Abstract
Purpose:
To evaluate the factors influencing final visual outcome after surgical repair of open globe injuries.
Materials and Methods:
The study was carried out at a tertiary referral eye care center in Central India. In this retrospective study, case records of 669 patients with open globe injuries were analyzed. Different preoperative variables were correlated with the final visual outcome. Exclusion criteria were patients with less than four months follow up, previous ocular surgery, presence of intraocular foreign body or endophthalmitis at the time of presentation. Using statistical tests, the prognostic factors for vision outcome following surgical repair of open globe injuries were studied.
Results:
Based on the Spearman's Rho correlation analysis, following factors were found to be significantly associated with the final visual acuity at univariate level: age (P<0.001), preoperative visual acuity (P=0.045), mode of injury (P=0.001), and time lag between the injury and surgery (P=0.003). None of the other clinical factors have statistically significant correlation with final visual acuity. On multivariate analysis using binary logistic regression, only age, mode of injury and the time lag between injury and surgery achieved statistically significant results.
Conclusion:
In the current study, elapsed time between the injury and surgery, age of the patient, preoperative visual acuity and mode of injury were found to be adversely affecting the final visual outcome. Recognizing these factors prior to surgical intervention or intraoperatively can help the surgeon in evidence-based counseling of the trauma victim and family.
Keywords: Ocular trauma, open globe injury, preoperative visual acuity, prognostic factors, relative afferent pupillary defect
Ocular trauma is one of the leading causes of ocular morbidity in children and young adults.[1] Successful surgical repair of open globe injury and subsequent visual rehabilitation is a topic of great significance and challenge to the practicing ophthalmologists.[2] One of the important components in the management of open globe injury is counseling of the trauma victim and his family.[2] Even though, with the advent of new modalities and improved technology, the management of penetrating ocular injuries has changed,[2] we need to prognosticate any patient with ocular trauma before and even after the repair of open globe injury. To predict the vision outcome in ocular trauma patients, there have been numerous studies till date.[3–17] Based on literature review, the factors likely to predict outcome after open globe injury are mechanism or type of injury, preoperative visual acuity (VA), time lag between injury and surgery, relative afferent pupillary defect (RAPD), size and location of the wound. International classification of ocular trauma is based on some of the variables affecting the final visual outcome.[18] Besides the above listed variables, other parameters that can predict vision outcome are retinal detachment, uveal or retinal tissue prolapse, vitreous hemorrhage, lens damage, hyphema and number of operative procedures.[3–17]
However, there is limited literature for outcome of open globe injuries in Indian patients.[19–21] The present study is aimed at evaluating the factors affecting the final vision outcome in patients with open globe injuries at a tertiary referral eye care center in central India.
Materials and Methods
We retrospectively reviewed the case records of patients who underwent surgical repair of open globe injury at a tertiary referral eye care center in central India from April 2003 to January 2008. The center is located in a relatively semi urban location in central India. The center receives high volume of emergency patients out of which significant proportion of patients present with history of ocular trauma and open globe injury. Most of the open globe injuries were secondary to work-related ocular injuries.
Cases with surgical repair done before presentation to our institute [Graph 1, Fig. 1a and b], with poor visual acuity of the injured eye prior to injury, with associated endophthalmitis, with intraocular foreign body and with follow up of less than four months post surgery were excluded from the study. Similarly, cases operated by residents or inexperienced surgeons were not included in the study. Case records of six hundred and sixty nine eyes of open globe injuries operated from April 2003 to January 2008 were retrospectively analyzed. All the patients in this study were operated by the surgeons experienced in ocular trauma or vitreoretina or cornea or oculoplasty. The factors studied were age and sex of the patient, initial VA after injury, presence or absence of RAPD, details of the object causing the injury, duration between injury and the surgery, total extent of the wound, wound involving limbus or not, wound involving visual axis, extent of wound beyond recti insertion which was noted intraoperatively, vitreous loss, iris prolapse, vitreous hemorrhage, presence or absence of retinal detachment, evidence of infection on or around the wound, presence or absence of hyphema and lens status.
