Abstract
Background:
Maternal mortality is a reflection of the care given to women by its society. It is tragic that deaths occur during the natural process of child birth and most of them are preventable.
Objectives:
The present study was undertaken to find out the causes and contributing factors of maternal deaths.
Materials and Methods:
All maternal deaths occurring in a year in the medical college and hospital were traced and interviews were taken from the relatives as well as the health care providers who were present at the time of death of the woman.
Results:
Out of the total maternal deaths, 72% belonged to 20-30 yrs age group, also 46.5% were illiterate, and majority deaths (60.5%) were from low socio-economics status. Direct causes were responsible for 76.7% of maternal deaths. Hypertensive disorders of pregnancy were most common (32.6%) cause of direct deaths, while malaria (9.3%) and anemia (7%) were most common indirect causes. Most of the women had to use their own resources to travel to health care facilities. Delays at different levels, often in combination, contributed to the maternal deaths.
Conclusions:
The study will serve as an eye-opener to the bottlenecks present in the community as well as in the health facility so as to take appropriate measures to prevent maternal deaths.
Keywords: Causes, delays, maternal death
Introduction
Worldwide, nearly 600,000 women between the ages of 15 and 49 die every year as a result of complications arising from pregnancy and childbirth.(1,2) These women die not from any disease but during the normal, life-enhancing process of procreation and most of these deaths are avoidable. Maternal mortality is not only a health disadvantage, rather it is a social disadvantage as it puts economic burden on the family, community, governments, and nations.
India is one of the countries with a high maternal mortality ratio (MMR) and the highest (136,000) estimated number of maternal deaths.(3) The main causes of maternal mortality in India are hemorrhage, sepsis, abortion, hypertensive disorders, and obstructed labor.(4) MMR for India was 407 by SRS 1997 estimates and came down to 301 per 100,000 live births by SRS 2003 estimates.(4) Going by this pace we would achieve the MMR of 195 by the year 2012 and of 160 by 2015, far from the NRHM goal of 100 per 100,000 live births by 2012 or Millennium Development Goal of 109 per 100,000 live births by 2015.(4) Orissa being an Empowered Action Group (EAG) state, has a high MMR of 358 per 100,000 live births.(4)
Maternal deaths occur both inside and outside the health institutions. Only estimating mortality rates are not beneficial, to know why and how they die is much more important to prevent such deaths. Even for deaths which occur in the hospitals, the actual reasons and the contributory factors may lie in the community.
The objectives of the study were –To elucidate the magnitude and causes of maternal deaths and to explore the factors and/or circumstances contributing to them.
Materials and Methods
This is a cross-sectional study. All the maternal deaths at S. C. B. Medical College and Hospital, Cuttack, Odisha, from 1 April 2006 to 31 March 2007 were included in the study. The study was conducted from July 2006 to June 2007. It was an ongoing process of identifying maternal deaths, tracing out their residences, providing prior intimation, and finally paying a visit to the family. The WHO definition of maternal deaths was adopted for the study.(5,6)
Information about maternal deaths was obtained from death register and bed head tickets (BHTs). Addresses were noted and letters were dispatched explaining the nature of the study and purpose of the visit to deceased women's homes. Semi-structured questionnaires were used for interviewing the relative(s) and the health care provider(s) (HCPs) present with the deceased woman. HCPs of the local community as well as in the tertiary hospital were interviewed to verify some of the points of the relatives and to obtain additional information, e.g. constraints in the hospital. Informed consent was taken from each respondent before the interview. Substantial help was taken from the WHO-developed questionnaires for verbal autopsy and facility-based studies.(6)
The SES was assessed and classified according to the social score method adopted by the WHO international collaborative study on family formation pattern and health.(7) The SES assessed four variables – educational status and occupation of the head of the household, per capita monthly income and housing. The study classifies maternal deaths as direct and indirect according to the WHO classification.(1) Direct deaths result from obstetric complications of pregnant state (pregnancy, labor, and puerperium). Indirect deaths are those resulting from previously existing disease or disease developing during pregnancy and aggravated by pregnancy. Delays are classified as types I, II or III.(8) Type I delay – delay in seeking modern medical care; type II delay – delay in reaching a health facility, and type III delay – delay in receiving appropriate care at the health facility.
Of the 50 deaths that had occurred during this period, only 43 addresses could be traced out for home visits. Therefore, final analysis was done on these cases only. Data thus collected was scrutinized, edited, and analyzed in the department. The data was analyzed using SPSS 11.0 (Statistical Package for Social Sciences). Proportions were used to describe the results.
