Abstract
Background:
Although autogenous materials have been used in abdominal wall hernioplasty for a long time, the introduction of prosthetic materials diminished their popularity. However, these materials may be expensive, inappropriate or unavailable. The aim of this study is to determine the place of de-epithelialized dermal flap in the reconstruction of abdominal wall hernias.
Materials and Methods:
A five-year prospective, descriptive analysis of eligible patients with difficult abdominal wall hernias closed with de-epithelialized dermal flap in a Nigerian Tertiary Health Institution, from January 2001 to December 2005.
Results:
Over the five-year period, 37 patients were recruited into the study. There were 11 males and 26 females, giving a male: female ratio of 1: 2.4. The ages ranged from 8 months to 47 years (mean = 12.6 years). The defects consisted of 15 incisional hernias, 12 intermuscular/inferior lumbar hernias, nine healed exomphalos major and two giant umbilical hernias. The size of the hernia defects ranged from 4.5 cm to13cm (mean = 6.4 cm). Three patients had bowel resection and end-to-end anastomosis, in addition to the flap reconstruction. Morbidity was minimal and included skin dimpling in 11 patients, seroma in three, and wound infection in two patients. Neither recurrence of herniation nor mortality was recorded during the period of follow-up, which ranged from three months to 4.5 years (mean = nine months).
Conclusion:
The results suggest that this is a useful technique that can easily be applied in many centers with minimal resources. It is cheap, effective and associated with minimal morbidity.
Keywords: Abdominal wall hernias, de-epithelialized dermal flap, hernioplasty
INTRODUCTION
The abdominal wall is a complex fascio-muscular structure[1] whose defects could result from congenital or acquired causes.[2] Two common considerations in the surgical management of giant abdominal wall hernias include care of the excessive skin (which could result in skin ulceration/infection before surgery) and closure of the fascial defect (which could result in recurrence after surgery). Although the former could easily be overcome, the later remains as a considerable surgical reconstructive challenge.[2–4] The use of autogenous materials in the reconstruction of such difficult defects has a long history,[5] but the advent of prosthetic materials diminished their popularity.[2,6–11] However, in certain instances, the use of these (prosthetic) materials may be inappropriate or fraught with unavailability and high cost.[2,12] In the developing countries, the difficulty in managing such patients is further compounded by poverty, ignorance and neglect, leading to late presentation.[12] In this article, we report our experience in the use of de-epithelialized dermal flap, a method that utilizes the excess local skin for the reconstruction of the defective fascia, in 37 consecutive patients with difficult abdominal wall hernias. To the best of the authors’ knowledge, this method of hernioplasty using autogenous material has not previously been described. It is presented to highlight the operative technique as well as to stimulate further research in this area.
MATERIALS AND METHODS
Thirty-seven patients with difficult abdominal hernias had hernioplasty using the de-epithelialized dermal flap in a prospective study during the five-year period, from January 2001 to December 2005 at our hospital. The study included all patients that consented to surgery, and whose hernias were considered (pre- or intra-operatively) unsuitable for direct closure [Figure 1], or those who have had recurrence(s) following such previous repair(s). Appropriate biochemical, hematological, microbiological and radiological investigations were carried out on all patients. All patients had conventional three-day bowel preparation and perioperative broad-spectrum antibiotics when necessary. Where the patient was found to be obese, weight reduction measures were instituted preoperatively. Postoperative analgesia was by parenteral pentazocine, which was later converted to oral non-steroidal anti-inflammatory agents (NSAIDS). Patients were observed for possible postoperative complications, including recurrences. Follow-up was at the surgical outpatient clinic and through the use of telephones where possible.
Figure 1.

