Abstract
Parathyroid carcinoma is a very rare cause of primary hyperparathyroidism. Pre-operative diagnosis remains a challenge. We report a case referred for a suspicious goiter with a poor general condition associated with hypercalcemia. Cytological findings attributed it to a possible parathyroid neoplasm that must be considered in the differential diagnosis of a nodular thyroid mass by the cytopathologist. Serum parathormone levels were correlated and the patient underwent surgery. Histopathology confirmed the diagnosis of parathyroid carcinoma. There can be a major pitfall, as it may appear indistinguishable from a benign adenoma.
Keywords: Hypercalcemia, hyperparathyroidism, parathyroid carcinoma
Introduction
Parathyroid carcinoma is one of the rare causes of primary hyperparathyroidism accounting for less than 1% of all cases. Eighty to eighty-five percent have a single adenoma. The signs and symptoms of parathyroid carcinoma are renal stones, bone pains, osteoporosis, abdominal pain and weight loss. Physical examination may reveal a cervical mass and the biochemical abnormalities are elevated serum calcium and parathormone levels. A case of parathyroid carcinoma is being presented because of its rarity and possible cytological and histological diagnostic dilemmas and pitfalls.
Case Report
A 35-year-old male presented in our hospital with neck swelling, generalized weakness, progressive exertional dyspnea, abdominal discomfort, reduced appetite and weight loss for 1 year. On clinical examination, a mass was palpable in the thyroid gland region along with pallor. Cardiovascular examination showed a systolic murmur. Routine laboratory studies on admission revealed Hb- 8.7 gm/dL with an otherwise normal peripheral blood count. Urea- 84 mg/dL, Creatinine- 2.7 mg/dL, alkaline phosphatase- 980 U/dL. Other parameters of liver function tests were not significant. Computed tomography (CT) scan showed a right-sided cervical mass in the thyroid measuring 3.7 × 2.5 cm pushing the trachea to the left. Fine needle aspiration cytology (FNAC) was advised with suspicion of a malignant lesion [Figure 1].
Figure 1.

CT scan showing right-sided cervical mass pushing the trachea to the left
CT-guided FNAC smears from the mass were highly cellular with round to oval cells that exhibited a stippled or granular nuclear chromatin with moderate pleomorphism [Figure 2]. The cells were predominantly arranged in two-dimensional cohesive groups. There were also many single cells and bare/naked nuclei around the groups. Absence of colloid and macrophages raised significant suspicion of a parathyroid neoplasm, as opposed to a follicular neoplasm, and serological and histological correlation was advised.
Figure 2.
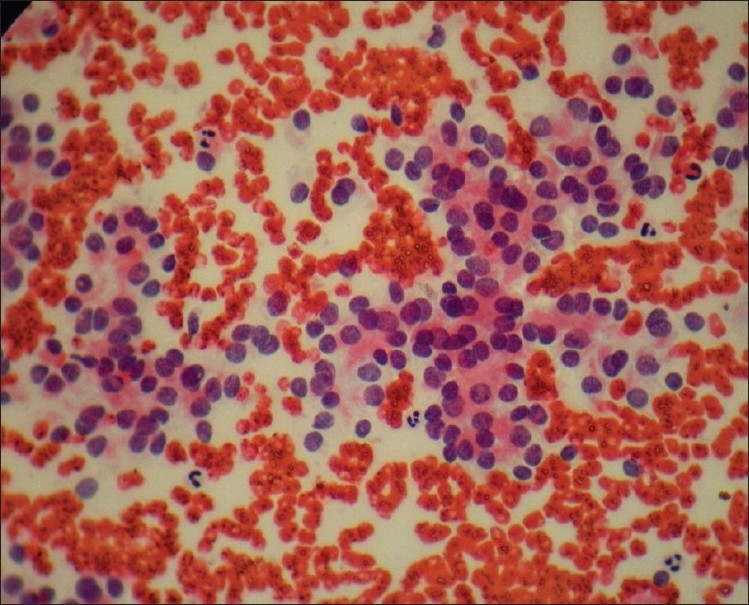
Guided aspirate showing highly cellular smear with stippled nuclear chromatin and moderate pleomorphism. Cells are arranged predominantly in cohesive groups with many single cells/naked nuclei. Absence of colloid and macrophages noted (Pap, ×400)
Further corroborative investigations were done. Serum calcium was raised to 13.1 mg/dL. Radiographs of both hands showed osteopenia of phalanges with sub-periosteal bone resorption of middle phalanges and erosion of tufts of terminal phalanges. Skull radiograph showed osteopenia with fine osteolytic lesions scattered within calvaria (salt pepper appearance). Kidney-ureter-bladder (KUB) radiography exhibited bilateral nephrocalcinosis. Ultrasonography (USG) of the abdomen showed bilateral contracted kidneys with nephrocalcinosis, mild hepatomegaly and ascites. Serum parathormone level was found to be markedly raised, 212 pg/ mL (normal range: 12-72 pg/mL). No evidence of metastatic disease could be found at initial presentation.