Results
The total number of deliveries and live births in the hospital during the study period was 6941 and 6881, respectively. The maternal mortality ratio was 727 per 1,00,000 live births. Most of the maternal deaths (72.1%) were in the 20–30 year age group. Proportional maternal mortality, i.e. maternal deaths per lakh women delivering in each specific age group was 893, 636, 588, and 631 in <20, 20–24, 25–29, and >30 year age group, respectively. A majority of the deceased women were from (53.5%) general caste. Nearly half of these women (46.5%) were illiterates, while 27.9% had education below secondary level. 93% women were married, while two (4.7%) women were unmarried at the time of death. Being a social taboo, the unmarried women tried illegal abortion methods which resulted in fever, bleeding per-vagina, and septicemia; finally, they were admitted to this tertiary hospital. Most of these women (60.5%) were from low SES; none were from high SES. 55.8% of the deceased mothers were primi-gravida.
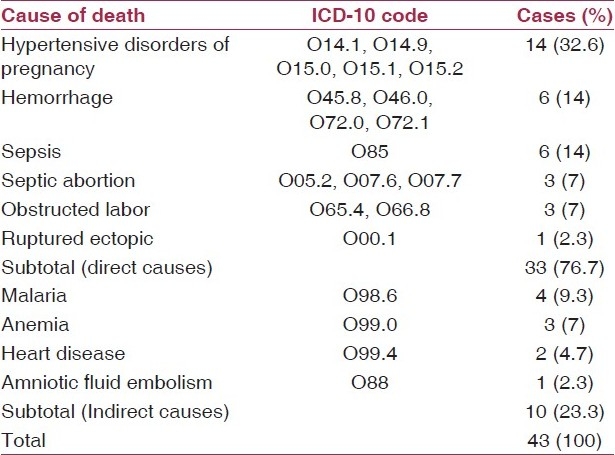
Direct causes were responsible for 76.7% of maternal deaths [Table 1]. 32.6% cases had died due to hypertensive disorders of pregnancy which included eclampsia (18.6%) and pregnancy-induced hypertension (14%). Most of the deaths were due to eclampsia in pregnancy (O15.0, ICD-10) followed by severe pre-eclampsia (O14.1, ICD-10). Hemorrhage and sepsis (14% each) were other important causes of maternal deaths. Hemorrhage was mostly post-partum (O072.0 and O072.1, ICD-10) in nature. Malaria (9.3%) and anemia (7%) were common indirect causes. The most common immediate(6) causes of death were hemorrhage and shock (16.3% each). Anemia was the most common (48.8%) contributory(6) cause of maternal death.
Table 1.
Underlying cause of death of the deceased women
Regarding antenatal care, 58.1% of the deceased women had received adequate antenatal checkup as per RCH guidelines,(9) while 23% had no ANC/TT immunization. Also, 74.4% of these mothers did not take the required amount of IFA tablets.(10) All of these deceased women had no prior planning for institutional delivery. Even 67% of these women were never been told about institutional delivery or delivery by skilled birth attendant (SBA). 14% and 11.6% were delivered by a traditional healer and a local dhai, respectively.
The minimum distance from home to the nearest health facility was 0.5 km; the maximum distance was 30 km. The average distance traveled to reach nearest health facility was 10.9 km; the average time taken was 1.2 h. 58.5% mothers had to travel for 1 h or more to reach the nearest health facility. The mode of transport for most of the women (51.1%) was auto-rickshaw. Hired cars, motorcycles, and cycles were also used for transportation. The mean distance to the Referral hospital (S. C. B. Medical College and Hospital) was 81.9 km, while the median time taken for reaching it was 8 h. A majority of deceased women (60%) reached the referral hospital within 10 h. 46.5% of mothers could utilize the medical ambulance services of the first health facility to reach the Referral Hospital while others hired cars (39.5%), private ambulances (7%), or auto-rickshaws (7%).
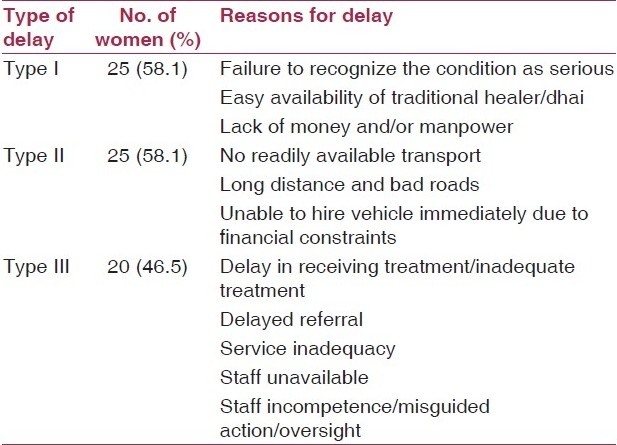
Delays at different levels contributed to the maternal deaths. Type I and type II delay each had a role in 58% of maternal deaths, while in 46.5% of cases, type III delay was one of the contributing factors [Table 2]. In most of the cases of maternal deaths, multiple types of delay were co-existing.
