Abstract
Background:
Studies in developed nations have reported an association of blindness and hearing impairment with mortality in elderly persons.
Objectives:
To study the association of blindness and hearing impairment with mortality in a cohort of elderly persons in rural north India.
Materials and Methods:
This community-based prospective study was conducted in eleven randomly selected villages, in Ballabgarh block, Haryana. A cohort of 1422 participants, of age 60 years and above, was examined at baseline, for their visual and hearing status. Data on the sociodemographic factors, various comorbidities, activities of daily living, and self-rated health were recorded. Baseline data was collected for the period May 2008 to August 2008. Follow-up data collection for mortality was completed in December 2009. The median follow-up period was 518 days.
Results:
One hundred out of 1422 elderly (7.0%) participants died during the follow-up period. Significant hazard ratios were found after adjustment for various comorbid conditions. On adjustment for sociodemographic factors (age, sex, and literacy), neither blindness nor hearing impairment was found to be significantly associated with mortality. After adjustment for all covariates in the study, hearing impairment (Hazard Ratio = 2.13; 95% CI, 1.29 – 3.54) was found to be significantly associated with mortality in the age group ≥70 years.
Conclusions:
This study demonstrated that hearing impairment was an independent risk factor for mortality in people aged ≥70 years. Similar studies with a longer period of follow-up are required in India, to guide public health interventions.
Keywords: Blindness, cohort, elderly, hearing impairment, mortality
Introduction
India is currently undergoing a demographic transition, with a shift to a higher proportion of elderly (increased from 5.6% in 1961 to 7.4% in 2001).(1) Increasing numbers of people are at risk of age-related visual impairment as the elderly population increases.(2) Blindness and hearing impairment contribute heavily to the overall burden of impairment. More than half of all the impaired persons in India have either visual or hearing impairment.(3) Even as the elderly are at a higher risk of developing disabilities, it is also possible that the presence of single or multiple disabilities may increase the risk of death among them. The ‘at-risk approach’, used in maternal and child health care, can be adopted for the care of the elderly as well.(4) Identification of groups among the elderly, who are at a greater risk of dying, will facilitate targeted interventions, with optimal utilization of the available resources. Among them, blindness and hearing impairment could be two possible predictors of mortality.
Various researchers in industrialized countries have studied the association of blindness and/or hearing impairment with mortality in the elderly.(5–17) It was felt that it would be useful to study this association in India.
The objective of the present community-based prospective study was to examine the association of blindness and hearing impairment with mortality in a cohort of elderly persons, aged 60 years or more, in a rural area.
Materials and Methods
The study was conducted in villages that are covered under the Intensive Field Practice Area (IFPA) of the Comprehensive Rural Health Services Project (CRHSP), Ballabgarh, District Faridabad, Haryana. It is a collaborative project between the All India Institute of Medical Sciences, New Delhi, and the state government of Haryana. The project caters to a population of about 88000 persons in 28 villages. Health care services are provided by medical officers and their teams of health assistants and health workers, through a network of two Primary Health Centers and twelve sub-centers. A Health Management Information System (HMIS) is in place, wherein, every person in these villages is allocated a unique 16-digit number and is under continuous demographic surveillance.
Ethical approval for the study was obtained from the Ethics Committee of the All India Institute of Medical Sciences, New Delhi, India. Written informed consent was obtained from the participants.
The relative risks reported in previous similar studies ranged from 1.15 to 2.9.(9,11) The December 2007, census data of this area had reported a death rate of 4.45% in elderly persons. Considering a relative risk of 2.0, and 4.45% deaths among the non-blind elderly persons, with a 5% level of significance, and power of 80%, the estimated sample size was 1381 elderly persons. This sample size was calculated for an exposed: unexposed ratio of 1: 3.
The study population consisted of all elderly persons (age ≥60 years) living in the study villages at the time of baseline examination. Eleven villages were selected randomly. The total population of the selected villages was 23979, including 1465 (6.1%) elderly persons (CRHSP Ballabgarh – December 2007 census). Of these 1465 persons, 1422 (97%) were recruited and followed up for the outcome measurement, with no loss to follow-up. Of the remaining 43 persons, 17 refused to participate, 16 were excluded from the study, as it was not possible to administer the study tests to them, and 10 could not be contacted despite three visits to their homes. Baseline data collection was carried out from May 2008 to August 2008, and follow-up data collection was completed in the month of December 2009.
