sleep time per night categories

After adjustment for age, odds ratio of MS in females increased in sleep duration less than 5 hours and decreased in sleep duration over 9 hour (model 1, Table 3). After adjustment for sex, odds ratio of MS in people under 60 years increased in sleep duration less than 5 hours and decreased in sleep duration over 9 hours (model 2, Table 3).
Table 3.
Odds ratio of metabolic syndrome in different usual sleep per night categories based on sex and age group
Discussion
In this study we found association between MS and sleep duration in women aged less than 60 years with sleep duration below 5 hours. Sleep duration over 9 hours showed a protective effect on MS in women over 60 years.
Our findings are different from similar studies in other countries. Hall et al27 reported that after adjustment for use of antihypertensive medication, prevalence of MS and its components remained high in short sleepers of American people. Only short sleep duration was correlated to MS, while sex was not a significant factor. In a sample of Korean people, Choi28 found that both short and long sleep durations are related to increased risk of the MS and its components. In the Korean population more components of the MS were highly associated with sleep duration in subjects less than 60 years old compared to those over 60. Altogether, these studies suggest that sleep duration may be an important risk factor for the MS. There is no explanation for the differences in the effect of sex and age on interaction of sleep duration and MS between our study and other similar studies. It may be related to genetic ethnicity or differences in daily life stresses.
In healthy subjects, experimental sleep restriction causes insulin resistance and increases evening cortisol and sympathetic activation.29 In the general population, obstructive sleep apnea is associated with glucose intolerance.29 Possible pathways linking short sleep duration to hypertension and cardiovascular events include increases in body weight and changes in glucose metabolism. Nedeltcheva et al30 tested the hypothesis that the curtailment of human sleep could promote excessive energy intake. In this study sleep restriction was accompanied by increased consumption of calories from snacks, with higher carbohydrate content, particularly during the period from 19:00 to 07:00. Therefore, recurrent bedtime restriction can modify the amount, composition, and distribution of human food intake. In another study a single night of sleep deprivation increased ghrelin levels and feelings of hunger in nine normal-weight healthy men.31
Sleep deprivation is associated with a dys-regulation of the neuroendocrine control of appetite, with a reduction of the satiety factor, leptin, and an increase in the hunger-promoting hormone, ghrelin. Thus, sleep loss may alter the ability of leptin and ghrelin to accurately signal caloric need, acting in concert to produce an internal misperception of insufficient energy availability.32 In one study, the effects of sleep duration on leptin were quantitatively associated with alterations of the cortisol and TSH profiles and were accompanied by an elevation of post breakfast homeostasis model assessment values.5
These studies suggest a relationship between sleep restriction, weight gain and diabetes. This risk may involve at least three pathways: alterations in glucose metabolism, upregulation of appetite and decreased energy expenditure.33
Most of these studies have shown association between short sleep duration and components of MS, however, there is little evidence on the relation between long sleep duration and MS components. Long sleep duration might be a compensation for or a reaction to stressful living conditions. If this is right, then more sleep hours may act as a coping strategy, alleviating some adverse effects of stresses on health. It may also act simply as a protective factor, saving individual from stressful hours. We did not differentiate between short or long sleep duration and disordered sleep or sleep apnea.
Conclusion
There is a relation between sleep duration and MS and its components. This relation is affected slightly by sex and age. However, this cross-sectional study could not deduce a causal relation between sleep duration and MS. Further studies are needed to clarify whether sleep duration can be considered as a cardiovascular risk factor. As the incidence of sleep deprivation is increasing, it would be an essential health problem in the future.
Authors’ Contributions
JN carried out the design and prepared the manuscript. NM coordinated the study design and participated in data collection and prepared the manuscript. NT provided assistance in design and manuscript preparation. All authors have read and approved the content of the manuscript.
Acknowledgments
This program was conducted by Isfahan Cardiovascular Research Center (ICRC) (a WHO Collaborating Center) in collaboration with Isfahan Provincial Health Office, both affiliated to Isfahan University of Medical Sciences (IUMS). The program was supported by grant No. 31309304 of the Iranian Budget and Planning Organization, as well as the Deputy for Health of the Iranian Ministry of Health, Treatment and Medical Education, and the Iranian Heart Foundation (IHF). We are thankful to collaborating teams in ICRC, Isfahan Provincial Health Office, Najaf-Abad Health Office and Arak University of Medical Sciences.
Footnotes
Conflict of Interests Authors have no conflict of interests.