A child with a huge right inferior lumbar hernia, containing significant amount of his abdominal viscera
Operative technique
All procedures were carried out under general (intubation) anesthesia in an appropriate position. Skin preparation and draping followed known standards. Incision was placed at the summit of the swelling [Figure 2] to raise two flaps of skin. Where a previous scar existed, such was excised as much as possible. The hernia sac was then opened [Figure 3], care being taken to avoid injury to the underlying viscera. The contents of the sac were then reduced and the size of the defect was determined [Figure 4]. In a few instances where some contents could not be reduced due to lack of space, or where a faecal fistula existed [Figure 5], the appropriate segment of the bowel was excised and end-to-end anastomosis effected. One of the skin flaps (usually the lower one in the case of a transverse incision) is flipped over the defect to determine the site that lies directly over the fascial defect [Figure 6]. The skin over this area of the flap is then de-epithelialized [Figure 7], using a scalpel or ordinary razor blade (sterilized with antiseptic solution). The excess part of the flap is then trimmed out, leaving only the de-epithelialized portion [Figure 8], which is then sutured continuously [Figures 9 and 10] to the margin of the defect (using an appropriately sized monofilament nylon), starting from one end of the base of the flap. The peritoneum over the second flap is then dissected [Figures 4 and 6] in order to create a raw surface that will stay over the sutured de-epithelialized flap. This flap is also trimmed to size so that it could be sutured to the margin of the first flap. The wounds were drained by vacuum drains, while interrupted or continuous non-absorbable sutures were applied to the skin [Figure 11]. Suture removal was between seven to ten days.
Figure 2.
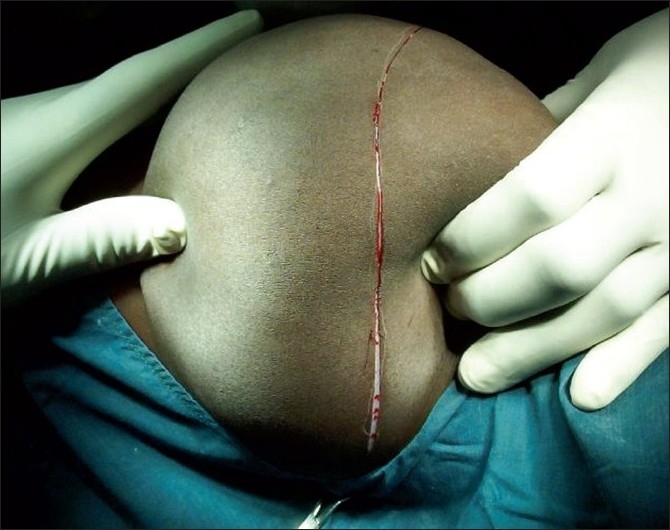
Same patient in Figure 1 showing incision on the summit of the hernia, to obtain two flaps of skin
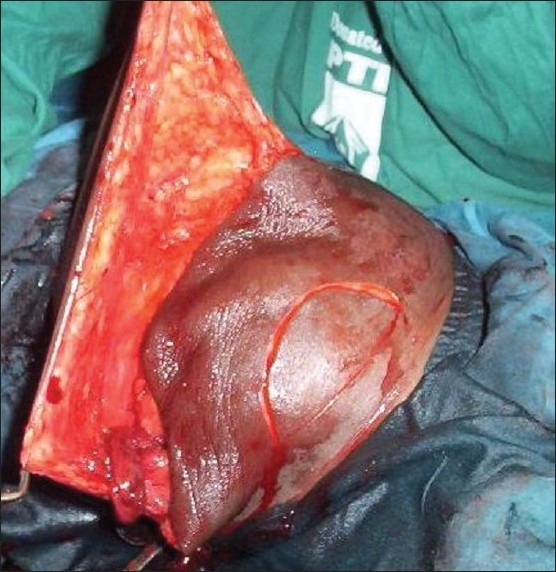
Figure 3.
