Abstract
Ultrasound is a modality now available to all physicians and can help in making rapid decisions, particularly with critically ill patients. This article reviews the basis of the use of sonography for the diagnosis of pneumothorax.
Keywords: Ultrasound, pneumothorax, trauma
INTRODUCTION
Pneumothoraces (PTXs) are among the most common life-threatening thoracic injuries. While still used and recommended as a screening modality, supine anteroposterior chest radiography (CXR) is insensitive for the detection of PTXs, with reported sensitivities approximating 50%.[1] Advances in the imaging of trauma patients, particularly the increased use of both computed tomography (CT) and thoracic ultrasonography (US), have led to increased rates of identification of PTXs and a new radiologic entity called occult pneumothoraces (OPTXs). Initially defined as a PTX not suspected on the basis of either clinical examination or plain radiograph, but subsequently detected with a CT (thoracic and/or abdominal),[1] the incidence of OPTXs in the trauma population is 2–17% according to the most recent published review.[1]
The implementation of thoracic US in the initial assessment of injured patients has led some authors to expand the definition of OPTX to include patients with PTX occult to the CXR but identified on US.[1] While the optimal management of these OPTXs is still a matter of debate,[1,2] all agree that thoracic US provides a method of rapidly detecting PTXs that would have been missed if only supine CXRs were obtained or diagnosed in a delayed fashion if CT scans were obtained in all patients.[3] Thoracic US possesses the advantages of portability, repeatability, absence of radiation, ease of use and high sensitivity in the detection of PTX.[4] A growing number of publications now support its use as part of the initial assessment of the trauma patient in combination with the FAST exam, giving rise to the term EFAST: The extended focused assessment with sonography for trauma.[4]
Physiology of PTXs and physics of air detection
A PTX is a collection of air in the pleural space resulting in non-apposition of the visceral and parietal pleura. The direct depiction of a PTX by US is not possible due to the high acoustic impedance of air which causes almost complete reflectance of sound waves.[5] Instead, the diagnosis of a PTX will be based on the absence of signs usually found when the parietal and visceral pleura are in apposition.
Patient position, transducer type and placement
When the time and situation permits, a comprehensive bilateral thoracic examination that includes all available lung surfaces, including posterior, is felt to offer information comparable to CT scan in expert hands.[6] Practically however, to assess for a PTX in most critical situations, the patient will be supine. As the pleura and its movements are the focus of this exam, we prefer a high frequency linear transducer for best depiction of the relatively superficial pleura, recognizing that microconvex transducers have been described to give a better appreciation of lung artifacts that emanate across the field such as true B-line type comet-tail artifacts.[6] The most practical location to initially place the transducer will be at the second or third intercostal space on the mid-clavicular line, the transducer being parallel to the spine.[7] Both lungs should always be examined, starting with the one perceived most likely to have a normal exam.
Ultrasonographic signs of normal pleural apposition
Lung sliding
Normal respiration results in gliding of the visceral pleura against the parietal pleura. This is observed via US as a sliding movement typically best appreciated near the lung bases. This physiologic sign can be visually enhanced by the use of the color power doppler mode and the M-mode functions. Lung sliding (LS) being a dynamic process requiring real-time imaging and real-time interpretation, the color power doppler function allows a single still image to depict this dynamic process.[3,8] When evaluating normal lung without a pneumothorax, there will be a flow signal at the thoracopleural interface corresponding to the sliding movement of the visceral and parietal pleura. M-mode, which displays motion of anatomical structures in time, also enables the evaluator to depict LS as a static image. Normal pleural movement will generate an image described as the seashore sign. This “seashore” appearance results from the motionless chest wall anteriorly, represented by linear waves, and the motion of the lung posteriorly, depicted as a homogenous granular pattern [Figure 1].
Figure 1.