Graph 1.
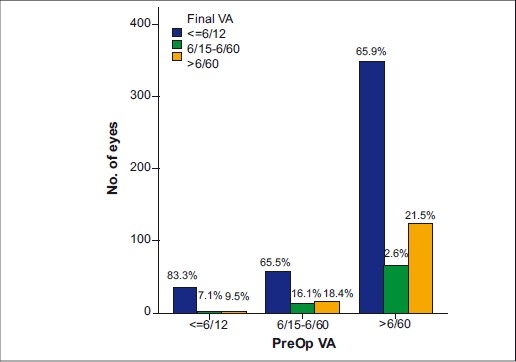
Distribution of preoperative in comparision visual acuity
Figure 1.
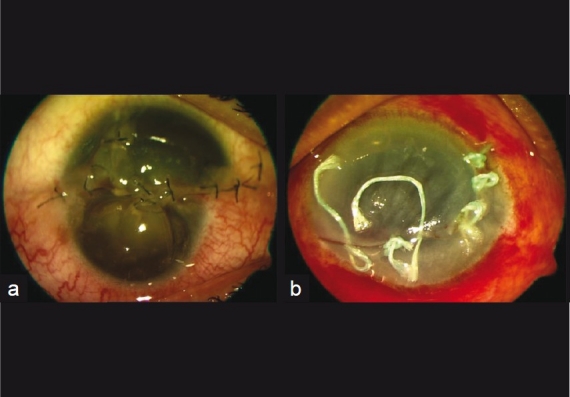
Anterior segment photograph of the patient with (a) complex corneal laceration repaired elsewhere (b) corneal laceration who underwent primary repair by another eye specialist
Details of all the surgical steps were recorded. Follow up data for duration of follow up, visual acuity at four months follow up and anatomical status of the eye were recorded. Anatomical status of the eye indicating corneal scar, phthisis bulbi, pseudophakia or traumatic cataract, retinal detachment, and glaucoma was recorded in the study eyes.
For statistical analysis, the initial visual acuity VA after injury and the VA at final follow up were grouped in three categories: Group 1 – VA ≤ 20/40, Group 2- VA: 20/50-20/200 and Group 3 – VA >20/200. The relationship between different preoperative variables and the final VA were investigated using correlation analysis (Spearman's rho) for univariate analysis. Furthermore, binary logistic regression was performed for the purpose of multivariate analysis, in which final VA were grouped into only two categories: ≤20/200 and >20/200. Whenever necessary, the association between factors and final VA was considered statistically significant if P ≤ 0.05.
Results
Of the 669 patients, 567 (84.8%) were males and 102 (15.2%) were females. The average age was 18 years, with a median of 13 years (range: 2-57 years). The average time lag between the injury and surgery was 4 days, with a median of 2 days (range: 3 h-90 days). Two hundred and forty six (36.8%) patients had only one surgery, while 390 (58.8%) had two and the remaining 33 (4.9%) patients had three surgeries. Average follow-up was 7 months, with a median of 6 months (range: 4-24 months).
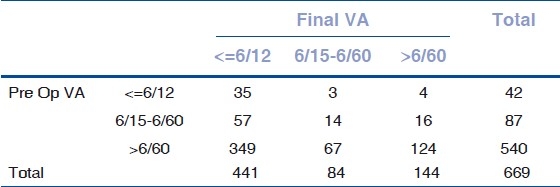
There were 42 (6.3%) patients having a preoperative VA better than 20/40, 87 (13.0%) eyes were within 20/50-20/200 and the remaining 540 (80.7%) had a preoperative VA worse than 20/200. After surgery, at four months follow up, 441 (65.9%) patients achieved better than 20/40 VA, 84 had VA between 20/50-20/200 and the other 144 (21.5%) were worse than 20/200. The detailed distribution of final VA achieved by patients can be found in Table 1.