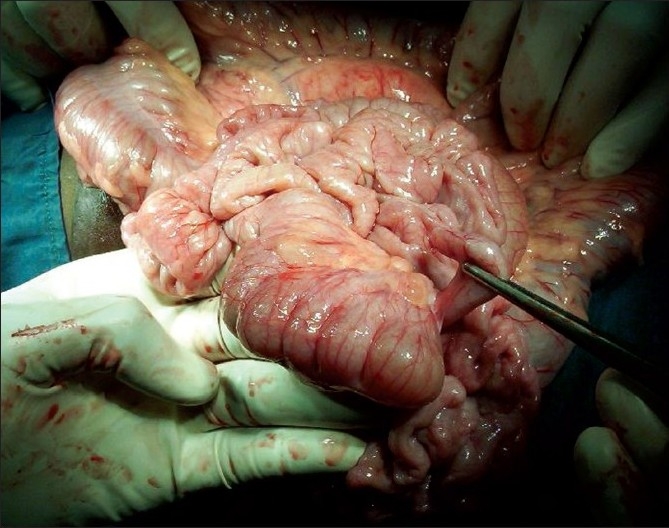
Hernia sac opened to display its contents; in this case, the entire small and large bowel (same patient as in Figure 1)
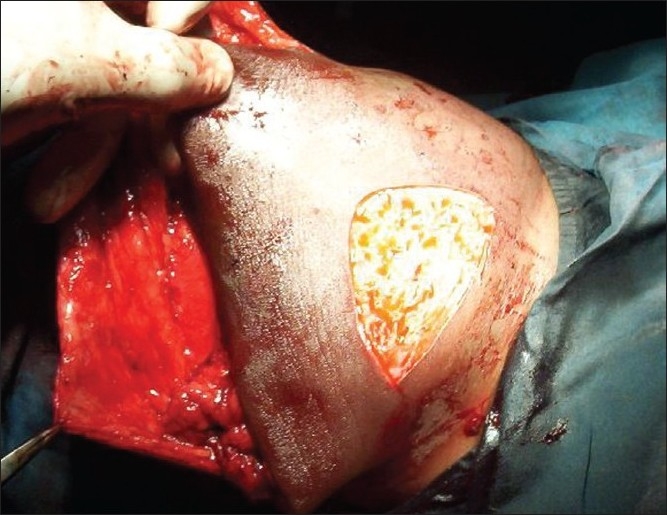
Figure 4.
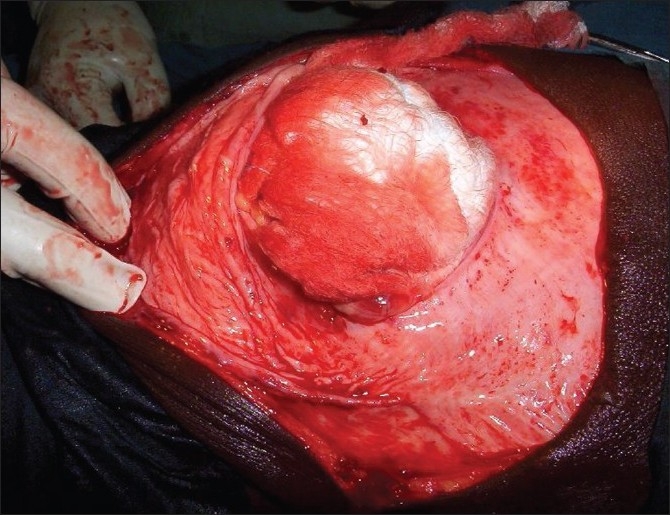
Contents of the sac have been reduced (and covered with abdominal pack) to demonstrate the size of the defect (same patient as in Figure 1). Here the hernia sac has not been dissected
Figure 5.

Same patient on follow-up, six weeks after surgery
Figure 6.
Incision on one flap of skin to mark the area to be deepithelialized (same patient in Figure 1). Note that the hernia sac (peritoneum) has been dissected out from the other flap of skin
Figure 7.