A questionnaire was administered to all the study participants, to collect information on the sociodemographic details, history of associated morbidities (hypertension, diabetes mellitus, coronary artery disease, stroke, and any orthopedic impairment), data on self-rated health, and feeding and dressing. The questionnaire was pretested, and the necessary improvements were made. It was developed in English, translated into Hindi, and then back-translated into English to check for the correctness of the translation. It was administered to the participants in Hindi, by a single trained investigator. The history of five of the above-mentioned specific morbidities was elicited by asking the question, “Are you suffering from any of these illnesses, or have you taken treatment for any of them?” Orthopedic impairment was assessed by observation as well. Visual acuity was recorded with a Snellen's vision chart. The vision was recorded at a distance of 6 m separately for each eye; with distant glasses, if any. Blindness was defined as a visual acuity of less than 6/60 in the better eye, with available correction. For hearing assessment, all participants were administered the Whisper test first, and subsequently examined with the Rinne's test and Weber's test, using a 512 Hz tuning fork by the investigator. The Whisper test was calibrated using the audiometer, before administration to the participants. The initial calibration and fortnightly appraisals during the period of data collection were done under the supervision of a faculty from the department of the ear, nose, and throat (ENT), All India Institute of Medical Sciences, New Delhi.
All participants found blind or hearing impaired at the time of baseline examination were referred to Ophthalmology and ENT clinics at the comprehensive rural health services project (CRHSP), Ballabgarh Hospital for Management. These participants were contacted again at the time of follow-up examination. They were asked about any improvement of visual/auditory status during the follow-up period. Data for the outcome variable, that is, all-cause mortality during the follow-up period, were collected from death registers maintained by health workers of the sub-centers covering the respective villages. Accredited social health activists (ASHAs) and Anganwadi workers of the respective villages were also contacted to collect data on the deaths that occurred after the last visit of the health worker. Furthermore, the mortality data were cross-checked for deficiencies/discrepancies, if any, with the Health Management Information System (HMIS) at CRHSP, Ballabgarh.
Data were entered in an MS Excel sheet. Analysis was done using STATA 9.0 (College Station, Texas, USA). Data were presented as number (percentage). The association of the demographic variables and various self-reported morbidities, with mortality, was compared using the chi-square test. The Cox proportional hazard models, both univariate and multivariate, were used to find the hazard of blinding and hearing impairment on mortality. The results were reported as Hazard Ratio (95% C.I.). The P value less than 0.05 was considered statistically significant.
Results
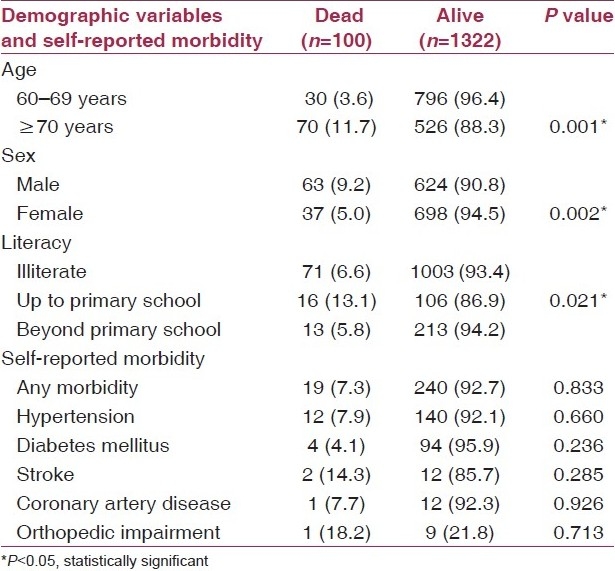
Results of the 1422 participants – 58.1% were in the age group of 60 to 69 years. About half (51.7%) of the participants were female and three-fourth of the participants (75.5%) had had no schooling. Sixty-two (4.4%) participants were dependent on others for dressing and 53 (3.9%) for feeding. Hypertension was reported by 10.7% and diabetes mellitus by 6.9% participants [Table 1]. Their own health was reported as fair by 68.3%, poor by 14.9%, good by 13.5%, very poor by 1.8%, and excellent by 1.5% of the participants.
Table 1.
Baseline characteristics of the participants
There were no out-migrations among participants during the follow-up period. No participant reported improvement of vision or hearing impairment during the follow-up period.
One hundred out of the 1422 (7%) participants died during the follow-up period. The follow-up period for participants ranged from a minimum of three days to a maximum of 567 days, with the median follow-up period being 518 days.
Out of 134 blind participants, 15 (11.2%) died, as compared to 85 deaths (6.6%) out of 1288 participants with normal vision (P=0.048). The percentage of deaths was significantly (P=0.001) higher in participants with hearing impairment (13.3%), as compared to participants with no hearing impairment (5.9%).
