Abstract
Bilateral occurrence of macular hole in X-linked retinoschisis is an extremely rare event. Spectral domain optical coherence tomography (OCT) findings revealed that formation of a macular hole is secondary to the retinoschisis process alone. Bilateral macular holes should be added to the spectrum of X-linked retinoschisis variations and the retinoschisis process alone should be accounted for their formation.
Keywords: X linked retinoschisis, macular hole, spectral domain optical coherence tomography
X-linked retinoschisis (XLR) is a leading cause of macular degeneration in male children. Stellate foveal schisis is pathognomonic, with a peripheral retinoschisis in half the cases. However, a high degree of clinical variability is observed.[1] The other reported features include arborescent and dendriform retinal lesions, vascular sheathing, veils in the vitreous cavity, pseudopapillitis, pigmentary alterations, and neovascularization of the periphery or the optic disc.
Occurrence of a macular hole in patients of XLR is an extremely rare phenomenon. We searched in Medline and Ovid databases using search words X-linked retinoschisis, macular hole, spectral domain optical coherence tomography and did not find any article describing bilateral occurrence of macular hole in XLR. We are reporting a case of bilateral macular hole in XLR and emphasizing the origin of tangential traction secondary to elevation of retina.
Case Report
A 25-year-old male presented with complaints of defective vision in both eyes since early childhood without any complaint of night blindness. Family history was negative. Patient had no history of trauma and did not suffer from pathologic myopia. Visual acuity was 10/200 (4/60) in the right eye and counting finger close to face in the left eye. Anterior segment examination was within normal limits in both the eyes. Fundus examination revealed a large macular hole in the right eye [Fig. 1a], a small macular hole in the left eye [Fig. 1b] along with multiple small cystic cavities surrounding the macular holes, and peripheral retinal pigment epithelium mottling in both eyes. Electroretinogram (ERG) of both eyes revealed selectively reduced b-wave amplitude. Diagnosis of XLR was made which was substantiated by optical coherence tomography (OCT). Absence of nyctalopia and scotopic and photopic ERG responses excluded other diagnoses such as retinitis pigmentosa and Goldmann-Favre syndrome. OCT showed a large macular hole and rolled edges of the outer retinal layers in the right eye [Fig. 2a], a small macular hole in the left eye [Fig. 2b] and schisis of retina in both eyes. Macular hole edges showed bulb-like swelling of the retina. Separation of the outer nuclear layer from the outer plexiform layer can be seen underneath the superior edge of the large macular hole while it is still attached to the outer plexiform layer inferiorly. Curling of the separated outer nuclear layer is visible.
Figure 1.
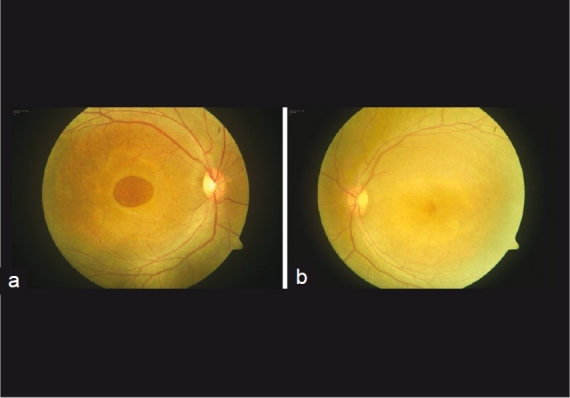
(a) Right eye, large macular hole (b) Left eye, stellate foveal schisis
Figure 2.
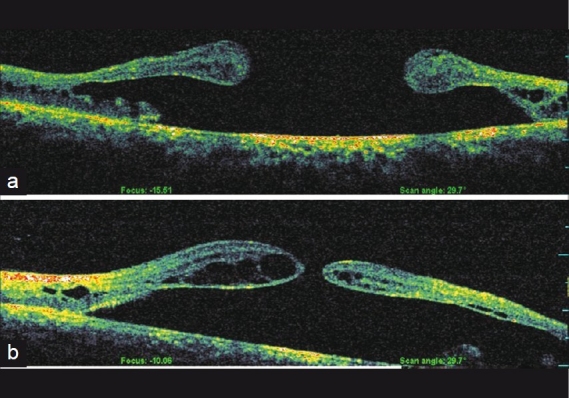
(a) Right eye, vertical OCT scan through large macular hole (b) Left eye, vertical OCT scan through small macular hole
In view of stable vision since many years and loss of photoreceptor layer from the foveal region no intervention was advised other than observation.
Discussion
XLR is a leading cause of macular degeneration in male children. It is characterized by a high degree of clinical variability.[1] Vision loss in the first decade is the most common clinical presentation. Bilateral foveal schisis is the most common clinical finding. Folds radiate outward in a stellate pattern from the foveola, and contain micro cystic schisis cavities. This clinical picture is characteristic and has been reported in 68-100% of affected males. The diagnosis of juvenile XLR typically is dependent on a careful fundus examination,[2] but OCT may be helpful for confirming the presence of the schisis cavity directly.[3]
Gass suggested a key role of ‘Muller-cell cone’ in the pathogenesis of age-related macular hole as well as congenital XLR. Muller-cell cone is the site for foveal splitting and cyst formation in both the pathologies.[4] In XLR, accumulation of defective retinoschisin protein within and around the Muller cells results in cystic spaces in multiple retinal layers.[1] Coalescence of these cysts causes formation of larger cysts which finally results in larger schisis cavities. This causes elevation of the schisis (retinal layers). In the uppermost region of the schisis cavities, degeneration of the retina takes place because of tangential traction caused by elevation of the retinal tissue. Breakage of inner layers occurs and a macular hole forms. In OCT scans of both eyes [Figures 3a and b] which are passing through edges of the macular holes, spindle-shaped swelling of the retina with kinking in the central part is visible. Degeneration of the retina in the central part appears to be responsible for the production and enlargement of the macular hole. It also explains the bulb-like swelling of the edges of the macular hole. These events are solely secondary to retinoschisis.