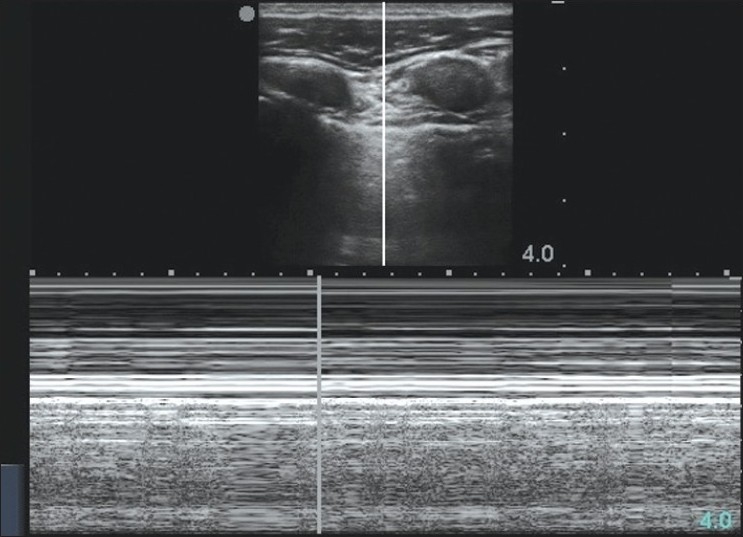
M-mode depiction of the “seashore” appearance that results from the motionless chest wall anteriorly, represented by linear waves, and the motion of the lung posteriorly, depicted as a homogenous granular pattern
Comet tail artifacts: B-lines and Z-lines
Comet tail artifacts (CTAs)[9] are reverberations depicted as vertical echoic lines extending from the pleura into the lung tissue and are synchronized with LS. Dr. Lichtenstein[10] has made a distinction between B-lines and Z-line types of CTAs. B-lines are believed to arise from distended water-filled interlobular septae under the visceral pleural and therefore both pleural surfaces have to be in apposition to be visualized. B-lines always extend to the bottom of the US viewing screen, erasing the A-Line, and may be enhanced, either focally or diffusely, in certain pathologic conditions with increased lung water-content such as pulmonary contusion, edema and ARDS.[7] These lines will move with lung sliding. Z-lines, however, are a “parasitic” type of reverberating CTA also originating from the pleural surface and creating small reverberations that do not extend to the bottom of the US viewing screen and do not erase the A-Line. While Z-lines are clinically unhelpful and devoided of pathologic meaning,[10] B-lines are almost always meaningful and form the basis of diagnosing a variety of alveolar-interstitial syndromes, an exploding topic beyond the scope of this review.[11] The A-line referred to is a horizontal artefact corresponding to subpleural air, and originates from the parietal pleura. This air may be free beneath the parietal pleural (PTX – no sliding) or contained within normal visceral pleura and lung (No PTX sliding present) and does not confidently discriminate a PTX from a normal lung, but may be relatively “hyperlucent” with a true PTX. The A-line is basically the line we look for when evaluating lung sliding.
Ultrasonographic signs of pneumothorax
As described earlier, the non-apposition of the visceral and parietal pleura in a PTX prevents the ultrasound probe from detecting LS and CTA. The absence of LS will also result in the absence of color power signal at the thoraco-pleural interface as long as the transducer is held in a fixed location for this aspect of the examination.[8] When using the M-mode, the seashore sign noted in the presence of normal lung apposition is replaced by the stratosphere sign, an image composed of only horizontal lines due to the absence of movement of the chest wall coupled to the non-detection of LS [Figure 2]. While the absence of LS alone is not specific to the presence of a pneumothorax and can be found in other pathologic conditions (pleural adhesions; pulmonary infiltrates, contusions, ARDS; atelectasis and mainstem intubation), the absence of both of these signs strongly suggests a pneumothorax, and warrants either a search for a confirmatory lung point or intervention, depending on the clinical urgency.
Figure 2.
M-mode depiction of the “stratosphere sign”, an image composed of only horizontal lines due to the absence of movement of the chest wall coupled to the non-detection of LS
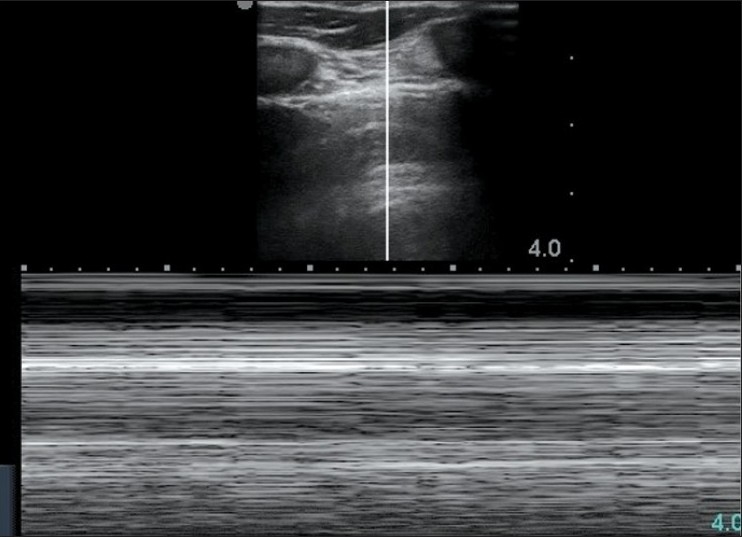
Another US sign that assists in confirming the presence of a PTX, and perhaps quantify its importance, is the lung point sign[12] or partial-sliding sign.[13] The explanation supporting this technique is that lung volume increases in inspiration and decreases in expiration. In that regard, when considering a potential PTX, there should be a point where the lung comes in contact with the chest wall in inspiration and not in expiration and at that particular location, the ultrasound image will alternate between LS and no LS or, in M-mode, between the seashore and stratosphere signs [Figures 1 and 2]. It must be emphasized, however, that often with the most clinically urgent PTXs, large amounts of intra-pleural air will completely separate the pleural surfaces, and the lung point only becomes visible as the situation improves with decompression. This series confirms the clinical diagnosis [Figures 3–5, and Supplementary †Videos 1–3].
