Abstract
Purpose:
To report the management outcomes of diplopia in patients with blowout fracture.
Materials and Methods:
Data for 39 patients with diplopia due to orbital blowout fracture were analyzed retrospectively. The inferior wall alone was involved in 22 (56.4%) patients, medial wall alone was involved in 14 (35.8%) patients, and the medial and inferior walls were involved in three (7.6%) patients. Each fracture was reconstructed with a Medpore® implant. Strabismus surgery or prism correction was performed in required patients for the management of persistent diplopia. Mean postoperative follow up was 6.5 months.
Results:
Twenty-three (58.9%) patients with diplopia underwent surgical repair of blowout fracture. Diplopia was eliminated in 17 (73.9%) patients following orbital wall surgery. Of the 23 patients, three (7.6%) patients required prism glasses and another three (7.6%) patients required strabismus surgery for persistent diplopia. In four (10.2%) patients, strabismus surgery was performed without fracture repair. Twelve patients (30.7%) with negative forced duction test results were followed up without surgery.
Conclusions:
In our study, diplopia resolved in 30.7% of patients without surgery and 69.2% of patients with diplopia required surgical intervention. Primary gaze diplopia was eliminated in 73.9% of patients through orbital wall repair. The most frequently employed secondary surgery was adjustable inferior rectus recession and <17.8% of patients required additional strabismus surgery.
Keywords: Blowout, diplopia, prism, strabismus
Blowout fractures are repaired based on the clinical symptoms and signs of the patients, although reconstruction may not completely resolve the cosmetic and functional problems. Recognized sequelae of orbital blowout fractures include enophthalmos, diplopia from extraocular muscle dysfunction, infraorbital nerve anesthesia, disfiguring facial contour, and tearing due to the obstruction of the nasolacrimal duct.[1–3] Treatment options are also based on the nature of the fracture, severe displacement of periorbital tissues, and the experience of the surgeon. Diplopia and enophthalmos are additional indications for surgery.[4]
Management of diplopia in association with blowout fracture is usually possible with orbital wall repair, strabismus surgery, the use of prisms, and medical treatment.[5] The aim of this study was to illustrate our surgical experience in patients with diplopia due to blowout fractures.
Materials and Methods
This study was based on the retrospective analysis of 39 patients with orbital computerized tomography (CT) indicated blowout fracture who had presented to Gulhane Military Medicine Academy Ophthalmology Department, between January 1994 and June 2010. Patients with diplopia who had at least 2 months of follow up were included in the study group. Patients with concomitant orbital fractures involving the orbital rim (n = 8), associated ocular injury with visual loss that prevented the perception of diplopia (n = 5), and asymptomatic patients with small nondisplaced fractures (n = 16) were not included in the study. The study protocol was approved by the Medical Ethical Committee, with consideration of the principles proposed by the Helsinki Declaration. The average follow-up was 6.5 months (2-20 months).
Data regarding patient demographics, signs and symptoms, cause of injury, nature of fracture, surgical outcome and complications were collected. Complete ophthalmic examinations including ocular motility and preoperative orbital CT scans were routinely employed in all cases. Hess screens, binocular single visual fields, forced duction and forced generation tests were analyzed on initial visits and on follow-up visits when warranted. The immediate indication for orbital wall repair included potentiation of the oculocardiac reflex. Indication for surgery within 2 weeks included extraocular muscle or perimuscular soft tissue entrapment, persistent diplopia, enophthalmos (> 2 mm), and large orbital wall defect extending over more than one-half of the floor, as revealed by CT scan. Patients operated upon after 14 to 20 days of trauma were denoted as delayed admission to the hospital.
Orbital floor fractures were repaired under general anesthesia with porous polyethylene (Medpore®, 0.85 mm, Porex Surgical Products, Newnan, GA) implants through a subciliary incision or transconjunctival incision. The strabismus surgery indication included persistent diplopia due to ocular motility restriction with or without orbital wall repair. Strabismus surgery for extraocular motility restrictions included the faden operation and recession procedures, with or without adjustable sutures. Early postoperative and late complications including infection, hematoma, eyelid malposition, enophthalmos, and migration or extrusion of the implant were evaluated.