References
- 1.Mullington JM, Haack M, Toth M, Serrador JM, Meier-Ewert HK. Cardiovascular, inflammatory, and metabolic consequences of sleep deprivation. Prog Cardiovasc Dis. 2009;51(4):294–302. doi: 10.1016/j.pcad.2008.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ekel RH. The metabolic syndrome. In: Fauci AS, Eugene B, Hauser SL, Longo DL, Jameson J, Joseph L, editors. Harrison's principles of internal medicine. 17th ed. New York: McGraw-Hill; 2008. p. 1015. [Google Scholar]
- 3.Executive Summary of the Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, And Treatment of High Blood Cholesterol In Adults (Adult Treatment Panel III) JAMA. 2001;285(19):2486–97. doi: 10.1001/jama.285.19.2486. [DOI] [PubMed] [Google Scholar]
- 4.Hu FB, Manson JE, Stampfer MJ, Colditz G, Liu S, Solomon CG, et al. Diet, lifestyle, and the risk of type 2 diabetes mellitus in women. N Engl J Med. 2001;345(11):790–7. doi: 10.1056/NEJMoa010492. [DOI] [PubMed] [Google Scholar]
- 5.Knutson KL, Spiegel K, Penev P, Van Cauter E. The metabolic consequences of sleep deprivation. Sleep Med Rev. 2007;11(3):163–78. doi: 10.1016/j.smrv.2007.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sarrafzadegan N, Kelishadi R, Baghaei A, Hussein SG, Malekafzali H, Mohammadifard N, et al. Metabolic syndrome: an emerging public health problem in Iranian women: Isfahan Healthy Heart Program. Int J Cardiol. 2008;131(1):90–6. doi: 10.1016/j.ijcard.2007.10.049. [DOI] [PubMed] [Google Scholar]
- 7.Patel SR, Malhotra A, White DP, Gottlieb DJ, Hu FB. Association between reduced sleep and weight gain in women. Am J Epidemiol. 2006;164(10):947–54. doi: 10.1093/aje/kwj280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yaggi HK, Araujo AB, McKinlay JB. Sleep duration as a risk factor for the development of type 2 diabetes. Diabetes Care. 2006;29(3):657–61. doi: 10.2337/diacare.29.03.06.dc05-0879. [DOI] [PubMed] [Google Scholar]
- 9.Knutson KL. Sex differences in the association between sleep and body mass index in adolescents. J Pediatr. 2005;147(6):830–4. doi: 10.1016/j.jpeds.2005.07.019. [DOI] [PubMed] [Google Scholar]
- 10.Gangwisch JE, Malaspina D, Boden-Albala B, Heymsfield SB. Inadequate sleep as a risk factor for obesity: analyses of the NHANES I. Sleep. 2005;28(10):1289–96. doi: 10.1093/sleep/28.10.1289. [DOI] [PubMed] [Google Scholar]
- 11.Mallon L, Broman JE, Hetta J. High incidence of diabetes in men with sleep complaints or short sleep duration: a 12-year follow-up study of a middle-aged population. Diabetes Care. 2005;28(11):2762–7. doi: 10.2337/diacare.28.11.2762. [DOI] [PubMed] [Google Scholar]
- 12.Ayas NT, White DP, Al Delaimy WK, Manson JE, Stampfer MJ, Speizer FE, et al. A prospective study of self-reported sleep duration and incident diabetes in women. Diabetes Care. 2003;26(2):380–4. doi: 10.2337/diacare.26.2.380. [DOI] [PubMed] [Google Scholar]
- 13.Gottlieb DJ, Punjabi NM, Newman AB, Resnick HE, Redline S, Baldwin CM, et al. Association of sleep time with diabetes mellitus and impaired glucose tolerance. Arch Intern Med. 2005;165(8):863–7. doi: 10.1001/archinte.165.8.863. [DOI] [PubMed] [Google Scholar]
- 14.Taheri S, Lin L, Austin D, Young T, Mignot E. Short sleep duration is associated with reduced leptin, elevated ghrelin, and increased body mass index. PLoS Med. 2004;1(3):e62. doi: 10.1371/journal.pmed.0010062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hasler G, Buysse DJ, Klaghofer R, Gamma A, Ajdacic V, Eich D, et al. The association between short sleep duration and obesity in young adults: a 13-year prospective study. Sleep. 2004;27(4):661–6. doi: 10.1093/sleep/27.4.661. [DOI] [PubMed] [Google Scholar]
- 16.Gangwisch JE, Heymsfield SB, Boden-Albala B, Buijs RM, Kreier F, Pickering TG, et al. Short sleep duration as a risk factor for hypertension: analyses of the first National Health and Nutrition Examination Survey. Hypertension. 2006;47(5):833–9. doi: 10.1161/01.HYP.0000217362.34748.e0. [DOI] [PubMed] [Google Scholar]
- 17.Cappuccio FP, Stranges S, Kandala NB, Miller MA, Taggart FM, Kumari M, et al. Gender-specific associations of short sleep duration with prevalent and incident hypertension: the Whitehall II Study. Hypertension. 2007;50(4):693–700. doi: 10.1161/HYPERTENSIONAHA.107.095471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ayas NT, White DP, Manson JE, Stampfer MJ, Speizer FE, Malhotra A, et al. A prospective study of sleep duration and coronary heart disease in women. Arch Intern Med. 2003;163(2):205–9. doi: 10.1001/archinte.163.2.205. [DOI] [PubMed] [Google Scholar]