Table 1.
Distribution of preoperative factors with postoperative final visual acuity
Of all the patients, 478 (71.4%) had a penetrating trauma while the other 191 (28.6%) had a blunt injury. According to the extent of wound, 468 patients (70.0%) had corneal wound [Fig. 2], 66 (9.9%) had scleral wound [Fig. 3] and the remaining 135 (20.2%) had corneoscleral wound [Fig. 4]. Lid laceration [Fig. 5] was associated in 27 eyes (4.0%). RAPD was noted in 120 eyes (17.9%). Hyphema [Fig. 6] was associated in 243 eyes (36.3%). Lens was found to be cataractous with or without rupture of anterior capsule [Figs. 7 and 8] in 477 eyes (71.3%), and was absent inside the eye secondary to traumatic expulsion of the lens in 24 eyes (3.6%). Vitreous loss was noted in 138 eyes (20.6%) while vitreous hemorrhage was noted in 204 eyes (30.5%). Wound was seen extending to the insertion of rectus muscle (intraoperative finding) in 96 eyes (14.3%). Retinal detachment was present in 93 eyes (13.9%). Infection of the corneal wound edges without endopthalmitis was noted in 78 eyes (11.7%). Details of the frequency statistics are given in Table 2. Preoperative and postoperative clinical photographs of few patients recruited in the study are shown in Fig. 9a and b, Fig. 10a and b and Fig. 11a and b.
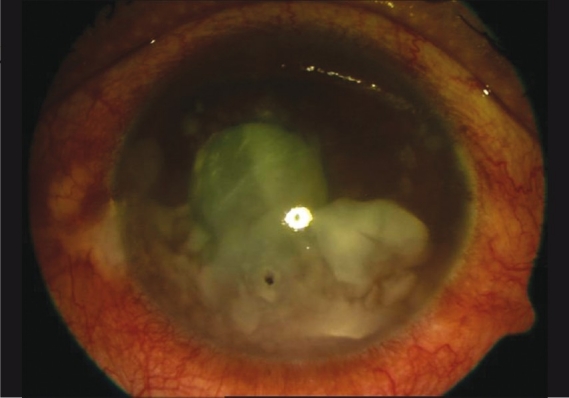
Figure 2.
Patient with full thickness corneal laceration involving visual axis and traumatic cataract
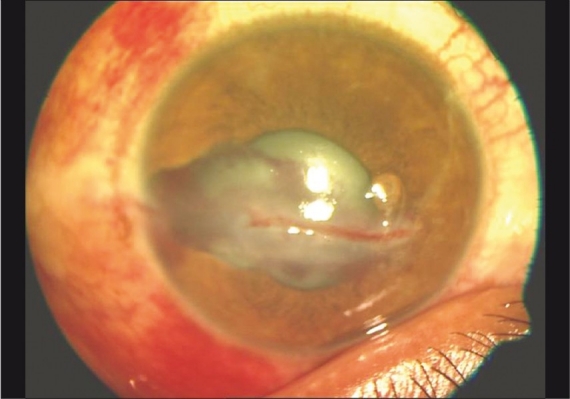
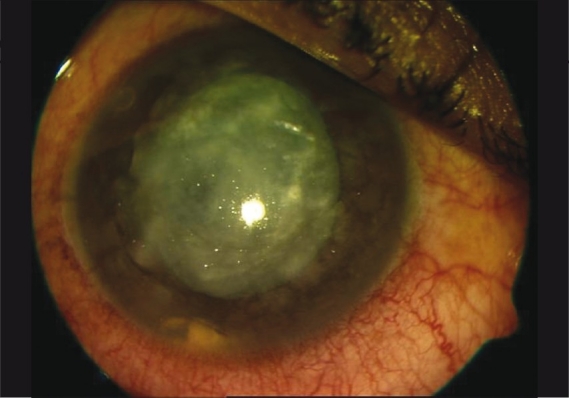
Figure 3.