The appropriate portion of skin flap has been de-epithelialized (same patient in Figure 1). The excess skin flap around the deepithelialized portion will be excised
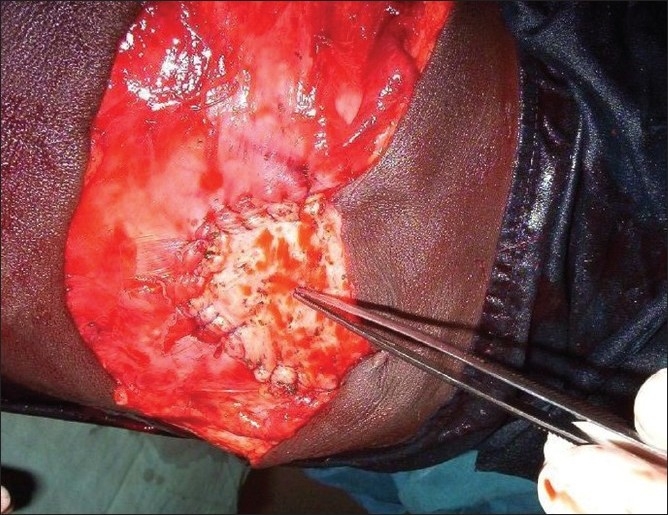
Figure 8.
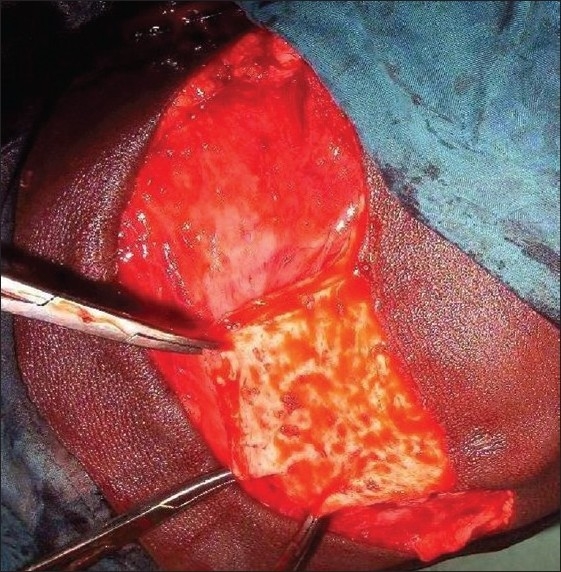
The de-epithelialized flap (held with forceps) is here demonstrated, after the excess skin around it has been excised (same patient as in Figure 1)
Figure 9.
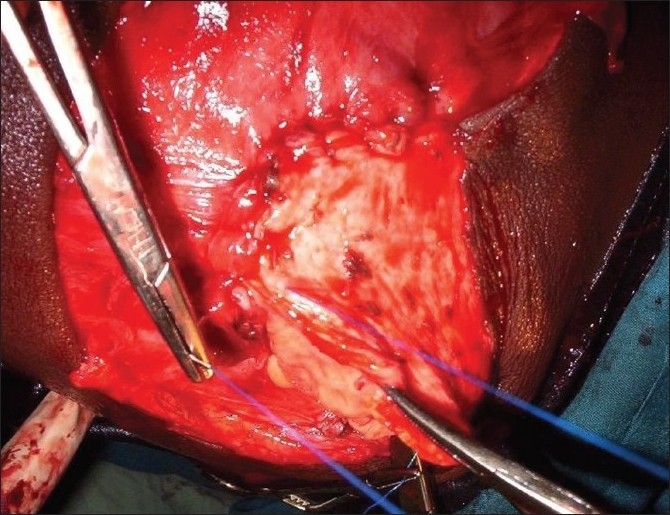
The de-epithelialized flap is sutured to the margin of the defect, starting with the pedicle, using a non-absorbable suture (same patient as in Figure 1)
Figure 10.
Suturing has been completed. The sutured flap is shown by the forceps (same patient as in Figure 1)
Figure 11.