Figure 3.
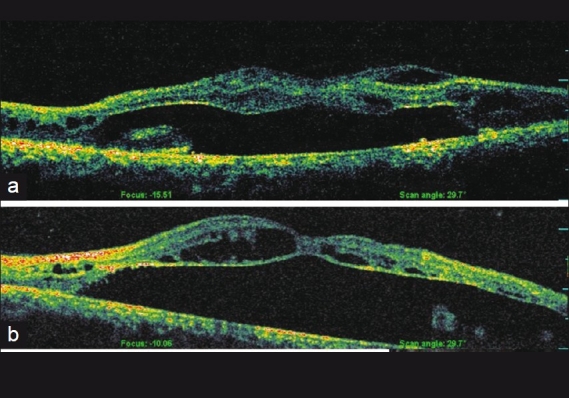
(a) Right eye, OCT scan through edge of macular hole (b) Left eye, OCT scan through edge of macular hole
Our view is in contrast to Shukla et al.,[5] who reported unilateral macular hole in XLR and suggested de-roofing as a possible event in the formation of the macular hole. Even in the OCT scan of the left eye of our case [Fig. 3B],where the hole is small, no vitreoretinal traction responsible for de-roofing can be attributed. Although cortical vitreous is strongly adherent to the internal limiting membrane in some cases of XLR, and exerts a tangential traction on the macula, dragging it nasally, particularly when vitreous veils create temporal redundancy,[6] no such observations can be made in our case. In another case report Shanmugam[7] has described unilateral macular hole in an XLR patient associated with retinal detachment. OCT images provided by the author showed prominent vitreoretinal traction. Vitreoretinal traction also has been considered to play a role in the pathogenesis of X-linked retinoschisis. However, such vitreoretinal traction was seen in only three eyes (9%) in a study done by Jia Yu,[8] even these eyes were not associated with any retinal elevation.
In summary, our case of XLR is unique in the sense that first it has bilateral occurrence of a macular hole and second there was no vitreoretinal traction visible on OCT. We have also described spectral domain OCT findings of this extremely rare presentation which will be helpful in understanding the natural course of XLR.
Conclusion
The clinical spectrum of XLR should include bilateral macular hole, and tangential traction secondary to elevation of retina should be considered as a responsible factor.
References
- 1.Tantri A, Vrabec TR, Cu-Unjieng A, Frost A, Annesley WH, Jr, Donoso LA. X-linked retinoschisis: A clinical and molecular genetic review. Surv Ophthalmol. 2004;49:214–30. doi: 10.1016/j.survophthal.2003.12.007. [DOI] [PubMed] [Google Scholar]
- 2.Gass JD. Heredodystrophic disorders affecting the pigment epithelium and retina. In: Gass JD, editor. Stereoscopic atlas of macular disease. 3rd ed. Vol. 1. St. Louis: CV Mosby; 1987. pp. 235–332. [Google Scholar]
- 3.Apushkin MA, Fishman GA, Janowicz MJ. Correlation of optical coherence tomography findings with visual acuity and macular lesions in patients with X-linked retinoschisis. Ophthalmology. 2005;112:495–501. doi: 10.1016/j.ophtha.2004.08.027. [DOI] [PubMed] [Google Scholar]
- 4.Gass JDM. Muller cell cone, an overlooked part of the anatomy of the fovea centralis. Arch Ophthalmol. 1999;117:821–823. doi: 10.1001/archopht.117.6.821. [DOI] [PubMed] [Google Scholar]
- 5.Shukla D, Naresh KB, Rajendran A, Kim R. Macular hole secondary to X-linked retinoschisis. Eye (Lond) 2006;20:1459–61. doi: 10.1038/sj.eye.6702338. [DOI] [PubMed] [Google Scholar]
- 6.Greven CM, Moreno RJ, Tasman W. Unusual manifestations of X-linked retinoschisis. Trans Am Ophthalmol Soc. 1990;88:211–25. [PMC free article] [PubMed] [Google Scholar]
- 7.Shanmugam MP, Nagpal A. Foveal schisis as a cause of retinal detachment secondary to macular hole in juvenile X-linked retinoschisis. Retina. 2005;25:373–5. doi: 10.1097/00006982-200504000-00022. [DOI] [PubMed] [Google Scholar]
- 8.Yu J, Ni Y, Keane PA, Jiang C, Wang W, Xu G. Foveomacular schisis in juvenile X-linked retinoschisis: An optical coherence tomography study. Am J Ophthalmol. 2010;149:973–8. doi: 10.1016/j.ajo.2010.01.031. [DOI] [PubMed] [Google Scholar]