Figure 3.
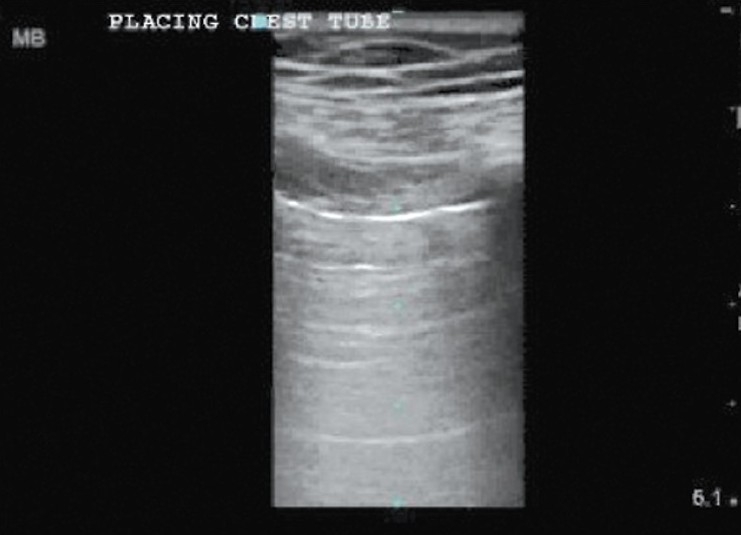
Bedside thoracic ultrasound examination of a 70 year old man who had an acute hypoxemic deterioration while on mechanical ventilation at 16:27 noting absent lung sliding (†video 1)
Figure 5.

Bedside thoracic ultrasound examination of a 70 year old man after decompressing the chest at 16:30 and noting the return of lung sliding (†video 3)
Figure 4.

Bedside thoracic ultrasound examination of a 70 year old man while decompressing the chest at 16:29 noting the partial egress of air and visualization of the lung point sign (†video 2)
Finally, due to the presence of intra-pleural air, it will not be possible to identify B-lines in the presence of a PTX. It is important to differentiate B-line and Z-line type CTAs since Z-lines can be identified despite a PTX[10] but not B-Lines. Mistaking Z-lines for B-lines could result in decreased sensitivity of the US exam for the diagnosis of a PTX.
Accuracy of thoracic ultrasonography for the diagnosis of PTXs
Bedside thoracic US to detect PTXs has a high sensitivity and specificity when performed by an experienced operator. Sodati et al. reported in 2007[14] a blinded, multicentric, observational study of 109 chest and/or multitrauma patients where chest US had a sensitivity and specificity of 92% and 99.4% in diagnosing PTX when compared to CT. Using the lung point evaluation along multiple intercostal spaces, US was adequate in locating the lateral limit of each PTX. In 2005, Lichenstein published a retrospective study of 200 consecutive ICU patients and determined the sensitivity and specificity of the absence of LS for the diagnosis of OPTX to be 100% and 78% respectively.[10] The finding of the lung point had a sensitivity of 79% and a specificity of 100%. Among others, Blaivas et al. also reported a prospective blinded study in 2005 comparing supine CXR and bedside US to CT. Once again, thoracic US had a sensitivity of 98.1% and a specificity of 99.2% for identifying PTXs on the basis of the absence of LS. US also allowed sonologists to differentiate between small, medium, and large PTXs with good agreement with CT results.[15] We believe that real-world performance, however, will likely reflect the pre-test probabilities of PTXs in any population, as well as the operator's experience.[4]
CONCLUSION
Thoracic US is able to rapidly identify PTXs undetected by supine CXR. Studies have shown its high sensitivity, specificity and accuracy in diagnosing PTXs and in quantifying their extension. Despite this reality, the question remains as to how these PTXs observed on US, but not identified on CXR, should best be treated, particularly in mechanically ventilated patients.[1] While further studies on the management of OPTXs are pending, we encourage physicians to incorporate this diagnostic tool in the evaluation of patients, but recommend diligence and clinical correlation in interpreting the significance of the results.[3]
†Videos available on www.onlinejets.org
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Ball CG, Kirkpatrick AW, Feliciano DV. The occult pneumothorax: What have we learned. Can J Surg. 2009;52:E173–9. [PMC free article] [PubMed] [Google Scholar]
