Abstract
Aim:
The aim was to study the structural sequelae and refractive outcome after laser treatment for Type 1 prethreshold retinopathy of prematurity (ROP) in Asian Indian eyes.
Materials and Methods:
A retrospective chart review of infants with Type 1 prethreshold ROP (defined according to the Early Treatment for Retinopathy of Prematurity study) undergoing laser treatment at a tertiary center between January 2004 and December 2008 was done. The 1-year outcome of infants was analyzed.
Results:
Sixty-nine eyes of 36 infants were included. The mean birth weight was 1121.69 ± 254.81 g and the gestational age was 28.99 ± 2.03 weeks. Sixty-five eyes (94.2%) had zone 2 and 4 (5.8%) had zone 1 disease. Forty-four (63.77%) eyes had stage 2 ROP with plus disease and 25 (36.23%) eyes had prethreshold (fewer than five contiguous or eight cumulative clock hours) stage 3 ROP with plus disease. None of the eyes developed retinal structural sequelae. On cycloplegic retinoscopy, 59.4% eyes had nonsignificant hyperopia [spherical equivalent (SE) ≤ 4 D], 14.5% eyes had no refractive error (SE 0 D), 24.7% eyes had low myopia (SE < 5 D), and 1.4% eyes had high myopia (SE > 5.0 D). Eyes developing myopia were associated with a greater number of clock hours of ROP, greater number of laser spots used, and a longer time to disease regression. Two infants (5.6%) had esotropia and one (2.8%) had exotropia.
Conclusion:
Asian Indian infants treated for Type 1 prethreshold ROP did not develop retinal structural sequelae. Myopia was seen in nearly one-fourth of the eyes.The risk factors for myopia were a greater number of clock hours of ROP, greater number of laser spots, and a longer time to regression of ROP.
Keywords: Myopia, prethreshold retinopathy of prematurity, retinopathy of prematurity
Retinopathy of prematurity (ROP) is a proliferative vascular retinopathy affecting infants with a young gestational age and low birth weight.[1,2] No standard guidelines for the treatment of ROP existed before the multicenter trial of Cryotherapy for Retinopathy of Prematurity (CRYO-ROP).[3] The CRYO-ROP study established that treatment with cryotherapy in threshold ROP reduced the incidence of unfavorable outcomes.[3,4] However, follow-up studies on threshold ROP treated successfully with either cryotherapy or laser photocoagulation reported a high incidence of structural sequelae and myopia.[5–13] The guidelines for the treatment of ROP have changed after the Early Treatment for Retinopathy of Prematurity (ETROP) study.[14] The ETROP study used a complex algorithm to identify patients with prethreshold ROP with a high risk for progression, who were enrolled into the trial. Based on the study results, the investigators defined Type 1 and Type 2 ROP from the cohort of prethreshold eyes and recommended treatment for Type 1 prethreshold ROP.[14] Follow-up studies from the ETROP trial report a significantly better structural outcome compared with conventionally managed eyes, with no greater risk of ocular complications.[15] The ETROP study enrolled infants with ≤ 1250 g birth weight. However, treatable ROP affects a significant proportion of infants with heavier birth weight (>1250 g birth weight) in developing Asian and middle-income group countries.[16–18] Little information exists about the structural sequelae and refractive outcome of laser-treated prethreshold eyes in these infants. The present study reports the structural sequelae and refractive outcome after laser photocoagulation in Asian Indian eyes with Type 1 prethreshold ROP.
Materials and Methods
We did a retrospective chart review of infants with Type 1 prethreshold ROP undergoing laser treatment at a tertiary center between January 2004 and December 2008. Type 1 prethreshold ROP was defined according to the ETROP study and included one of the following: (1) zone 1 stage 1 or 2 ROP with plus disease, (2) zone 1 stage 3 (fewer than five contiguous or eight cumulative clock hours) ROP with plus disease, (3) zone 2 stage 2 ROP with plus disease, and (4) zone 2 stage 3 (fewer than five contiguous or eight cumulative clock hours) ROP with plus disease.[14] Infants completing 1-year follow-up after laser treatment were included. A retrospective chart review was done to retrieve various parameters for these infants including the birth weight, period of gestation, postconceptional age at the time of treatment, zone of involvement, stage, and total clock hours of ROP.