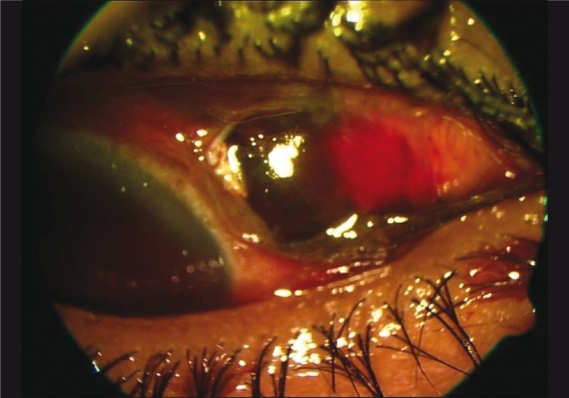
External photograph showing full thickness scleral laceration with uveal tissue prolapse
Figure 4.
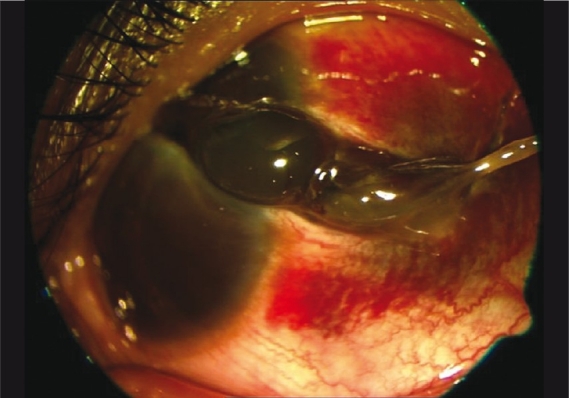
External photograph of a patient with extensive corneoscleral laceration
Figure 5.
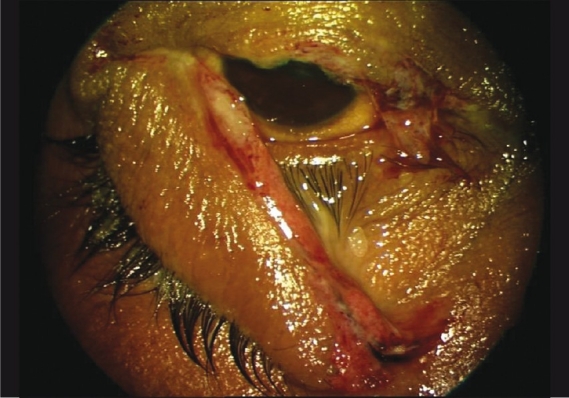
Photograph showing partial avulsion of upper lid
Figure 6.
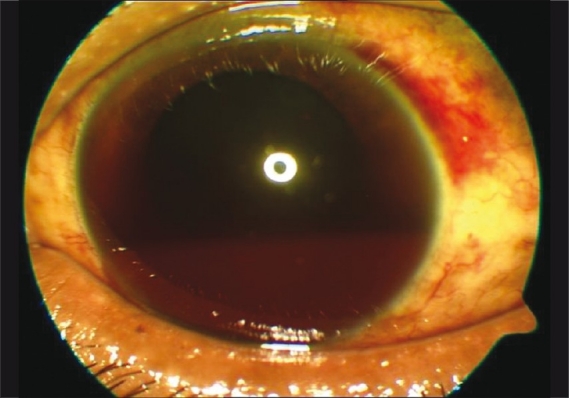
Presence of half chamber hyphaema with occult scleral dehiscence in superotemporal quadrant (not seen in this particular image)
Figure 7.
Presence of ruptured traumatic cataract with small corneal laceration
Figure 8.
Presence of ruptured traumatic cataract with foreign body in anterior chamber with small corneal laceration
Table 2.