The patient was treated for control of hypercalcemia and the mass was surgically resected. On cut section it revealed a hard, encapsulated appearing but adherent grey-white lesion measuring 3.5 × 2.5 × 2 cm with focal areas of hemorrhage. Histopathology showed a cellular tumor divided into nodules by broad fibrous bands [Figure 3]. The tumor cells were arranged in trabecular and pseudo-rosette pattern separated by thin blood vessels showing monomorphic round to ovoid nuclei and clear cytoplasm; brisk mitoses were present (8 per 10 hpf). No definite capsular invasion could be demonstrated on thorough sectioning.
Figure 3.
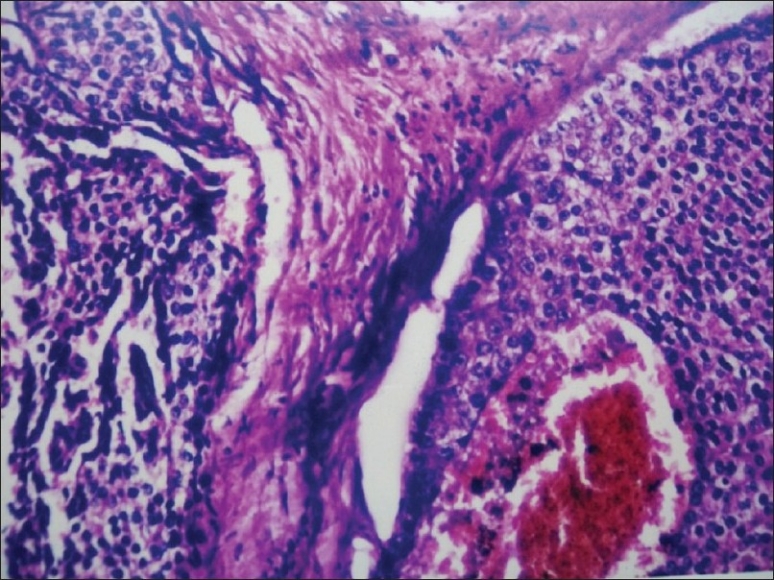
Histological section showing a cellular tumor divided into nodules by fibrous bands (H and E, ×100)
The patient was followed up in the surgical, medical and endocrinology outpatient departments and later reported with increase in ascites and CT findings of liver metastasis within 1 year. He was treated conservatively and succumbed to his disease in the following months.
Discussion
Carcinoma of parathyroid gland is suspected clinically if there is a raised serum calcium and parathormone level with a palpable mass in the neck. Diagnosis of parathyroid carcinoma is usually established on pathological criteria. The Wynne study recorded polydipsia/polyuria in 38%, myalgia/arthalgia in 27%, palpable neck mass was present in 14% and asymptomatic patients were 7%.[1] The etiology is unknown in most cases although several genetic defects have been reported. Mutations of the HRPT2 gene (1q 25-31) cause hyperparathyroidism jaw tumor syndrome, and about 15% of these patients develop parathyroid cancer.[2] The gene codes for a tumor suppressor protein called parafibromin.