- 19.Amagai Y, Ishikawa S, Gotoh T, Doi Y, Kayaba K, Nakamura Y, et al. Sleep duration and mortality in Japan: the Jichi Medical School Cohort Study. J Epidemiol. 2004;14(4):124–8. doi: 10.2188/jea.14.124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kripke DF, Garfinkel L, Wingard DL, Klauber MR, Marler MR. Mortality associated with sleep duration and insomnia. Arch Gen Psychiatry. 2002;59(2):131–6. doi: 10.1001/archpsyc.59.2.131. [DOI] [PubMed] [Google Scholar]
- 21.Patel SR, Ayas NT, Malhotra MR, White DP, Schernhammer ES, Speizer FE, et al. A prospective study of sleep duration and mortality risk in women. Sleep. 2004;27(3):440–4. doi: 10.1093/sleep/27.3.440. [DOI] [PubMed] [Google Scholar]
- 22.Ferrie JE, Shipley MJ, Cappuccio FP, Brunner E, Miller MA, Kumari M, et al. A prospective study of change in sleep duration: associations with mortality in the Whitehall II cohort. Sleep. 2007;30(12):1659–66. doi: 10.1093/sleep/30.12.1659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sarraf-Zadegan N, Sadri G, Malek AH, Baghaei M, Mohammadi FN, Shahrokhi S, et al. Isfahan Healthy Heart Programme: a comprehensive integrated community-based programme for cardiovascular disease prevention and control.Design, methods and initial experience. Acta Cardiol. 2003;58(4):309–20. doi: 10.2143/AC.58.4.2005288. [DOI] [PubMed] [Google Scholar]
- 24.The practical guide: identification, evaluation, and treatment of overweight and obesity in adults. Maryland: NIH Publication; 2000. North American Association for the Study of Obesity, National Heart LaBI, National Institutes of Health (U.S), NHLBI Obesity Education Initiative. [Google Scholar]
- 25.An epidemiological approach to describing risk associated with blood pressure levels. Final report of the Working Group on Risk and High Blood Pressure. Hypertension. 1985;7(4):641–51. [PubMed] [Google Scholar]
- 26.Grundy SM, Brewer HB, Jr, Cleeman JI, Smith SC, Jr, Lenfant C. Definition of metabolic syndrome: Report of the National Heart, Lung, and Blood Institute/American Heart Association conference on scientific issues related to definition. Circulation. 2004;109(3):433–8. doi: 10.1161/01.CIR.0000111245.75752.C6. [DOI] [PubMed] [Google Scholar]
- 27.Hall MH, Muldoon MF, Jennings JR, Buysse DJ, Flory JD, Manuck SB. Self-reported sleep duration is associated with the metabolic syndrome in midlife adults. Sleep. 2008;31(5):635–43. doi: 10.1093/sleep/31.5.635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Choi KM, Lee JS, Park HS, Baik SH, Choi DS, Kim SM. Relationship between sleep duration and the metabolic syndrome: Korean National Health and Nutrition Survey 2001. Int J Obes (Lond) 2008;32(7):1091–7. doi: 10.1038/ijo.2008.62. [DOI] [PubMed] [Google Scholar]
- 29.Levy P, Bonsignore MR, Eckel J. Sleep, sleep-disordered breathing and metabolic consequences. Eur Respir J. 2009;34(1):243–60. doi: 10.1183/09031936.00166808. [DOI] [PubMed] [Google Scholar]
- 30.Nedeltcheva AV, Kilkus JM, Imperial J, Kasza K, Schoeller DA, Penev PD. Sleep curtailment is accompanied by increased intake of calories from snacks. Am J Clin Nutr. 2009;89(1):126–33. doi: 10.3945/ajcn.2008.26574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Schmid SM, Hallschmid M, Jauch-Chara K, Born J, Schultes B. A single night of sleep deprivation increases ghrelin levels and feelings of hunger in normal-weight healthy men. J Sleep Res. 2008;17(3):331–4. doi: 10.1111/j.1365-2869.2008.00662.x. [DOI] [PubMed] [Google Scholar]
- 32.Knutson KL, Van Cauter E. Associations between sleep loss and increased risk of obesity and diabetes. Ann N Y Acad Sci. 2008;1129:287–304. doi: 10.1196/annals.1417.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Spiegel K, Leproult R, L’hermite-Baleriaux M, Copinschi G, Penev PD, Van Cauter E. Leptin levels are dependent on sleep duration: relationships with sympathovagal balance, carbohydrate regulation, cortisol, and thyrotropin. J Clin Endocrinol Metab. 2004;89(11):5762–71. doi: 10.1210/jc.2004-1003. [DOI] [PubMed] [Google Scholar]