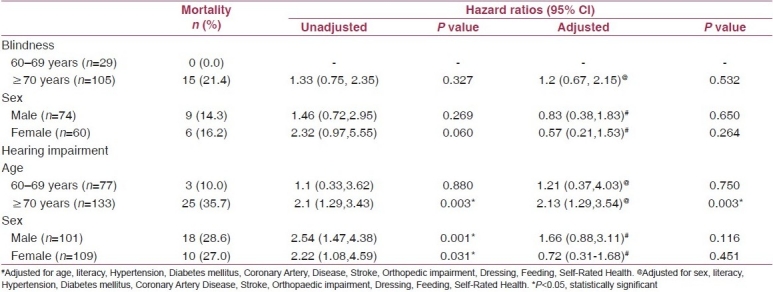
After adjustment for all the covariates (age, sex, literacy, hypertension, diabetes mellitus, coronary artery disease, stroke, orthopedic impairment, dressing, feeding, self-rated health), neither blindness nor hearing impairment was found to be significantly associated with mortality. Adjustment for only morbidities had no effect on the crude hazard ratios [Table 2].
Table 2.
Association of blindness and hearing impairment with mortality

On further exploratory analysis by age and sex, hearing impairment was found to be significantly associated with mortality in the age group ≥70 years with a Hazard Ratio of 2.13 (1.29 – 3.54; 95% CI). The rest of the associations were insignificant. Hazard ratios for blindness in the age group 60 – 69 years could not be calculated, as there were no events in that group [Table 3].
Table 3.
Association of blindness and hearing impairment with mortality by age and sex
Discussion
In this cohort study, we investigated the association of blindness and hearing impairment with mortality in the elderly age group in a rural area. A few studies conducted across the world have addressed the same study question, albeit in urban areas.(5–17) In the Indian context, as more than two-thirds of the population is residing in rural areas, this is an important consideration.
Univariate analysis revealed an association of blindness and hearing impairment with mortality. This corroborates the evidence generated from similar previous studies.(5–17) The male gender appeared to be protected for blindness as compared to the female gender in this univariate analysis. However, no association existed between blindness and mortality, after adjustment was made for sociodemographic factors (age, sex, and literacy). This finding is not in agreement with the findings from the previous studies. One of the possible reasons for the differing results could be the different sociodemographic factors for which the adjustments were made.(5–12)
In the study by Wang et al., from Australia, adjustments were made for height, weight, body mass index, and home ownership, apart from age and sex,(5) and in another study by Lee et al. from USA, adjustments were made for age, sex, race, and marital status.(7)
Adjustments only for the selected morbidities, had no effect on the observed association between blindness and mortality. This was in support of the evidence generated by various similar previous studies.(5,6,8–10,12) However, in some studies, the observed association between blindness and mortality was no longer present, at least in some subgroups, once the adjustments were made for the identified confounders.(7,11) This could be due to a difference between various potential confounders adjusted for in the studies, and different methods used for their ascertainment.
Hearing impairment remained associated with mortality; however, the results became insignificant once adjustments were made for the sociodemographic factors, especially age. This was in agreement with one study conducted in Canada by Ostbye et al.(15)
Hearing impairment was found to be significantly associated with mortality even after adjustment for all the potential confounders in the age group of 70 years or more. Similar significant associations were reported in the same age group in one previous study in Italy.(16)
It is possible that hearing impairment is a marker of accelerated aging, and hence, is indicative of a greater risk of death in those who are hearing impaired.
Similarly, in a study by Lam et al., in the United States, significant association was found between hearing impairment and mortality among a group of women belonging to the non-white, non African–American race (including Asians, among others).(14)
A couple of limitations need to be mentioned. First, the period of person-years of follow-up in the present study was smaller in comparison to other similar studies, mostly due to the lower duration of follow-up. Second, the method of ascertainment of the comorbid conditions was self-reported by the participants, which could have resulted in some diagnostic gap for the said morbidities.
To conclude, the results of the present study showed that elderly persons aged ≥70 years, residing in the rural area, who suffered from hearing impairment, were at increased risk of mortality, as compared to persons without this impairment. Sociodemographic factors (age, sex, and literacy) had a strong confounding effect. However, the presence of various comorbid conditions (hypertension, diabetes mellitus, coronary artery disease, stroke, and orthopedic impairment) had no effect on this association.
The presence of hearing impairment in the age group ≥70 years should be considered as a risk factor for mortality, and more efforts for mortality reduction should be directed toward this ‘at-risk group’ through screening.
With the increase in the elderly population in India, similar studies with longer follow-up periods are warranted, to generate an evidence-base for public health interventions.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1. [Last accessed on 2010 Aug 9]. Available from: http://www.censusindia.gov.in/Census_Data_2001/India_at_glance/broad.aspx .