Results
The age of patients ranged from 5 to 65 years, with a mean age of 23.3 years. There were 33 (84.6%) male and 6 (15.3%) female patients. Signs and symptoms of patients are shown in Table 1. The cause of blowout fracture was motor vehicle accident in 12 (30.7%) patients, assault in 10 (25.6%) patients, work-related incidents in eight (20.5%) cases, sports injuries in six (15.3%) cases, and falls in three (7.6%) cases. The inferior wall alone was involved in 22 (56.4%) cases, the medial wall alone was involved in 14 (35.8%) cases, and the medial and inferior walls were involved in three (7.6%) cases [Table 2]. Enophthalmos greater than 2 mm was present in four (10.2%) patients preoperatively and eliminated in all patients, except for one (2.5%) postoperatively.
Table 1.
Preoperative and postoperative (1 year) signs and symptoms of patients
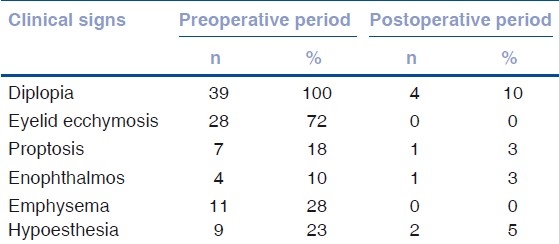
Table 2.
Affected wall of orbita

The mean time between trauma and orbital wall repair was 8.4 days (range, 2 to 20 days) [Table 3]. Twenty-three (58.9%) patients underwent orbital wall repair. One patient who was five years old with nonresolving pain, nausea, and vomiting underwent surgery on the second day of trauma, with CT evidence of inferior rectus muscle entrapment. Early orbital wall repair of blowout fractures was performed within 2 weeks in 16 patients with symptomatic diplopia with positive forced duction and CT scan documentation of inferior rectus muscle or perimuscular soft-tissue entrapment. In seven patients with delayed admission to the hospital, orbital wall repair was performed after 14 to 20 days had elapsed since the injury. Postoperative primary gaze diplopia was present in four (25%) patients from the early repair group and in two (28.5%) patients in the delayed group. There was no significant difference in postoperative primary gaze diplopia when comparing early vs delayed repair.
Table 3.
Time interval between trauma and orbital wall repair

Seven (17.8%) patients underwent strabismus surgery. The mean time between trauma and strabismus surgery was 10.5 months (range, 3 to 28 months). Three (7.6%) patients required strabismus surgery to correct persistent diplopia, although they had previously undergone orbital wall reconstruction. In four (10.2%) patients, strabismus surgery was performed without fracture repair due to history of trauma 28 months prior. The mean angle of deviation was 14 prism diopters (Δ) (range, 10 to 18Δ) before strabismus surgery. Five (12.8%) patients underwent inferior rectus muscle recession involving adjustable sutures [Fig. 1a, b]. One (2.5%) patient had medial rectus muscle recession, and one (2.5%) patient underwent the faden operation. At the final follow-up, mean deviation was 3.6Δ (range, 0 to 8Δ). Three (7.6%) patients who had previously undergone fracture repair required prism glasses to correct persistent diplopia.
Figure 1.

(a) Right hypotropia due to inferior orbital wall fracture; (b) Third day postoperatively, recession of the inferior rectus with an adjustable suture after repair of the inferior orbital wall fracture
Twelve (30.7%) patients with negative forced duction test results were followed up without surgery [Fig. 2a, b], among these patients one (2.5%) required prisms. In two (5.1%) of these patients, CT scan revealed orbital air, and diplopia resolved with complete resolution of emphysema within two days of trauma.
Figure 2.
