Introduction
Postpartum period is the period that is associated with intense physical and emotional changes leading to anxiety and mood disturbances. There are three degrees of postpartum mood disorders, i.e., “baby blues”, postpartum depression (PPD), and postpartum psychosis.(1) Postpartum blues (PPB), otherwise “baby blues,” are comparatively milder in nature and are the most common one.(2) It generally begins 1 to 3 days after parturition and is distinguished by sudden mood swings, unexplained weeping, irritability and impatience, lack of sleep, crying spells, anxiety, loneliness, and a feeling of vulnerability.(3)
About 60–80% of all new mothers suffer from the PPB which rarely requires medication and normally subsides with support and education.(4) It is significant to carry out the follow-up, because up to 20% of these mothers are likely to progress to PPD and an adverse consequence on children's cognitive growth.(5) The exact cause of PPB is not known, but various factors such as hormonal changes, sociocultural factors, economical conditions, and relationship conflicts have been found to be associated.(6)
Early diagnosis of PPB and identification of the risk factors involved will allow the healthcare provider to prevent it from developing into PPD. Hence, this study was conducted to assess the possible correlates involved in PPB in an urban society.
Materials and Methods
A survey was carried out among mothers within 2 weeks of delivery at a referral hospital in Bangalore after obtaining the approval from hospital authorities and ethical committee. Mothers within 2 weeks of delivery and in good health were included from the maternity ward and from outpatient department after obtaining the written consent. Women with debilitating illness, disabling mental disorders, alcohol dependence, and narcotic drug dependence were excluded from the study. Based on ICH-GCP guidelines, 130 subjects in the age group of 18–45 years were randomly screened.
Two questionnaires were used in this study. Subjects were encouraged to complete the questionnaires on their own with minimum assistance to avoid bias. First questionnaire was the Edinburgh Postnatal Depression Scale (EPDS), used to diagnose the PPB. The EPDS included 10 questions and each one is valued on a four-point scale with maximum possible score of 30.(7) The subjects who scored more than 10 were considered to be suffering from “baby blue.” Second questionnaire was the maternal demographic questionnaire used to identify the correlates of PPB.
The statistical analyses used were descriptive analysis, Chi-square test of significance, and Fisher's exact probability test. The association between the demographic variables and PPB was tested using chi-square test of significance and Fisher's exact probability test. The statistical analyses were performed with the help of SPSS software version 11.
Results
Among the 130 women screened, 123 mothers fulfilled the inclusion criteria and were recruited in this study. Of the 123 women screened, 72 were diagnosed to have PPB, accounting for 58.5% prevalence rate. Most of the mothers were literate (91%) and housewives (77%). About 9% of the mothers had previous history of miscarriage and 8% had a history of psychiatric illness. Two mothers had marked suicidal tendency (by EPDS).
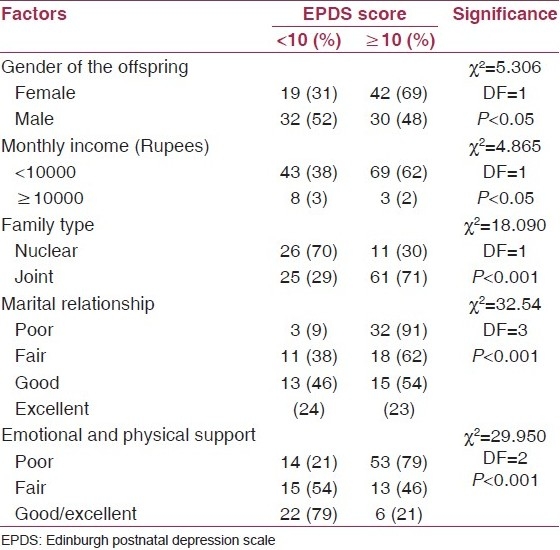
EPDS score of 10 and above was seen in mothers with female offspring (69%, P<0.05), low family income (62%, P=0.05), and living in joint family (71%, P<0.001). Poor marital relationship (91%, P<0.001) and deficit of emotional-physical support (P<0.001) were also associated with PPB.