- 2. [Last accessed on 2010 Aug 9]. Available from: http://www.who.int/mediacenter/factsheets/fs282/en/index.html .
- 3. [Last accessed on 2010 Aug 9]. pp. 1–4. Table C-20, Available from: http://www.censusindia.gov.in/Tables_Published/C.Series/C.Series_link/c20_india.pdf .
- 4. [Last accessed on 2010 Aug 17]. Available from: http://whqlibdoc.who.int/php/WHO_PHP_76.pdf .
- 5.Wang JJ, Mitchell P, Simpson JM, Cumming RG, Smith W. Visual impairment, age-related cataract, and mortality. Arch Ophthalmol. 2001;119:1186–90. doi: 10.1001/archopht.119.8.1186. [DOI] [PubMed] [Google Scholar]
- 6.Taylor HR, McCarty CA, Nanjan MB. Vision impairment predicts five-year mortality. Trans Am Ophthalmol Soc. 2000;98:91–6. [PMC free article] [PubMed] [Google Scholar]
- 7.Lee DJ, Gómez-Marín O, Lam BL, Zheng DD. Visual acuity impairment and mortality in US adults. Arch Ophthalmol. 2002;120:1544–50. doi: 10.1001/archopht.120.11.1544. [DOI] [PubMed] [Google Scholar]
- 8.Knudtson MD, Klein BE, Klein R. Age-related eye disease, visual impairment, and survival: The Beaver Dam Eye Study. Arch Ophthalmol. 2006;124:243–9. doi: 10.1001/archopht.124.2.243. [DOI] [PubMed] [Google Scholar]
- 9.Foong AW, Fong CW, Wong TY, Saw SM, Heng D, Foster PJ. Visual acuity and mortality in a chinese population. The Tanjong Pagar Study. Ophthalmology. 2008;115:802–7. doi: 10.1016/j.ophtha.2007.04.066. [DOI] [PubMed] [Google Scholar]
- 10.Karpa MJ, Mitchell P, Beath K, Rochtchina E, Cumming RG, Wang JJ. Direct and indirect effects of visual impairment on mortality risk in older persons. Arch Ophthalmol. 2009;127:1347–53. doi: 10.1001/archophthalmol.2009.240. [DOI] [PubMed] [Google Scholar]
- 11.Freeman EE, Egleston BL, West SK, Bandeen-Roche K, Rubin G. Visual acuity change and mortality in older adults. Invest Ophthalmol Vis Sci. 2005;46:4040–5. doi: 10.1167/iovs.05-0687. [DOI] [PubMed] [Google Scholar]
- 12.Berdeaux G, Brézin AP, Fagnani F, Lafuma A, Mesbah M. Self-reported visual impairment and mortality: a French nationwide perspective. Ophthalmic Epidemiol. 2007;14:80–7. doi: 10.1080/09286580600899691. [DOI] [PubMed] [Google Scholar]
- 13.Karpa MJ, Gopinath B, Beath K, Rochtchina E, Cumming RG, Wang JJ, et al. Associations between hearing impairment and mortality risk in older persons: The Blue Mountains Hearing Study. Ann Epidemiol. 2010;20:452–9. doi: 10.1016/j.annepidem.2010.03.011. [DOI] [PubMed] [Google Scholar]
- 14.Lam BL, Lee DJ, Gómez-Marín O, Zheng DD, Caban AJ. Concurrent visual and hearing impairment and risk of mortality, The National Health Interview Survey. Arch Ophthalmol. 2006;124:95–101. doi: 10.1001/archopht.124.1.95. [DOI] [PubMed] [Google Scholar]
- 15.Ostbye T, Steenhuis R, Wolfson C, Walton R, Hill G. Predictors of five-year mortality in older Canadians: The Canadian study of health and aging. J Am Geriatr Soc. 1999;47:1249–54. doi: 10.1111/j.1532-5415.1999.tb05207.x. [DOI] [PubMed] [Google Scholar]
- 16.Appollonio I, Carabellese C, Magni E, Frattola L, Trabucchi M. Sensory impairments and mortality in an elderly community population: a six-year follow-up study. Age Ageing. 1995;24:30–6. doi: 10.1093/ageing/24.1.30. [DOI] [PubMed] [Google Scholar]
- 17.Michikawa T, Nishiwaki Y, Kikuchi Y, Nakano M, Iwasawa S, Asakura K, et al. Gender-specific associations of vision and hearing impairments with adverse health outcomes in older Japanese: a population-based cohort study. BMC Geriatr. 2009;9:50. doi: 10.1186/1471-2318-9-50. [DOI] [PMC free article] [PubMed] [Google Scholar]