Distribution statistics for preoperative and postoperative factors
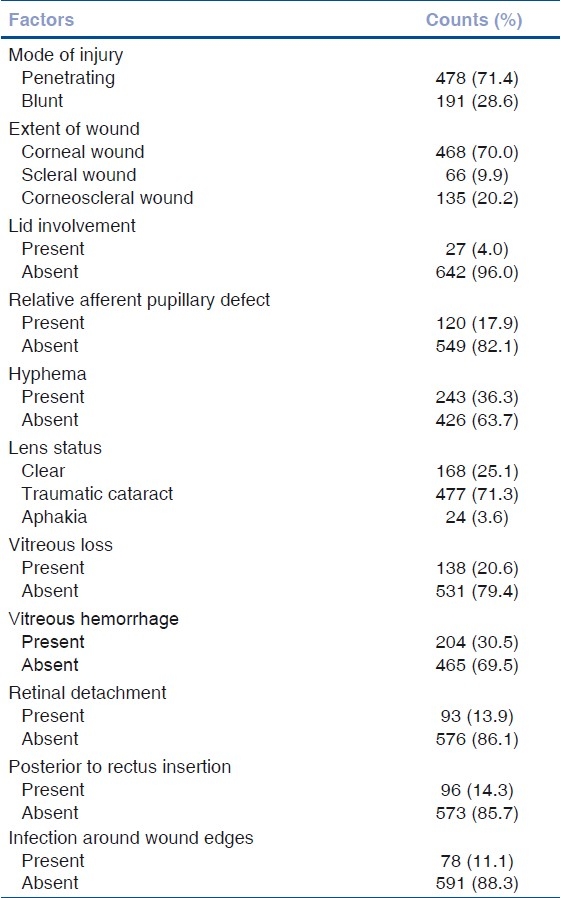
Figure 9.

(a) Clinical photograph of the patient with corneal laceration with eye lash in the corneal wound (b) Postoperative clinical photograph of the patient with corneal laceration repair
Figure 10.
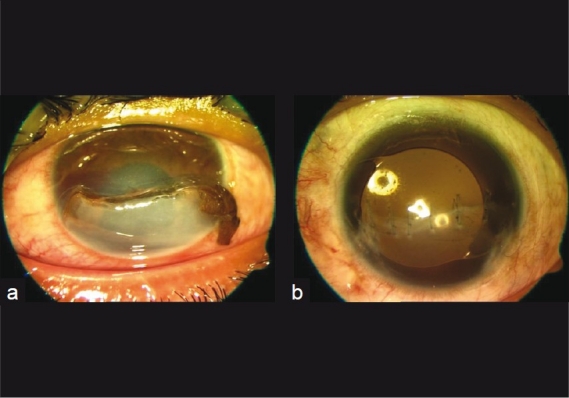
(a) Preoperative clinical photograph of the patient with full thickness corneal laceration and traumatic cataract with corneal edema of the inferior half of the cornea, (b) Post operative clinical photograph of the patient following corneal laceration repair with cataract extraction and scleral fixated intraocular lens
Figure 11.

(a) Clinical image of the patient with corneal laceration with traumatic cataract (b) Postoperative clinical photograph of the patient with repaired corneal laceration with presence of post operative traumatic endophthalmitis
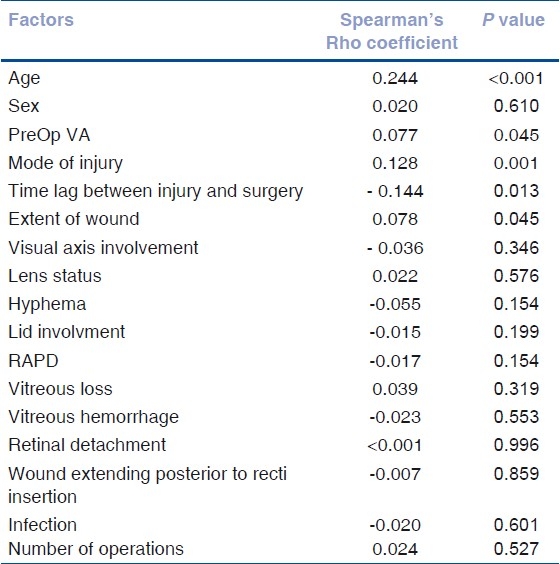
Based on the Spearman's Rho correlation analysis, the following factors were found to be significantly associated with the final VA at the univariate level: age (P<0.001), preoperative VA (P=0.045), mode of injury (P=0.001) and time lag between the injury and surgery (P=0.003). None of the other clinical factors have statistically significant correlation with final VA according to our study results. The details can be found in Table 3.