Table 2.
Type of delay contributing to maternal deaths (multiple delays were present simultaneously)
Discussion
The age distribution pattern of the deceased mothers is similar to the pattern of maternal deaths in India.(4) 25.6% of these mothers were in the risk group(10) at the time of child birth. In a study by Sarin et al.,(11) the 57.8% of maternal deaths was in the 21–30 year age group. The proportional maternal mortality is least in 20–30 years although absolute numbers of maternal deaths are highest. However, proportional number of deliveries and near misses(6) in age-specific groups has not been computed for this study. An ICMR study(12) reported that 62.7% of maternal deaths were in uneducated women. A study by Sarin et al.(11) reported that a majority of the maternal deaths were among women belonging to poor class (76.4%). A majority (55.8%) of deaths in the present study were in primigravida. Oladapo et al.(13) reported that about one third of the women who died were experiencing their first child birth. Age at marriage, literacy, socio-economic status, and parity are some of the determinants of maternal mortality and can act as risk factors if are on the unfavorable side.(10,14)
The most common cause of maternal death was hypertensive disorders of pregnancy (30%). Govt. of India and the WHO(1,4,15) report hemorrhage as the most common cause. The pattern of causes in this hospital-based study is quite different from that seen in community. Direct cause contributed to 76.7% of all deaths in the hospital. In most of the hospital-based studies in India,(12,16–18) the direct causes were responsible for 51% to 82% of maternal mortalities. A similar study by Oladapo et al.(13) reported hypertensive disorders of pregnancy (28%) as the most common cause of maternal death followed by hemorrhage (21.3%) and sepsis (20.0%).
Here the common indirect causes of maternal death were malaria (10%) and anemia (8%). In different hospital-based studies in Orissa and other parts of India,(19–23) the mortality in pregnant women suffering from Falciparum malaria ranged from 4% to 66%. In a study by Chhabra et al.,(24) the main indirect cause of death was anemia (13.9%).
Proper ANC check-up, TT immunization, and IFA tablet consumption all help for a better prognostic outcome of childbirth. Many of the deceased mothers had poor ANC (41.9%), inadequate TT immunization (37.3%), and IFA tablets consumption (74.4%). A majority of the mothers (67.4%) had not received any advice for safe confinement. Advice for safe confinement includes advice to deliver the baby at a health institution or by a SBA as a routine. Women who are told about safe confinement can be better prepared both psychologically and financially during delivery.
The mean distance to the Referral hospital was 81.9 km while the median time taken for reaching it was 8 h. Long distances, poor communication facilities, unavailability of transport service, delay in arranging for transport, money and manpower, shifting to multiple facilities, delay in the health facility(s), delay in referral, and poor condition of roads were the reasons for the long time interval.
In the present study, type I and type II delay, each had a role in 58% of maternal deaths, while in 46.5% of cases type III delay was one of the contributing factors. Multiple delays were major contributing factors for maternal mortality. In a study by Cham et al.,(25) in 7 of the 32 cases the process of seeking medical attention was delayed, 27 of the 32 women were delayed in reaching an appropriate medical facility, while 31 women experienced delay in receiving prompt and adequate obstetric care at the hospital level. Distance to health centre and its accessibility, availability of transport, and prompt referral of critical/unmanageable cases are some important determinants to reducing the burden of maternal mortality besides ability to make quick decisions to seek medical help on the part of the stakeholder(s).
Conclusion
An attempt has been made in the present study to throw light upon some of the community factors which had contributed to maternal deaths in this tertiary level health center so that steps can be taken to prevent such type of maternal deaths in future. The pattern of causes of maternal deaths in the hospital is different from that in the community, so the health institution has to be geared up accordingly. Factors like low socio-economic status, low educational level, and delays at different levels should be closely evaluated. Subsequent studies on maternal mortality like surveys of severe morbidity (Near Misses)(6) will help in providing further evidence. People have to be made aware about the role of medical institutions in preventing the maternal deaths so that they can take timely decisions to reach health institutions.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Maternal Mortality in 2004, Estimates developed by WHO. Geneva: UNICEF and UNFPA; 2004. WHO, UNICEF, UNFPA. [Google Scholar]
- 2.Reduction of maternal mortality: A joint WHO/UNFPA/UNICEF/World Bank statement. Geneva; 1999. World Health Organization. [Google Scholar]
- 3.Maternal Mortality in 2000, Estimates developed by WHO. Geneva: UNICEF and UNFPA; 2004. World Health Organization. [Google Scholar]
- 4. Govt. of India (Sample Registration System), Maternal Mortality in India: 1997.2003, Trends, Causes and Risk Factors, Registrar General, India, New Delhi in collaboration with Centre for Global Health Research, Toronto.