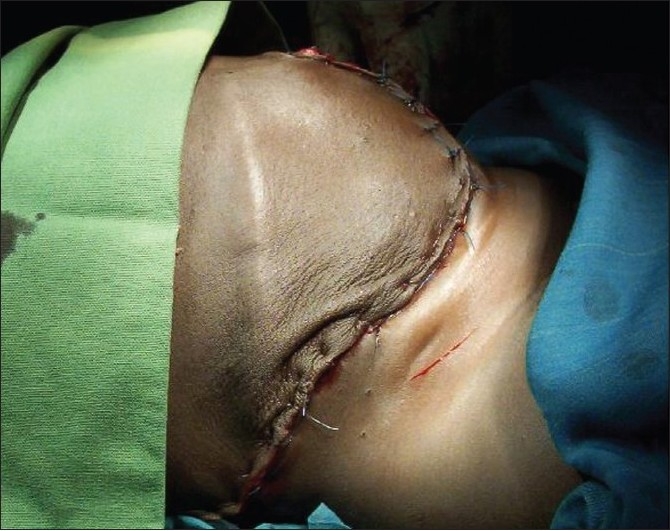
Immediate postoperative outlook, skin closed over a vacuum tube drain (same patient as in Figure 1)
RESULTS
A total of 37 patients had their hernias repaired using this method during the five-year period. There were 11 males and 26 females, giving a male: female ratio of 1: 2.4. The ages ranged from 8 months to 47 years (mean = 12.6 years). The defects consisted of 15 incisional hernias, 12 intermuscular/inferior lumbar hernias, nine healed exomphalos major and two giant umbilical hernias. The co-morbid pathologies included skin ulcerations [Figure 12] in nine patients, obesity in three (all females) and entero-cutaneous fistulae [Figure 12] in two patients. The size of the hernia defects ranged from 4.5 cm to 13 cm (mean = 6.4 cm). Three patients had bowel resection and end-to-end anastomosis, in addition to the flap reconstruction. Morbidity was minimal and included skin dimpling in 11 patients, seroma in three, and wound infection in two patients. Duration of hospital stay ranged from 8 to 17 days (mean = 11 days). Neither recurrence of herniation nor mortality was recorded during the period of follow-up, which ranged from three months to 4.5 years (mean = nine months).
Figure 12.

A middle-aged woman with recurrent incisional hernia following cesarian section. Note the skin ulcerations and enterocutaneous fistula
DISCUSSION
In most cases of abdominal wall hernias, primary direct closure of the defect can be achieved. However, where the defect is wide or significant viscera is contained in the hernia sac, such reduction and repair might proof unsuccessful, resulting in bowel obstruction, splinting of the diaphragm, impaired mesenteric and inferior vena caval flow, and gangrene of the bowel.[2,13–15] Several techniques have been devised to minimize this problem, but with limited effectiveness. Notable among these is the use of pre-operative pneumoperitoneum, which not only expands the peritoneal cavity, but also the hernia sac. Direct closure and hemi-phrenic nerve crush or post-operative paralysis (with ventilatory support) could be very expensive and faced with respiratory complications.[14,15]
Several methods of conventional open and laparoscopic repair of difficult hernias are available. Similarly, several prosthetic materials are in use in the reconstructive armamentarium of the abdominal wall,[16] including materials made from nylon, teflon, prolene, and marlex. The difference lies in their foreign body reactivity and hence in their adhesive potential[16]. Autogenous tissues, and newer modifications of prosthetic meshes, have been shown to prevent these complications.[16–18] Dermal grafts, fascia lata grafts and vascularized grafts based on the thigh muscles have been used for long.[2] Our de-epithelialized dermal flap (DDF) utilizes local skin and obviates the need to operate at two different sites in a patient, as opposed to the use of tissues like fascia lata.