Table 3.
Univariate analysis of different factors affecting final vision outcome
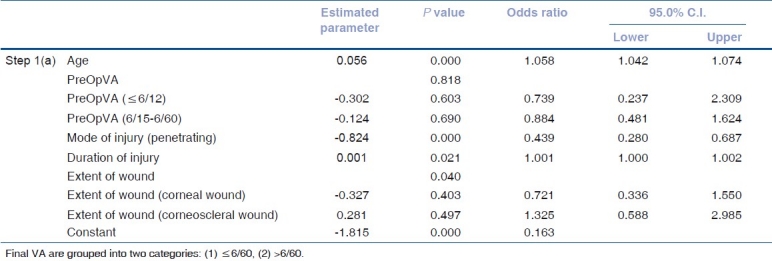
Furthermore, all the factors found significant in univariate analysis were included in the multivariate analysis using binary logistic regression to further evaluate their associations with final VA. The results are given in Table 4. It can be seen that only age, mode of injury and the time lag between injury and surgery achieved statistically significant results.
Table 4.
Multivariate analysis of factors affecting final vision outcome
Discussion
Numerous studies have been done in the past to co-relate the final visual outcome with the several preoperative factors related to ocular injury. Factors that have been found to correlate significantly with visual outcome include age,[11] type or mechanism of injury,[3,6,8,19–21] initial VA,[3–17,19–21] presence of RAPD,[11,15,19–21] extent of wound and size of open-globe injury,[3–17,19,20] location of open globe wound,[3,8,9,19–21] lens damage,[3–17,19–21] hyphema,[4,19,21] vitreous hemorrhage,[3,4,8,9,19,21] retinal detachment,[7] and presence and type of intraocular foreign body.[17]
We analyzed the data regarding the preoperative factors affecting final vision outcome following surgical repair of open globe injury. We attempted to create a homogenous group of patients with open globe injuries by excluding cases with intraocular foreign body or endophthalmitis at presentation as both of them can affect the visual outcome.[2] Likewise, the cases done by residents and inexperienced surgeons were excluded from the study because unfamiliarity and poor surgical technique can adversely affect the outcome. Endophthalmitis by itself is very strong predictor of visual outcome; hence, it was excluded as the current series was undertaken to find out factors besides endophthalmitis which can affect the final vision outcome. Intraocular foreign body also on its nature and time of retention inside the eye since injury can skew the final vision outcome; hence patients with intraocular foreign bodies were also not taken into the current series.
The analysis of features of the injured eye with a favorable or unfavorable visual outcome was done in patients from central India wherein there are significant industrial eye injuries and also high incidence of field or agriculture related eye injuries. By clustering the study group to one particular segment also highlights the burden of ocular trauma in a small segment of the society itself. Also, in the current series, the majority of patients were in younger age group with a high percentage of them being work-related eye injuries. Being work-related eye injuries, it suggests to the central authorities to take preventive measures and to enforce eye protection at work place to prevent injuries. In most population-based studies till date,[6,15] there is a strong preponderance for open globe injuries to affect males, which we have confirmed from the current study. This may reflect the more aggressive characteristics of male behavior and to a lesser extent the involvement of men in higher risk working activities. Based on statistical analysis, final vision outcome was affected by increasing age of the patient. In the present study, statistical methods revealed visual acuity was 1.058 times likely to be poorer when patient ages by an additional one year.