All infants underwent confluent laser treatment (spots less than half burn width apart) with either a diode laser (IRIS Medical Oculight SL, 810-nm infrared laser; Iris Medical Inc., Mountain View, CA, USA) or 532-nm green laser (IRIS Medical Oculight GL, 532-nm green laser; Iris Medical Inc.). Treatment details were analyzed including the type of laser used, number of laser spots, number of laser sittings, and time required for regression of disease. The unfavorable outcome included (1) a posterior retinal fold involving the macula, (2) a retinal detachment involving the macula, or (3) retrolental tissue or mass obscuring the view of the posterior pole.[14]
The 1-year outcome of infants including refractive error, presence of strabismus or nystagmus, and retinal structural sequelae was retrieved. At the 1-year follow-up visit, the refractive error was assessed after cycloplegia using the 1% atropine ointment twice a day for 3 days. Spherical equivalent (SE) of retinoscopy findings were used for the present study. The refractive error was labeled as hyperopia (SE ≥ +0.25 D), no refractive error (SE = 0), and myopia (SE ≥ −0.25 D). At the same visit, a detailed retinal examination was carried out by an experienced retinal surgeon (MRD). The various retinal structural sequelae studied included narrowing of arcades, macular drag, disc drag, vitreal membranes, and presence of localized peripheral tractional detachment. Various factors including baseline infant characteristics, severity of disease, and time to regression were compared for eyes with myopia and no myopia. Student's t-test was used to compare independent linear variables and a chi-square test for nominal variables. P < 0.05 was considered statistically significant.
Results
Thirty-six infants met the inclusion criterion of the study. The mean birth weight of infants was 1121.69 ± 254.81 g (range 625–1600 g). Thirteen infants (36.11%) had a birth weight greater than 1250 g. The mean gestational age was 28.99 ± 2.03 weeks (range 26–33 weeks). The mean postconceptional age at the time of laser treatment was 36.93 ± 3.38 weeks (range 32-48 weeks). Of the 72 eyes of these 36 infants, 69 eyes were treated for Type 1 prethreshold ROP. Sixty-five (94.2%) eyes had zone 2 disease and 4 (5.8%) had zone 1 disease. Forty-four (63.77%) eyes had stage 2 ROP with plus disease and 25 (36.23%) eyes had prethreshold (fewer than five contiguous or eight cumulative clock hours) stage 3 ROP with plus disease. The mean number of total clock hours of ROP was 8.94 ± 2.73 clock hours (range 5–12). Of the 69 eyes, 66 eyes were treated with a diode laser and 3 eyes with a 532-nm green laser. The mean number of laser spots applied was 1492.97 ± 961.56. None of the eyes required retreatment. The mean time for the regression of ROP following treatment was 4.76 ± 2.45 weeks (range 2–16 weeks).
At 1-year follow-up, all eyes had a favorable outcome. None of the eyes showed structural posterior pole sequelae such as narrowing of arcades, disc drag, or macular drag. Peripheral ocular changes, namely, vitreous membranes and peripheral tractional retinal detachment were not observed in any eye.
Two infants (5.6%) had esotropia and one (2.8%) had exotropia. None of the three infants developing strabismus had anisometropic amblyopia, as the refractive eror was similar for both eyes. Rest all infants had a parallel visual axis. None of the infants had nystagmus.
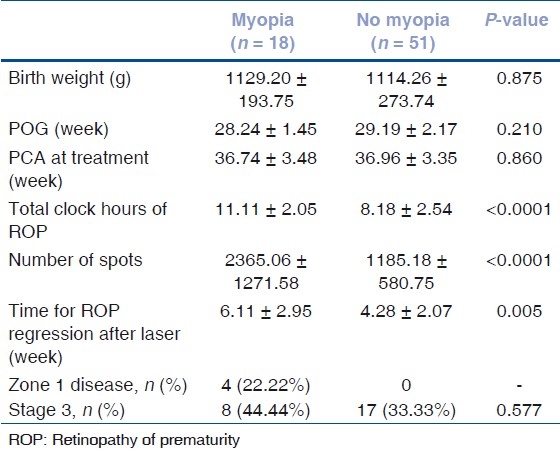
On cycloplegic retinoscopy, the median refractive error was 0.75 D (range −9.5 to +4 D). Forty-one (59.4%) eyes had nonsignificant hyperopia (range 0.25–4 D] and 10 (14.5%) eyes had no refractive error (SE 0 D). Seventeen (24.7%) eyes had low myopia (<5 D; range −0.25 D to −4.25 D). High myopia (>5.0 D) was seen in only one (1.4%) eye. This eye had 9.5 D myopia. Various factors including baseline infant characteristics, severity of disease, and time to regression were compared for eyes with myopia (n = 18) and no myopia (n = 51), despite a grossly unequal number of eyes in two groups. As compared to eyes with no myopia, eyes developing myopia had a significantly greater number of total clock hours of ROP, greater number of laser spots, and longer time required for the regression of ROP after laser [Table 1].