The effect of pressure on the usually redundant skin, and the resultant necrosis that results, accounted for skin ulcerations in nine out of our patients, and entero-cutaneous fistula in another two. It is also two of these patients who had post-operative wound infection, despite the use of peri-operative broad-spectrum antibiotics. Bowel preparation aided the reduction of visceral contents of the sac by significantly reducing the faecal load. It may have also helped in reducing the rate of post-operative wound infection by reducing the luminal microbial load. Three of our patients who were obese at the time of initial consultation had to loose weight before surgery. Apart from cardiovascular complications, Medina et al.[19] noted that patients undergoing herniorrhaphy with body mass index (BMI) above 37 (97.5 percentile) had a six-fold increased risk of surgical wound infection. Most of the incisional hernias we encountered followed failed repairs by direct closure. The DDF is usually available in enough amounts to allow tension-free closure of the musculo-aponeurotic defect. However, limited right hemi-colectomy had to be done in one child in order to allow reduction of the hernial sac contents into the peritoneal cavity without any untoward effect. The other two patients had bowel resection in order to get rid of entero-cutaneous fistula. In our experience, the need for DDF (or prosthetic material) is not related to the size of the defect alone, but also the contents of the sac relative to the volume of the peritoneal cavity. It should be noted that closure of the hernial defect must not take place at the expense of increasing the stretch on the already exhausted stretched aponeurosis.[20]
Being a flap, the survival of DDF does not depend on diffusion of nutrients from peritoneal fluid, as is the case in autogenous grafts. Suturing the base of the flap to the margin of the defect may arguably reduce the blood supply to the flap. If this assertion is true, it may produce an ischemia-induced fibroplastic changes in the flap, simulating the dense fibrotic anterior rectus sheath, similar to what has been observed following the use of tissue expanders in the management of such patients.[4] Drainage of seroma, and treatment of superficial wound infection in the few patients with these complications, did not pose any serious problem in management. Skin dimpling which was observed in some patients after surgery [Figure 11] improved significantly in all patients on follow-up [Figure 5]. As the number of patients in this study is few, and the duration of follow-up in most of them is short, it is difficult to draw definite conclusions. However, the results suggest that this is a useful technique that can easily be applied in many centers with minimal resources. It is cheap, effective and associated with minimal morbidity. To the best of the authors’ knowledge, this is the first report that describes the use of a flap from the redundant skin of a hernial sac, to repair a defective underlying musculo-aponeurotic layer of the abdominal wall. We hope that this will stimulate others who work under similar conditions as ours to conduct further research in this area in order to validate our results.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Moore KL, Dalley AF. Adomen. In: Moore KL, Dalley AF, editors. Clinically oriented anatomy. 5th ed. Williams and Wilkins: Lipincott; 1999. pp. 192–354. [Google Scholar]
- 2.Adebamowo CA, Oluwatosin O. Anterior abdominal wall reconstruction with fascia lata. West Afr J Med. 2001;20:231–3. [PubMed] [Google Scholar]
- 3.Towne BH, Peters G, Chang JH. The problem of “giant” omphalocoele. J Pediatr Surg. 1980;15:543–8. doi: 10.1016/s0022-3468(80)80770-6. [DOI] [PubMed] [Google Scholar]