VA at the time of presentation did not statistically affect the final visual outcome as revealed after multivariate analysis of the factors found statistically significant in univariate analysis. In other studies, VA was found to be significantly affecting the final visual outcome.[3–17] Good vision outcome despite a poor preoperative VA could be because of preoperative factors such as hyphema, traumatic cataract, vitreous hemorrhage and retinal detachment, which can be treated surgically with good outcome. Based on the current study, in open globe injuries without evidence of endophthalmitis at initial presentation, only poor VA at presentation after injury, in isolation need not be correlated with poorer visual outcome.
In the current study, based on mode of injury, blunt injury was shown to be 2.278 times more likely to have poor final VA compared to penetrating injury. This is in concurrence with other studies where the authors have shown injury by sharp objects are correlated with a more favourable visual outcome when compared to blunt impact mechanisms.[8,15] Rahman et al, showed a statistically significant improved visual outcome in patients suffering sharp injuries compared to blunt injuries (P = 0.004).[15]
Blunt injury can affect the internal structures of the eye, and similarly, optic nerve and extent of the wound can be posterior to recti insertion resulting in poorer final vision outcome.
Time lag between injury and surgery also adversely affects the final vision outcome though not very strongly significant as per statistical tests. Increase in the time lag of one day from injury to surgery results in 1.001 times more likelihood of poor final visual acuity. Issac et al, demonstrated a 1.16 fold increased chance of worse visual prognosis with each day of delay of surgery.[5]
Current study though involves a significant number of patients from a single centre, it is limited by the retrospective data collection and analysis and focuses on only one segment of the society in central India. A limited follow up in the current study is also one of the drawbacks of this study. Future prospective multicentric study is suggested to look at the factors affecting outcome in patients with open globe injuries.
In this retrospective review, we have shown several factors that may aid the clinician in deciding on the prognostic value after primary repair of open globe injury. In conclusion, in the current study elapsed time between injury and surgery, age of the patient and mode of injury adversely affect the final visual outcome. Preoperative VA affects the final visual outcome on univariate analysis but when studied in correlation with other factors using binary logistic regression it was found to be statistically insignificant.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Parver LM. Eye trauma: The neglected disorder (editorial) Arch Ophthalmol. 1986;104:1452. doi: 10.1001/archopht.1986.01050220046022. [DOI] [PubMed] [Google Scholar]
- 2.Sterberg P., Jr . Prognosis and outcomes for penetrating ocular trauma. In: Shingleton BJ, Hersh PS, Kenyon KR, editors. Eye trauma. Louis: Mosby Year Book; 1991. pp. 238–41. [Google Scholar]
- 3.De Juan EJ, Sternberg PJ, Michels RG. Penetrating ocular injuries: Types of injuries and visual results. Ophthalmology. 1983;90:1318–22. doi: 10.1016/s0161-6420(83)34387-6. [DOI] [PubMed] [Google Scholar]
- 4.Barr CC. Prognostic factors in corneoscleral laceration. Arch Ophthalmol. 1983;101:919–24. doi: 10.1001/archopht.1983.01040010919013. [DOI] [PubMed] [Google Scholar]