- 5.International Statistical Classification of Diseases and Related Health Problems. Tenth Revision. Geneva: World Health Organization; 1992. World Health Organization. [PubMed] [Google Scholar]
- 6.Beyond the numbers: Reviewing maternal deaths and complications to make pregnancy safer. Geneva: World Health Organization; 2004. World Health Organization. [Google Scholar]
- 7.Omran AR, Standley CC, Azar JE, Bertan M, Guzman V, Nahapetian V, et al. Family formation pattern and health, An international collaborative study in India, Iran, Lebanon, and Philippines. Geneva: WHO; 1976. p. 561. [Google Scholar]
- 8.Maternal Mortality Update 2002: A Focus on Emergency Obstetric Care. New York: UNFPA; 2003. United Nations Population Fund (UNFPA) [Google Scholar]
- 9.Govt. of India, MCH Division. National Child Survival and Safe Motherhood Programme. 1994 [Google Scholar]
- 10.Park K. Park's Textbook of Preventive and Social Medicine. 20th ed. 2009. p. 450. (482, 556-7). [Google Scholar]
- 11.Sarin AR, Singla P, Kaur H. Maternal mortality - Aetiological factors: Analytic study from a teaching hospital of Punjab. Indian J Mat Child Hlth. 1992;3:69–73. [PubMed] [Google Scholar]
- 12.Bedi N, Kambo I, Dhillon BS, Saxena BN, Singh P. Maternal deaths in India: Preventable Tragedies (An ICMR Task Force Study) J Obstet Gynecol Ind. 2001;51:86–92. [Google Scholar]
- 13.Oladapo OT, Lamina MA, Fakoya TA. Maternal deaths in Sagamu in the new millennium: A facility-based retrospective analysis. BMC Pregn Childbirth. 2006;6:6. doi: 10.1186/1471-2393-6-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Konar H. D. C. Dutta's Textbook of Obstetrics. 7th ed. 2011. pp. 603–4. (630-1). [Google Scholar]
- 15.World Health Organization. The World Health Report: Make every mother and child count. 2005 [Google Scholar]
- 16.Bhasker Rao K. Maternal mortality in a teaching hospital in Southern India: A 13-year study. Obstet Gynecol. 1975;46:397–400. [PubMed] [Google Scholar]
- 17.Majhi AK, Sanyal P, Chakraborty T, Mukherjee GG. Changing trends in maternal mortality in a teaching cum referral hospital. J Obstet Gynaecol India. 1996;46:345–53. [Google Scholar]
- 18.Rao KB, Malika PE. A study of maternal mortality in Madras city. J Obstet Gynaecol India. 1977;27:876–80. [PubMed] [Google Scholar]
- 19.Clinical course of malaria in pregnancy a prospective controlled study from India. Trans Royal Soc Trop Med Hyg. 1988;82:376–9. doi: 10.1016/0035-9203(88)90124-1. [DOI] [PubMed] [Google Scholar]
- 20.Mishra SK, Mohanty S, Satpathy SK, Patnaik JK. Complicated Falciparum malaria during pregnancy. J Obstet Gynaecol. 1998;48:31–4. [Google Scholar]
- 21.Nair LS, Nair AS. Effects of malaria infection on pregnancy. Indian J Malariol. 1993;30:207–14. [PubMed] [Google Scholar]
- 22.Singh N, Awadhia SB, Dash AP, Shrivastava R. Malaria during pregnancy: A priority area for malaria research and control in South East Asia. Vol. 9. East Asia: Regional Health Forum; 2005. p. 1. [Google Scholar]
- 23.Saikia PK, Battacharjee NK, Baruah KD. Malaria in pregnancy. A clinical study in an industrial hospital. Abstract published in Journal of Association of Physician of India. 50th Golden Jubilee Conference, Madras. 1994 [Google Scholar]
- 24.Chhabra S, Sirohi R. Averting maternal deaths in spite of resource constraints: An Indian rural experience over two decades. J Obstet Gynaecol. 2004;24:521–4. doi: 10.1080/01443610410001722563. [DOI] [PubMed] [Google Scholar]
- 25.Cham M, Sundby J, Vangen S. Maternal mortality in the rural Gambia: A qualitative study on access to emergency obstetric care. Reprod Health. 2005;2:3. doi: 10.1186/1742-4755-2-3. [DOI] [PMC free article] [PubMed] [Google Scholar]