- 4.Verlende P, Zoltie N. A new surgical approach to exomphalos. Br J Plast Surg. 1990;43:241–3. doi: 10.1016/0007-1226(90)90169-z. [DOI] [PubMed] [Google Scholar]
- 5.Dennis C, Equist IF. Strangulated external hernia. In: Nyhus LM, Condon RE, editors. Hernia. 2nd ed. Philadelphia: Lipincott Company; 1978. [Google Scholar]
- 6.Temudom T, Siadati M, Sarr MG. Repair of complex giant or recurrent ventral hernias by using tension free intraperitoneal prosthetic mesh (Stoppa Technique): lesson learned from our initial experience (fifty patients) Surgery. 1996;120:738–44. doi: 10.1016/s0039-6060(96)80025-0. [DOI] [PubMed] [Google Scholar]
- 7.Carbajo MA, Martín del Olmo JC, Blanco JI, de la Cuesta C, Toledano M, Martin F, et al. Laparoscopic treatment vs.open surgery in the solution of major incisional and abdominal wall hernias with mesh. Surg Endosc. 1999;13:250–2. doi: 10.1007/s004649900956. [DOI] [PubMed] [Google Scholar]
- 8.Luijendijk RW, Hop WC, van den Tol MP, de Lange DC, Braaksma MM, IJzermans JN, et al. A comparison of suture repair with mesh repair for incisional hernia. N Engl J Med. 2000;6:392–8. doi: 10.1056/NEJM200008103430603. [DOI] [PubMed] [Google Scholar]
- 9.Arroyo A, García P, Pérez F, Andreu J, Candela F, Calpena R. Randomized clinical trial comparing suture and mesh repair of umbilical hernia in adults. Br J Surg. 2001;88:1321–3. doi: 10.1046/j.0007-1323.2001.01893.x. [DOI] [PubMed] [Google Scholar]
- 10.LeBlanc KA, Whitaker JM, Bellanger DE, Rhynes VK. Laparoscopic incisional and ventral hernioplasty: Lessons learned from 200 patients. Hernia. 2003;7:118–24. doi: 10.1007/s10029-003-0117-1. [DOI] [PubMed] [Google Scholar]
- 11.Chelala E, Gaede F, Douillez V, Dessily M, Alle JL. The suturing concept for laparoscopic mesh fixation in incisional and ventral hernia. Hernia. 2003;7:191–6. doi: 10.1007/s10029-003-0143-z. [DOI] [PubMed] [Google Scholar]
- 12.Atimomo CE. Management of giant umbilical hernia in an adult Nigerian. Nig Med Pract. 1996;31:91–3. [Google Scholar]
- 13.Bruce J, Afshani E, Karp MP, Jewett TC., Jr Omphalocele with pyloroduodenal obstruction by extrinsic hepatic compression: A case report. J Pediatr Surg. 1988;23:1018–20. doi: 10.1016/s0022-3468(88)80012-5. [DOI] [PubMed] [Google Scholar]
- 14.Nakayama DK, Mutich R, Motoyama EK. Pulmonary dysfunction after primary closure of an abdominal wall defect and its improvement with bronchodialators. Pediatr Pulmonol. 1992;12:174–80. doi: 10.1002/ppul.1950120309. [DOI] [PubMed] [Google Scholar]
- 15.Carlton GR, Towne BH, Bryan RW, Chang JH. Obstruction of the suprahepatic inferior vena cava as a complication of giant omphalocele repair. J Pediatr Surg. 1979;14:733–4. doi: 10.1016/s0022-3468(79)80255-9. [DOI] [PubMed] [Google Scholar]
- 16.Golash V. Laparoscopic geometrical repair of ventral hernia. Surgeon. 2006;4:33–8. doi: 10.1016/s1479-666x(06)80019-3. [DOI] [PubMed] [Google Scholar]
- 17.Klosterhalfen B, Klinge U, Schumpelick V. Functional and morphological evaluation of different polypropylene-mesh modifications for abdominal wall repair. Biomaterials. 1998;19:2235–46. doi: 10.1016/s0142-9612(98)00115-x. [DOI] [PubMed] [Google Scholar]
- 18.Welty G, Klinge U, Klosterhalfen B, Kasperk R, Schumpelick V. Functional impairment and complaint following incisional hernia repair with different polypropylene meshes. Hernia. 2001;5:141–7. doi: 10.1007/s100290100017. [DOI] [PubMed] [Google Scholar]
- 19.Medina M, Sillero M, Martínez-Gallego G, Delgado-Rodríguez M. Risk factors of surgical wound infection in patients undergoing herniorrhaphy. Eur J Surg. 1997;48:169–79. [PubMed] [Google Scholar]
- 20.Ascar OM. Recent observations upon paraumbilical and epigastric hernias. Surg Clin North Am. 1984;64:315–33. doi: 10.1016/s0039-6109(16)43288-3. [DOI] [PubMed] [Google Scholar]