- 5.Issac DL, Ghanem VC, Nascimento MA. Prognostic factors in open globe injuries. Ophthalmologica. 2003;217:431–5. doi: 10.1159/000073075. [DOI] [PubMed] [Google Scholar]
- 6.Esmaeli B, Elner SG, Schork A, Elner VM. Visual outcome and ocular survival after penetrating trauma: A clinicopathologic study. Ophthalmology. 1995;102:393–400. doi: 10.1016/s0161-6420(95)31009-3. [DOI] [PubMed] [Google Scholar]
- 7.Gilber CM, Soong HK, Hirst LW. A two- year prospective study of penetrating ocular trauma at the Wilmer Ophthalmological Institute. Ann Ophthalmol. 1987;19:104–6. [PubMed] [Google Scholar]
- 8.Pieramici DJ, Mathew W, MacCumber, Humayun MU. Open globe injury: Update on types of injuries and visual results. Ophthalmology. 1996;103:1798–803. doi: 10.1016/s0161-6420(96)30424-7. [DOI] [PubMed] [Google Scholar]
- 9.Pieramici DJ, Au Eong K, Sternberg PJ, Marsh MJ. Prognostic significance of a system for classifying mechanical injuries of the eye (globe) in open globe injuries. J Trauma. 2003;54:790–4. doi: 10.1097/01.TA.0000047053.53821.C8. [DOI] [PubMed] [Google Scholar]
- 10.Leonardo D, Ghanem VC. Prognostic factors in open globe injuries. Ophthalmologica. 2003;217:431–5. doi: 10.1159/000073075. [DOI] [PubMed] [Google Scholar]
- 11.Sternberg P, Jr, de Juan E, Jr, Michels RG, Auer C. Multivariate analysis of prognostic factors in penetrating ocular injuries. Am J Ophthalm. 1984;98:467–72. doi: 10.1016/0002-9394(84)90133-8. [DOI] [PubMed] [Google Scholar]
- 12.Hutton WL, Fuller DG. Factors influencing final visual results in severely injured eyes. Am J Ophthalm. 1984;97:715–22. doi: 10.1016/0002-9394(84)90503-8. [DOI] [PubMed] [Google Scholar]
- 13.Rofail M, Lee GA, Rourke P. Prognostic factors for open globe injury. Clin Exp Ophthalmol. 2006;34:783–6. doi: 10.1111/j.1442-9071.2006.01309.x. [DOI] [PubMed] [Google Scholar]
- 14.Schmidt GW, Broman AT, Hindman HB, Grant MP. Vision survival after open globe injury predicted by classification and regression tree analysis. Ophthalmology. 2008;115:202–9. doi: 10.1016/j.ophtha.2007.04.008. [DOI] [PubMed] [Google Scholar]
- 15.Rahman I, Maino A, Devadason D, Leatherbarrow B. Open globe injuries: factors predictive of poor outcome. Eye. 2006;20:1336–41. doi: 10.1038/sj.eye.6702099. [DOI] [PubMed] [Google Scholar]
- 16.Thakker MM, Ray S. Vision limiting complications in open globe injuries. Can J Ophthalmol. 2006;41:86–92. doi: 10.1016/S0008-4182(06)80074-8. [DOI] [PubMed] [Google Scholar]
- 17.Brinton GS, Aaberg TM, Reeser FH, Topping TM, Abrams GW. Surgical results in ocular trauma involving the posterior segment. Am J Ophthalmol. 1982;93:271–8. doi: 10.1016/0002-9394(82)90524-4. [DOI] [PubMed] [Google Scholar]
- 18.Kuhn F, Morris R, Witherspoon CD, Heimann K, Jeffers JB, Treister G. A standardized classification of ocular trauma. Ophthalmology. 1996;103:240–3. doi: 10.1016/s0161-6420(96)30710-0. [DOI] [PubMed] [Google Scholar]
- 19.Rao LG, Ninan A, Rao KA. Descriptive study on ocular survival, visual outcome and prognostic factors in open globe injuries. Indian J Ophthalmol. 2010;58:321–3. doi: 10.4103/0301-4738.64116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gupta A, Srinivasan R, Babu KR, Setia S. Comparison of the clinical presentation and visual outcome in open globe injuries in adults and children over 30 months. Eur J Ophthalmol. 2010;20:590–5. doi: 10.1177/112067211002000309. [DOI] [PubMed] [Google Scholar]
- 21.Shah M, Shah S, Khandekar R. Ocular injuries and visual status before and after their management in the tribal areas of western India: A historical cohort study. Graefes Arch Clin Exp Ophthalmol. 2008;246:191–7. doi: 10.1007/s00417-007-0698-y. [DOI] [PubMed] [Google Scholar]