Table 1.
Comparison of putative risk factors: myopia vs. no myopia
Discussion
In the present study, nearly one-third of infants had a birth weight greater than 1251 g. Treatable ROP in infants with > 1250 g birth weight is not uncommon in the developing world.[16–18] In contrast, most reports from western centers and developed countries focus on ROP in extremely premature infants with < 1250 g birth weight.[13,14,18–20] The mean birth weight of infants in the present study was 1121.69 g which is much higher than 703 g for the ETROP cohort.[14] The mean gestational age of infants in the present study was 28.99 weeks which is higher than 25 weeks for the ETROP cohort.[14] As the infants treated in the present study were heavier and older, the disease profile and outcomes in these infants are likely to be different.
Laser photocoagulation has replaced cryotherapy as the standard treatment for ROP in most centers.[21] With the introduction of the the ETROP guidelines, treatment is being done much earlier than threshold for Type 1 prethreshold ROP.[14] None of the eyes in the present study showed structural posterior pole sequelae. The CRYO-ROP study reported a 44.4% rate of retinal residua in threshold eyes with a favorable outcome at 3.5 years after cryotherapy.[5] A recent study reported a high rate of structural posterior pole sequelae in eyes successfully treated by laser treatment for threshold ROP.[12] These changes included narrowing of arcades, disc drag, and macular drag in 53.26%, 18.48%, and 14.13% eyes, respectively.[12] Peripheral ocular changes, namely, vitreous membranes and peripheral tractional retinal detachment were not seen in any of the eyes in the present study. In comparison, vitreous membranes and peripheral tractional retinal detachment were reported in 65.21% and 16.3% eyes, respectively, for eyes treated at threshold.[12]
Only 3 (8.3%) of the 36 infants in the present study had strabismus. This rate of strabismus is lower than the 28.8% recently reported for eyes undergoing laser treatment at threshold.[13] The ETROP study reported strabismus in 22.8% of prethreshold eyes with a bilateral favorable outcome.[22] The low rate of strabismus in the present study may be attributed to short follow-up duration, predominant symmetric presentation, and regression without sequelae in both the eyes of the infants.
A significant proportion of eyes with ROP develop myopia, which needs appropriate correction and follow-up.[9–13,23–27] High rates of myopia have been reported for threshold ROP treated with either cryotherapy or laser.[9–13] Recent studies and subgroup analysis in the ETROP study report myopia in nearly 80% of threshold eyes treated with laser photocoagulation.[12,23] In the present study, 26.1% infants had myopia (SE > 0.25 D) and 1.4% had high myopia (SE > 5 D). One may be tempted to compare these rates with the ETROP study which reported that 64.5% of treated high-risk prethreshold infants had myopia (SE > 0.25 D) and 25.5% had high myopia (SE > 5 D) at 9 months.[23] However, a direct comparison with the ETROP study is not possible, given the fact that an entirely different subset of infants with a higher birth weight and gestational age are dealt with in the present study. Previous studies have reported that the prevalence of myopia is positively correlated with a lower birth weight and greater severity of ROP.[9,24,25,28] In the present study, 13 (36.11%) infants had a birth weight greater than 1251 g. Myopia rates in these infants are likely to be lower. The development of myopia is linked to cicatricial retinal changes and retinal residual of ROP.[9,23,25–27] In the present study, the regression of ROP was seen without structural retinal sequelae, which may also account for lower rates of myopia.