However, previous psychiatric illness, abortion, and obstetric complications did not have significant association with PPB in this study [Table 1].
Table 1.
Correlation between various factors and EPDS score
Discussion
In India, the occurrence rate of PPB is in the range of 50–60%(8) and the prevalence of PPB in this study is found to be 58.5%. The rates vary depending on the screening techniques used and the type of study population.(9,10) Evidences from literature indicate higher rates of depression on using the EPDS for screening.(11)
Many women tend to hide the postpartum stress and bear it in silence due to the social stigma associated with this disorder.(12) There is 2- to 3-fold higher occurrence of the depressive symptoms among mothers within 5 weeks after delivery.(13)
This study demonstrates strong and consistent associations between many demographic and sociocultural variables and the PPB. Gender bias of the infants is a deep rooted cultural aspect existing in India, especially among the economically backward communities.(14) This study reveals this fact by showing that as high as 69% of the baby blue mothers are the ones who had given birth to female child. Mothers who are already having a girl child have a greater possibility of developing mental disorder because there are high expectations for a male child in the present conception.(6) There was remarkable association between family income and the baby blue. The baby blue was considerably high in mothers from low-income category (62%). It is obvious that the entry of a new member to an already economically struggling family could create enormous stress. Therefore, family planning counseling can be of important not only for spacing but also for economy management of the family. In a general Indian family setup, women are expected to stay with the in-laws and other family members with whom they face more stress.(15) This may be the probable reason accounting for 71% baby blue mothers from joint families. It is evident from this study that unhealthy marital relationship is the outstanding risk factor for PPB (91%). Lack of emotional and physical support from the family was another vital risk factor recognized in this study which is in consensus with previous studies.(16) On the contrary, mothers with history of psychiatric illness and obstetric complications(17) did not give any significant association. Despite the fact that the literature often presents conflicting details regarding the etiology of postpartum mood disorders,(18) the physicians and the healthcare professionals are expected to identify the problem at the early stages and provide primary assistance. The early detection of this disorder is highly essential as it might affect the parenting abilities of mother and ultimately affecting the infant's cognitive health.(19) This was a cross-sectional study, and follow-up studies with intervention would be remarkable.
Conclusion
Postpartum mood disturbances are the outcome of several sociocultural pressures faced by the women. Hence, these can be used as the indicators for early diagnosis of PPB and to initiate preventive measures.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Seyfried LS, Marcus SM. Postpartum mood disorders. Int Rev Psychiatry. 2003;15:231–42. doi: 10.1080/0954026031000136857. [DOI] [PubMed] [Google Scholar]
- 2.Hapgood CC, Elkind GS, Wright JJ. Maternity blues: Phenomena and relationship to later postpartum depression. Aust N Z J Psychiatry. 1988;22:299–306. doi: 10.3109/00048678809161211. [DOI] [PubMed] [Google Scholar]
- 3.Burt VK. Mood disorders in women: Focus on postpartum. Womens Health Psychiatry. 2006;2:6–12. [Google Scholar]