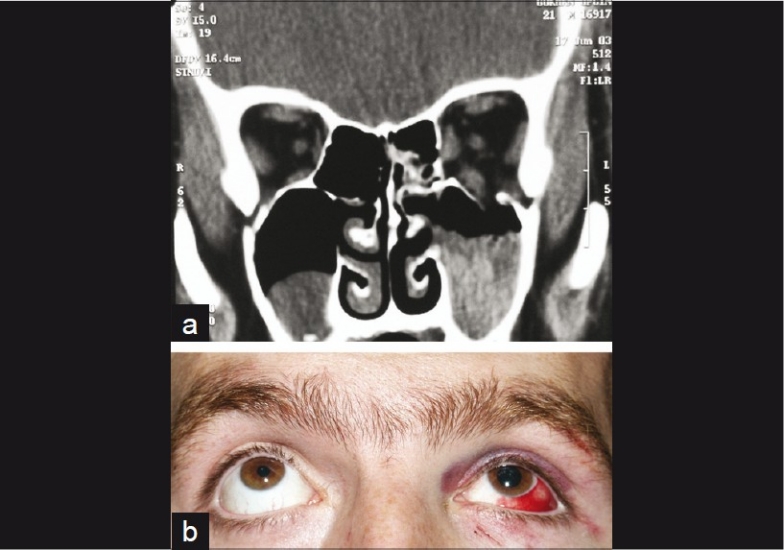
(a) Coronal CT scan of the patient showing the left orbital floor fracture with negative forced duction test results; (b) Elevation is within normal limits in the left eye. The patient was followed up without surgery
Discussion
Diplopia and ocular motility disorders are common complications of blowout fractures. Limited ductions occur in the field of the antagonist muscle due to restriction of the entrapped muscle.[6] Ocular motility disturbances are caused not only by the entrapment of rectus muscles and soft tissues, but also by muscle edema, muscle fibrosis, hemorrhage, and motor nerve palsies.[3] Diplopia in the presence of orbital wall fracture is one of the main indications for surgical intervention.[7] However, the degree of diplopia needed to perform the surgery is not clear. Horizontal diplopia within 25 to 30Δ of primary gaze is usually not tolerated well by patients.[5]
In our study, diplopia was present in 57.3% of all patients with blowout fractures. Reported incidence rates (36 to 86%) of diplopia in patients with blowout fractures vary widely.[8,9] Qurainy et al. reported a 58% incidence of diplopia, which is in agreement with our results.[10] To prevent fat atrophy and scarring of the orbital fat to the maxillary antrum, surgical repair should be performed within 2 weeks.[1] Matteini et al. performed early surgery within 3 days in children with diplopia and, usually, within 7 days in adults with diplopia.[7] The decision to proceed with surgery should be based on the patient's symptoms, clinical findings, and informed consent about the risks and benefits of surgical intervention. Orbital soft-tissue entrapment may generate the oculocardiac reflex (bradycardia, heart block, nausea, vomiting, and syncope), warranting immediate surgical intervention.[11] In this study, one patient who was five years old underwent immediate surgery on the second day due to nonresolving pain, nausea, and vomiting.
In the present study, 23 (58.9%) patients underwent orbital wall repair. Postoperative primary gaze diplopia was present in four patients from the early repair group and in two patients from the delayed group. In three of 23 patients, additional strabismus surgery was performed, and in another three patients, prism glasses were required. Strabismus surgery was performed in seven (17.8%) patients. In three of seven patients, strabismus surgery was performed after orbital wall repair. In four patients with a history of trauma, strabismus surgery was performed without orbital wall repair. Although forced duction test results were negative and force generation test results were positive, gaze restriction toward the field of action of the muscle continued in two of our patients after entrapment repair of orbital wall fractures. In these two patients, persistent diplopia may have resulted from a flap tear of the rectus muscle. Flap tear muscle injury is a common cause of posttraumatic diplopia, and the best results were obtained after early repair.[12] Patients with an angle of deviation greater than 6Δ usually complain of diplopia and require treatment.[2] Diplopia in patients with slight motility disorders responded well to prisms.[13] Four of our patients who had residual diplopia in primary gaze were treated with prism glasses.
After orbital injury, edema of the orbital tissues often obscures enophthalmos and orbital wall fractures. In our study, one of the patients who had preoperative enophthalmos continued to experience the condition postoperatively. Edema and hemorrhage may cause proptosis of the involved orbit. Two-week observation has been recommended for the resolution of proptosis, if urgent surgical indications do not exist.[14] In our study, proptosis improved in all patients, except in one patient who was still experiencing proptosis postoperatively. Potential surgical complications of blowout fracture including blindness, infection of implanted material, implant migration, postoperative mydriasis, epiphora, and worsening of diplopia have been reported.[1] We have not experienced any of these severe complications.