The present study is retrospective in nature. This induces inherent observational and inclusion bias. The study also lacks a control group. Another limitation of the study is a short follow-up duration. In summary, the study reports the outcome of Type 1 prethreshold ROP in a subset of infants who are heavier and older than those previously reported. Prethreshold ROP in these infants was milder and regressed without any retinal residua of ROP. Despite a normal anatomical outcome, a significant proportion (26.1%) of eyes develp myopia which needs to be followed up.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Palmer EA, Flynn JT, Hardy RJ, Phleps DL, Phillips CL, Schaffer DB, et al. Incidence and early course of retinopathy of Prematurity. Ophthalmology. 1991;11:1628–40. doi: 10.1016/s0161-6420(91)32074-8. [DOI] [PubMed] [Google Scholar]
- 2.Kinsey VE, Arnold HJ, Kalina RE, Stern L, Stahlman M, Odell G, et al. PaO2 levels and retrolental fibroplasia: A report of the cooperative study. Pediatrics. 1977;60:655–68. [PubMed] [Google Scholar]
- 3.Cryotherapy for Retinopathy of Prematurity Cooperative Group. Multicenter trial of cryotherapy for retinopathy of prematurity: Three month outcome. Arch Ophthalmol. 1990;108:195–204. doi: 10.1001/archopht.1990.01070040047029. [DOI] [PubMed] [Google Scholar]
- 4.Cryotherapy for Retinopathy of Prematurity Cooperative Group. Multicenter trial of cryotherapy for retinopathy of prematurity: One year outcome, structure and function. Arch Ophthalmol. 1990;108:1408–16. [PubMed] [Google Scholar]
- 5.Cryotherapy for Retinopathy of Prematurity Cooperative Group. Multicenter trial of cryotherapy for retinopathy of prematurity. 3 1/2-year outcome, structure and function. Arch Ophthalmol. 1993;111:339–44. [PubMed] [Google Scholar]
- 6.Cryotherapy for Retinopathy of Prematurity Cooperative Group. Multicenter trial of cryotherapy for retinopathy of prematurity: Ophthalmological outcomes at 10 years. Arch Ophthalmol. 2001;119:1110–33. doi: 10.1001/archopht.119.8.1110. [DOI] [PubMed] [Google Scholar]
- 7.McLoone E, O’Keefe M, McLoone S, Lanigan B. Long-term functional and structural outcomes of laser therapy for retinopathy of prematurity. Br J Ophthalmol. 2006;90:754–9. doi: 10.1136/bjo.2005.068304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ng EY, Connolly BP, McNamara JA, Regillo CD, Vander JF, Tasman W. A comparison of laser photocoagulation with cryotherapy for threshold retinopathy of prematurity at 10 years: Part 1. visual function and structural outcome. Ophthalmology. 2002;109:928–34. doi: 10.1016/s0161-6420(01)01017-x. [DOI] [PubMed] [Google Scholar]
- 9.Quinn GE, Dobson V, Kivlin J, Kaufman LM, Repka MX, Reynolds JD, et al. Prevalence of myopia between 3 months and 5 1/2 years in preterm infants with and without retinopathy of prematurity. Ophthalmology. 1998;105:1292–300. doi: 10.1016/s0161-6420(98)97036-1. [DOI] [PubMed] [Google Scholar]
- 10.Connolly BP, Ng EY, McNamara JA, Regillo CD, Vander JF, Tasman W. Comparison of laser photocoagulation with cryotherapy for threshold retinopathy of prematurity at 10 years: Part 2. refractive outcome. Ophthalmology. 2002;109:936–41. doi: 10.1016/s0161-6420(01)01015-6. [DOI] [PubMed] [Google Scholar]
- 11.McLoone EM, O’Keefe M, McLoone SF, Lanigan BM. Long-term refractive and biometric outcomes following diode laser therapy for retinopathy of prematurity. J AAPOS. 2006;10:454–9. doi: 10.1016/j.jaapos.2006.05.005. [DOI] [PubMed] [Google Scholar]
- 12.Dhawan A, Dogra M, Vinekar A, Gupta A, Dutta S. Structural sequelae and Refractive outcome after successful laser treatment for Threshold ROP. J Pediatr Ophthalmol Strabismus. 2008;45:356–61. doi: 10.3928/01913913-20081101-02. [DOI] [PubMed] [Google Scholar]
- 13.Axer-Siegel R, Maharshak I, Snir M, Friling R, Ehrlich R, Sherf I, et al. Diode Laser treatment of Retinopathy of prematurity.Anatomical and Refractive Outcomes. Retina. 2008;28:839–46. doi: 10.1097/IAE.0b013e318169faee. [DOI] [PubMed] [Google Scholar]