- 4.Beck CT. Postpartum depression predictors inventory-revised. Adv Neonatal Care. 2003;3:47–8. doi: 10.1053/adnc.2003.50014. [DOI] [PubMed] [Google Scholar]
- 5.Patel V, Rodrigues M, DeSouza N. Gender, poverty and postnatal depression; a study of mothers in Goa. Am J Psychiatry. 2002;159:43–7. doi: 10.1176/appi.ajp.159.1.43. [DOI] [PubMed] [Google Scholar]
- 6.Alvarado-Esquivel C, Sifuentes-Alvarez A, Salas-Martinez C, Martínez-García S. Validation of the Edinburgh postpartum depression scale in a population of puerperal women in Mexico. Clin Pract Epidemiol Ment Health. 2006;29(2):23. doi: 10.1186/1745-0179-2-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Prabhu TR, Ashokan TV, Rajeswari A. Postpartum psychiatric illness. J Obstet and Gynaecol of India. 2005;55:329–332. [Google Scholar]
- 8.Vera M, Alegría M, Freeman D, Robles RR, Ríos R, Ríos CF. Depressive symptoms among Puerto Ricans: Island poor compared with residents of the New York City area. Am J Epidemiol. 1991;134:502–10. doi: 10.1093/oxfordjournals.aje.a116122. [DOI] [PubMed] [Google Scholar]
- 9.Beeghly M, Olson KL, Weinberg MK, Pierre SC, Downey N, Tronick EZ. Prevalence, stability, and socio-demographic correlates of depressive symptoms in Black mothers during the first 18 months postpartum. Matern Child Health J. 2003;7:157–68. doi: 10.1023/a:1025132320321. [DOI] [PubMed] [Google Scholar]
- 10.Teissedre F, Chabrol H. A study of the Edinburgh Postnatal Depression Scale (EPDS) on 859 mothers: Detection of mothers at risk for postpartum depression. Encephale. 2004;30:376–81. doi: 10.1016/s0013-7006(04)95451-6. [DOI] [PubMed] [Google Scholar]
- 11.Kennedy H, Beck C, Driscoll J. A light in the fog: Caring for women with postpartum depression. J Midwifery Womens Health. 2002;47:318–30. doi: 10.1016/s1526-9523(02)00272-6. [DOI] [PubMed] [Google Scholar]
- 12.Cox JL, Murray D, Chapman G. A controlled study of the onset, duration and prevalence of postnatal depression. Br J Psychiatry. 1993;163:27–31. doi: 10.1192/bjp.163.1.27. [DOI] [PubMed] [Google Scholar]
- 13.Cohen A. Excess female mortality in India: The case of Himachal Pradesh. Am J Public Health. 2000;90:1369–1371. doi: 10.2105/ajph.90.9.1369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chandran M, Tharyan P, Muliyil J, Abraham S. Post-partum depression in a cohort of women from a rural area of Tamil Nadu, India. Incidence and risk factors. Br J Psychiatry. 2002;181:499–504. doi: 10.1192/bjp.181.6.499. [DOI] [PubMed] [Google Scholar]
- 15.Suri R, Burt VK, Altshuler LL, Zuckerbrow-Miller J, Fairbanks L. Fluvoxamine for postpartum depression. Am J Psychiatry. 2001;158:1739–40. doi: 10.1176/appi.ajp.158.10.1739. [DOI] [PubMed] [Google Scholar]
- 16.McCoy SJ, Beal JM, Shipman SB, Payton ME, Watson GH. Risk factors for postpartum depression: A retrospective investigation at 4-weeks postnatal and a review of the literature. Am Osteopath Assoc. 2006;106:193–198. [PubMed] [Google Scholar]
- 17.Wood AF, Thomas SP, Droppleman PG, Meighan M. The downward spiral of postpartum depression. MCN Am J Matern Child Nurs. 1997;22:308–16. doi: 10.1097/00005721-199711000-00007. [DOI] [PubMed] [Google Scholar]
- 18.Stuart S, Couser G, Schilder K, O’Hara MW, Gorman L. Postpartum anxiety and depression: Onset and co-morbidity in a community sample. J Nerv Ment Dis. 1998;186:420–4. doi: 10.1097/00005053-199807000-00006. [DOI] [PubMed] [Google Scholar]
- 19.Stuart S, Couser G, Schilder K, O’Hara MW, Gorman L. Postpartum anxiety and depression: Onset and co-morbidity in a community sample. J Nerv Ment Dis. 1998;186:420–424. doi: 10.1097/00005053-199807000-00006. [DOI] [PubMed] [Google Scholar]