Although there is significant overlap in the cytomorphologic features of cells derived from parathyroid and thyroid gland, the presence of cohesive cell groups, stippled nuclear chromatin, prominent vascular proliferation with attached epithelial cells, and frequent occurrence of single cells with naked nuclei are useful clues that favor parathyroid origin.[3] The absence of colloid or macrophages and lack of monolayered sheets and microfollicles also point toward parathyroid etiology. Cytopathologist performed guided FNAC can distinguish between parathyroid and thyroid nodules in patients with suspected parathyroid lesions.[4] However, they cannot be used to distinguish normal parathyroid from hyperplasia, adenoma or carcinoma[5] although some studies have suggested otherwise.[6]
As is the case with many endocrine neoplasms, the histopathological distinction between benign and malignant parathyroid tumors is difficult. In 1973, Shantz and Castleman[7] established a set of criteria for the diagnosis of this malignancy. These histological features are: 1) uniform sheets of (usually chief) cells arranged in a lobular pattern separated by dense fibrous trabeculae, 2) capsular or vascular invasion and 3) mitotic figures within tumor parenchymal cells that must be distinguished from endothelial cell mitoses. Unfortunately, none of these are pathognomonic as several features have occasionally been found in parathyroid adenomas.[8]
Parathyroid carcinomas may have such bland cytological appearance that nothing but the invasiveness of the tumor can differentiate them from a benign lesion.[9] But capsular invasion is present in only 67% of the parathyroid carcinomas affecting the thyroid gland.[10] When capsular invasion cannot be demonstrated, as per Shantz and Castleman criteria, uniform sheets of cells arranged in a lobular pattern separated by dense fibrous trabeculae and raised mitotic figures within tumor parenchymal cells are considered diagnostic evidence of malignancy. Parathyroid adenomas usually do not have classic dense fibrous bands and mitotic figures (if any) are at the most occasional. Various studies have found focal positivity for neuron specific enolase and chromogranin A in parathyroid carcinomas. However, they do not differentiate between hyperplasia, adenomas and carcinomas.
Parathyroid carcinomas, although rare, must be considered in the differential diagnosis of a nodular thyroid mass. They are often under-diagnosed pre-operatively, resulting in diagnostic dilemmas. Cytological suspicion benefits the patient with proper serological and hormonal assessment and pre-operative management. Diagnosis is confirmed by taking overall clinical, biochemical, radiological, cytological, intra-operative and histopathological features into account.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Wynne AG, van Heerden J, Carney JA, Fitzpatrick LA. Parathyroid carcinoma: clinical and pathological features in 43 patients. Medicine. 1992;71:197–205. [PubMed] [Google Scholar]
- 2.Sharretts JM, Kebebew E, Simonds WF. Parathyroid cancer. Semin Oncol. 2010;37:580–90. doi: 10.1053/j.seminoncol.2010.10.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dimashkieh H, Krishnamurthy S. Ultrasound guided fine needle aspiration biopsy of parathyroid gland and lesions. Cytojournal. 2006;3:6. doi: 10.1186/1742-6413-3-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lieu D. Cytopathologist-performed ultrasound-guided fine-needle aspiration of parathyroid lesions. Diagn Cytopathol. 2010;38:327–32. doi: 10.1002/dc.21203. [DOI] [PubMed] [Google Scholar]
- 5.Abati A, Skarulis MC, Shawker T, Solomon D. Ultrasound-guided fine-needle aspiration of parathyroid lesions: A morphological and immunocytochemical approach. Hum Pathol. 1995;26:338–43. doi: 10.1016/0046-8177(95)90068-3. [DOI] [PubMed] [Google Scholar]
- 6.Halbauer M, Crepinko I, Tomć Brzac H, Simonović I. Fine needle aspiration cytology in the preoperative diagnosis of ultrasonically enlarged parathyroid glands. Acta Cytol. 1991;35:728–35. [PubMed] [Google Scholar]
- 7.Schantz A, Castleman B. Parathyroid carcinoma. A study of 70 cases. Cancer. 1973;31:600–5. doi: 10.1002/1097-0142(197303)31:3<600::aid-cncr2820310316>3.0.co;2-0. [DOI] [PubMed] [Google Scholar]
- 8.Levin KE, Galante M, Clark OH. Parathyroid carcinoma versus parathyroid adenoma in patients with profound hypercalcemia. Surgery. 1987;101:649–60. [PubMed] [Google Scholar]
- 9.Bondeson L, Sandelin K, Grimelius L. Histopathological variables and DNA cytometry in parathyroid carcinoma. Am J Surg Pathol. 1993;17:820–9. doi: 10.1097/00000478-199308000-00007. [DOI] [PubMed] [Google Scholar]
- 10.Evans HL. Criteria for the diagnosis of parathyroid carcinoma.A critical study. Surg Pathol. 1991;4:244–65. [Google Scholar]