- 2.Yadav K, Jalili M, Zehtabchi S. Management of traumatic occult pneumothorax. Resuscitation. 2010;81:1063–8. doi: 10.1016/j.resuscitation.2010.04.030. [DOI] [PubMed] [Google Scholar]
- 3.Kirkpatrick AW, Gillman LM, Chun R, Ball CG, Lall R, Dunham M. Opening Pandora's box: The potential benefit of the expanded FAST exam is partialy confounded by the unknowns regarding the significance of the occult pneumothorax. Crit Ultrasound J. 2010;1:117–22. [Google Scholar]
- 4.Kirkpatrick AW, Sirois M, Laupland KB, Liu D, Rowan K, Ball CG, et al. Hand-held thoracic sonography for detecting post-traumatic pneumothoraces: The Extended Focused Assessment with Sonography for Trauma (EFAST) J Trauma. 2004;57:288–95. doi: 10.1097/01.ta.0000133565.88871.e4. [DOI] [PubMed] [Google Scholar]
- 5.Kirkpatrick AW. Clinician-performed focused sonography for the resuscitation of trauma. Crit Care Med. 2007;35(5 Suppl):S162–72. doi: 10.1097/01.CCM.0000260627.97284.5D. [DOI] [PubMed] [Google Scholar]
- 6.Lichtenstein D. Whole Body Ultrasonography in the Critically Ill. Heidelberg: Springer; 2010. Introduction to lung ultrasound; pp. 117–27. [Google Scholar]
- 7.Killu Keith, Dulchavsky Scott A. The ICU Ultrasound Pocket Book. 1st edition. USA: Detroit; 2010. Coba Victor; pp. 176–85. [Google Scholar]
- 8.Cunningham J, Kirkpatrick AW, Nicolaou S, Liu D, Hamilton DR, Lawless B, et al. Enhanced recognition of “lung sliding” with power color doppler imaging in the diagnosis of pneumothorax. J Trauma. 2002;52:769–71. doi: 10.1097/00005373-200204000-00029. [DOI] [PubMed] [Google Scholar]
- 9.Lichtenstein D, Mezière G, Biderman P, Gepner A. The comet-tail artifact: An ultrasound sign ruling out pneumothorax. Intensive Care Med. 1999;25:383–8. doi: 10.1007/s001340050862. [DOI] [PubMed] [Google Scholar]
- 10.Lichtenstein DA, Mezière G, Lascols N, Biderman P, Courret JP, Gepner A, et al. Ultrasound diagnosis of occult pneumothorax. Crit Care Med. 2005;33:1231–8. doi: 10.1097/01.ccm.0000164542.86954.b4. [DOI] [PubMed] [Google Scholar]
- 11.Ball CG, Ranson MK, Rodriguez-Galvez M, Lall R, Kirkpatrick AW. Sonographic depiction of posttraumatic alveolar-interstitial disease: The hand-held diagnosis of a pulmonary contusion. J Trauma. 2009;66:962. doi: 10.1097/TA.0b013e3180600949. [DOI] [PubMed] [Google Scholar]
- 12.Lichtenstein D, Mezière G, Biderman P, Gepner A. The “lung point”: An ultrasound sign specific to pneumothorax. Intensive Care Med. 2000;26:1434–40. doi: 10.1007/s001340000627. [DOI] [PubMed] [Google Scholar]
- 13.Sargsyan AE, Hamilton DR, Nicolaou S, Kirkpatrick AW, Campbell MR, Billica RD, et al. Ultrasound evaluation of the magnitude of pneumothorax: A new concept. Am Surg. 2001;67:232–6. [PubMed] [Google Scholar]
- 14.Soldati G, Testa A, Sher S, Pignataro G, La Sala M, Silveri NG. Occult traumatic pneumothorax: Diagnostic accuracy of lung ultrasonography in emergency department. Chest. 2008;133:204–11. doi: 10.1378/chest.07-1595. [DOI] [PubMed] [Google Scholar]
- 15.Blaivas M, Lyon M, Duggal S. A prospective comparison of supine chest radiology and bedside ultrasound for the diagnosis of traumatic pneumothorax. Acad Emerg Med. 2005;12:844–9. doi: 10.1197/j.aem.2005.05.005. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