In this study, 30.7% of patients with diplopia did not require surgery and 69.2% of patients with diplopia required surgical intervention. Although orbital wall repair surgery was required in 58.9% of patients, primary gaze diplopia was eliminated in 73.9% of patients with no complication related to use of the Medpore® implant. Additional strabismus surgery was required in 17.8% of patients and the most frequently employed secondary surgery was adjustable inferior rectus recession.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Burnstine MA. Clinical recommendations for repair of isolated orbital floor fractures. Ophthalmology. 2002;109:1207–13. doi: 10.1016/s0161-6420(02)01057-6. [DOI] [PubMed] [Google Scholar]
- 2.Gilhotra JS, McNab AA, McKelvie P, O’Donnell BA. Late orbital haemorrhage around orbital alloplastic orbital floor implants: A case series and review. Clin Exp Ophthalmol. 2002;30:352–5. doi: 10.1046/j.1442-9071.2002.t01-1-00555.x. [DOI] [PubMed] [Google Scholar]
- 3.Helveston EM. The relationship of extraocular muscle problems to orbital floor fractures: Early and late management. Trans Sect Ophthalmol Am Acad Ophthalmol Otolaryngol. 1977;83:660–2. [PubMed] [Google Scholar]
- 4.Ploder O, Oeckher M, Klug C, Voracek M, Wagner A, Burggasser G, et al. Follow-up study of treatment of orbital floor fractures: Relation of clinical data and software-based CT-analysis. Int J Oral Maxillofac Surg. 2003;32:257–62. doi: 10.1054/ijom.2003.0366. [DOI] [PubMed] [Google Scholar]
- 5.Segrest DR, Dortzbach RK. Medial orbital wall fractures: Complications and management. Ophthal Plast Reconstr Surg. 1989;5:75–80. doi: 10.1097/00002341-198906000-00001. [DOI] [PubMed] [Google Scholar]
- 6.Kushner BJ. Paresis and restriction of the inferior rectus muscle after orbital floor fracture. Am J Ophthalmol. 1982;94:81–6. doi: 10.1016/0002-9394(82)90195-7. [DOI] [PubMed] [Google Scholar]
- 7.Matteini C, Renzi G, Becelli R, Belli E, Iannetti G. Surgical timing in orbital fracture treatment: Experience with 108 consecutive cases. J Craniofac Surg. 2004;15:145–50. doi: 10.1097/00001665-200401000-00035. [DOI] [PubMed] [Google Scholar]
- 8.Leibsohn J, Burton TC, Scott WE. Orbital floor fractures: A retrospective study. Ann Ophthalmol. 1976;8:1057–62. [PubMed] [Google Scholar]
- 9.Biesman BS, Hornblass A, Lisman R, Kazlas M. Diplopia after surgical repair of orbital floor fractures. Ophthal Plast Reconstr Surg. 1996;12:9–17. doi: 10.1097/00002341-199603000-00002. [DOI] [PubMed] [Google Scholar]
- 10.al-Qurainy IA, Stassen LF, Dutton GN, Moos KF, el-Attar A. Diplopia following midfacial fractures. Br J Oral Maxillofac Surg. 1991;29:302–7. doi: 10.1016/0266-4356(91)90115-l. [DOI] [PubMed] [Google Scholar]
- 11.Burnstine MA. Clinical recommendations for repair of orbital facial fractures. Curr Opin Ophthalmol. 2003;14:236–40. doi: 10.1097/00055735-200310000-00002. [DOI] [PubMed] [Google Scholar]
- 12.Ludwig IH, Brown MS. Flap tear of rectus muscles: An underlying cause of strabismus after orbital trauma. Ophthal Plast Reconstr Surg. 2002;18:443–9. doi: 10.1097/01.IOP.0000034567.31754.7C. [DOI] [PubMed] [Google Scholar]
- 13.Buchel P, Rahal A, Seto I, Iizuka T. Reconstruction of orbital floor fracture with polyglactin 910/polydioxanon patch (ethisorb): A retrospective study. J Oral Maxillofac Surg. 2005;63:646–50. doi: 10.1016/j.joms.2004.11.013. [DOI] [PubMed] [Google Scholar]
- 14.Hawes MJ, Dortzbach RK. Surgery on orbital floor fractures: Influence of time of repair and fracture size. Ophthalmology. 1983;90:1066–70. doi: 10.1016/s0161-6420(83)80049-9. [DOI] [PubMed] [Google Scholar]