- 14.Early Treatment for Retinopathy of Prematurity Cooperative Group. Revised indications for the treatment of retinopathy of prematurity: Results of the early treatment for retinopathy of prematurity randomized trial. Arch Ophthalmol. 2003;121:1684–96. doi: 10.1001/archopht.121.12.1684. [DOI] [PubMed] [Google Scholar]
- 15.Early Treatment for Retinopathy of Prematurity Cooperative Group. Final Visual Acuity Results in the Early Treatment for Retinopathy of Prematurity Study. Arch Ophthalmol. 2010;128:663–71. doi: 10.1001/archophthalmol.2010.72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Vinekar A, Dogra MR, Sangtam T, Narang A, Gupta A. Retinopathy of prematurity in Asian Indian babies weighing greater than 1250 grams at birth: Ten year data from a tertiary care center in a developing country. Indian J Ophthalmol. 2007;55:331–6. doi: 10.4103/0301-4738.33817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chen Y, Li XX, Yin H, Gilbert C, Liang JH, Jiang YR, et al. Risk factors for retinopathy of prematurity in six neonatal intensive care units in Beijing, China. Br J Ophthalmol. 2008;92:326–30. doi: 10.1136/bjo.2007.131813. [DOI] [PubMed] [Google Scholar]
- 18.Gilbert C, Fielder A, Gordillo L, Quinn G, Semiglia R, Visintin P, et al. Characteristics of infants with severe retinopathy of prematurity in countries with low, moderate, and high levels of development: Implications for screening programs. Pediatrics. 2005;115:e518–25. doi: 10.1542/peds.2004-1180. [DOI] [PubMed] [Google Scholar]
- 19.Austeng D, Källen KB, Hellström A, Jakobsson PG, Johansson K, Tornqvist K, et al. Screening for retinopathy of prematurity in infants born before 27 weeks’ gestation in Sweden. Arch Ophthalmol. 2011;129:167–72. doi: 10.1001/archophthalmol.2010.346. [DOI] [PubMed] [Google Scholar]
- 20.Lad EM, Nguyen TC, Morton JM, Moshfeghi DM. Retinopathy of prematurity in the United States. Br J Ophthalmol. 2008;92:320–5. doi: 10.1136/bjo.2007.126201. [DOI] [PubMed] [Google Scholar]
- 21.Hurley BR, McNamara JA, Fineman MS, Ho AC, Tasman W, Kaiser RS, et al. Laser treatment for ROP: Evolution in treatment technique over 15 years. Retina. 2006;26:S16–7. doi: 10.1097/01.iae.0000244293.94251.20. [DOI] [PubMed] [Google Scholar]
- 22.Vanderveen DK, Coats DK, Dobson V, Fredrick D, Gordon RA, Hardy RJ, et al. Prevalence and course of strabismus in the first year of life for infants with prethreshold retinopathy of prematurity: Findings from the Early Treatment for Retinopathy of Prematurity Study. Arch Ophthalmol. 2006;124:766–73. doi: 10.1001/archopht.124.6.766. [DOI] [PubMed] [Google Scholar]
- 23.Early Treatment for Retinopathy of Prematurity Cooperative Group. Prevalence of myopia at 9 months in infants with highrisk prethreshold retinopathy of prematurity. Ophthalmology. 2005;112:1564–8. doi: 10.1016/j.ophtha.2005.03.025. [DOI] [PubMed] [Google Scholar]
- 24.O’Connor AR, Stephenson T, Johnson A, Tobin MJ, Moseley MJ, Ratib S, et al. Long-term ophthalmic outcome of low birth weight children with and without retinopathy of prematurity. Pediatrics. 2002;109:12–8. doi: 10.1542/peds.109.1.12. [DOI] [PubMed] [Google Scholar]
- 25.Quinn GE, Dobson V, Repka MX, Reynolds J, Kivlin J, Davis B, et al. Development of myopia in infants with birth weights less than 1251 grams. The cryotherapy for retinopathy of prematurity group. Ophthalmology. 1992;99:329–40. doi: 10.1016/s0161-6420(92)31968-2. [DOI] [PubMed] [Google Scholar]
- 26.Early Treatment for Retinopathy of Prematurity Cooperative Group. Prevalence of myopia and high myopia in the early treatment for retinopathy of prematurity study. Ophthalmology. 2008;115:1058–64. doi: 10.1016/j.ophtha.2007.07.028. [DOI] [PubMed] [Google Scholar]
- 27.Choi MY, Park IK, Yu YS. Long term refractive outcome in eyes of preterm infants with and without retinopathy of prematurity; comparison of keratometric value, axial length, anterior chamber depth, and lens thickness. Br J Ophthalmol. 2000;84:138–43. doi: 10.1136/bjo.84.2.138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Fledelius HC. Myopia of prematurity, clinical patterns.A follow-up of Danish children now aged 3-9 years. Acta Ophthalmol Scand. 1995;73:402–6. doi: 10.1111/j.1600-0420.1995.tb00297.x. [DOI] [PubMed] [Google Scholar]


