Abstract
Background:
Percutaneous nephrolithotomy is a routine endourologic procedure in patients with renal stones. Although it is less painful than open surgery, good postoperative analgesia is required to alleviate pain around nephrostomy tube.
Materials and Methods:
Sixty ASA grade I patients, 18 to 60 years of age, of either sex were randomized to receive 20 ml of 0.25% bupivacaine (group S) or 20 ml of normal saline (group C) through 23-gauge spinal needle along the nephrostomy tube under fluroscopic guidance at the end of the surgery. Postoperative pain score was assessed by visual and dynamic visual analog scores. When the scores were ≥4, rescue analgesia was given in the form of tramadol 1 mg/kg i.v. upto maximum 400 mg in 24 hours. Time to first demand analgesia and total dose of tramadol in first 24 hours was noted.
Results:
Pain scores at rest and during coughing as well as rescue analgesic requirements for first 24 hours were significantly less in the bupivacaine group than those of the control group (P < 0.05). The first request for demand analgesia was around 9 hours in group S, while in group C it was around 2.6 hours (P < 0.05). Total requirement of tramadol in group S was 119.3 mg and in C group it was 276.8 mg (P < 0.05).
Conclusion:
Peritubal infiltration of 0.25% bupivacaine is efficient in alleviating postoperative pain after PCNL.
Keywords: Percutaneous nephrolithotomy, postoperative analgesia, peritubal block
Introduction
Percutaneous nephrolithotomy (PCNL) is today the gold standard for the management of patients with renal calculi as it is less invasive than the open surgery, less time consuming, and is associated with less chances of infection. It is also associated with lower morbidity and faster recovery. However, placement of nephrostomy tube results in distressing peritubal pain requiring administration of analgesia. Inadequate analgesia can result in delayed mobilization, impaired ventilation, and prolonged hospitalization, which increases cost. Tubeless PCNL can avert this problem but can be performed only in the selected patients. Analgesics such as non-steroidal anti-inflammatory drugs and opioids have side effects and limiting their use in patients with potential renal problems. Skin infiltration with local anesthetic has not proven very effective after PCNL; however, infiltration of renal capsule has shown to facilitate painless insertion of nephrostomy tube.[1] We hypothesized that peritubal infiltration from renal capsule to skin would alleviate postoperative pain after PCNL. We investigated the analgesic efficacy of peritubal infiltration of 0.25% bupivacaine, under fluoroscopic guidance, after PCNL.
Materials and Methods
A prospective randomized double blind study was conducted in 60 American society of anaesthesiology grade I-II patients posted for PCNL surgery after informed consent and ethical committee's approval. They were randomly divided in two equal groups, group S or study group (0.25% bupivacaine infiltration) and group C or control group (normal saline infiltration), of 30 patients.
All the patients were aged between 18 and 60 years with body mass index BMI less than 35. Exclusion criteria included patients requiring supracostal puncture or more than one puncture or patients having excessive intraoperative bleeding, stone size >2.5 cm, and duration of surgery >3 hours.
On the day of surgery, all patients were premedicated with intravenous glycopyrolate 0.004 mg/kg and fentanyl 2.0 μg/ kg. Balanced general anesthesia was given. Analgesia in the form of opioids or NSAIDs was avoided during the entire procedure. At the end of the procedure but prior to extubation, a 23-gauge spinal needle was passed along the nephrostomy tube (22- 24 Fr) under fluroscopic guidance (to confirm the direction of the needle along the nephrostomy tube) so as to puncture the renal capsule at 6 o′clock position and 12 o′clock position. At each site, 10 ml of 0.25% bupivacaine in group S and 10 ml of normal saline in group C was infiltrated along renal capsule, muscle, subcutaneous tissue, and skin. Trachea was extubated with the patients in supine position and patients were transferred to postanesthesia care unit (PACU). Postoperative pain was assessed by visual analogue scale (VAS) (score between 0 and 10) at rest and during deep breathing and coughing (DVAS- dynamic visual analogue scale score between 0 and 10) by an independent observer blinded to infiltration, at 0 hours, every half hour for 2 hours, every 2 hour for 6 hours, and every 4 hour till 24 hours. In visual analogue scale, 0 means no pain and 10 means maximum untolerable pain. When the score was ≥4, intravenous tramadol was given in dose of 1 mg/kg as a rescue analgesic up to 24 hours. The total dose of tramadol was restricted to 400 mg in 24 hours. The duration of peritubal block was taken as the time from infiltration to first demand for rescue analgesic. The total requirement of tramadol within 24 hours and any side effects such as nausea, vomiting, and sedation were observed.
Statistical analysis was performed using SPSS version 12. Data are expressed as mean with 95% confidence intervals (CIs) for continuous variable. Comparisons of continuous variables were compared using independent t-test with two tail significance. Categorical variables were compared using chi-square tests. “P” value < 0.05 was considered significant.
Results
The demographic data were comparable and similar [Table 1]. Figure 1 shows the VAS at rest, while Figure 2 shows DVAS during coughing and deep breathing. Both were significantly low, i.e., <4 in the immediate postoperative period and remained low for a prolonged period, i.e., around 9 hours in the study group than that of the control group. The first demand of analgesia in study group was at 9.08 hours, while it was 2.66 hours in control group (P < 0.05) [Table 2]. Total consumption of tramadol in study group was 119.3 mg, which was significantly lesser than in that of the control group (276.8 mg) (P < 0.05). The side effects such as nausea and vomiting were also less in study group than in the control group, but the difference was nonsignificant (P > 0.05) [Table 2].
Table 1.
Demographics
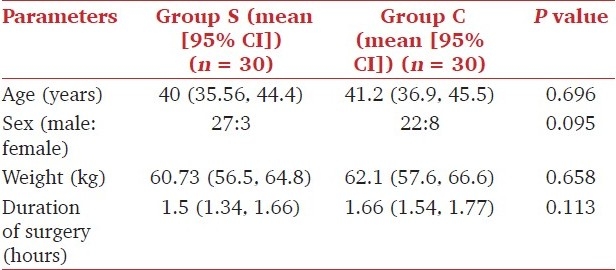
Figure 1.
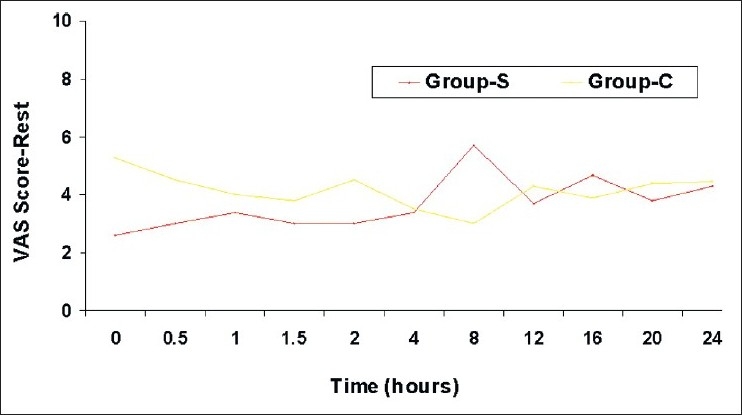
Mean VAS pain scores at rest
Figure 2.
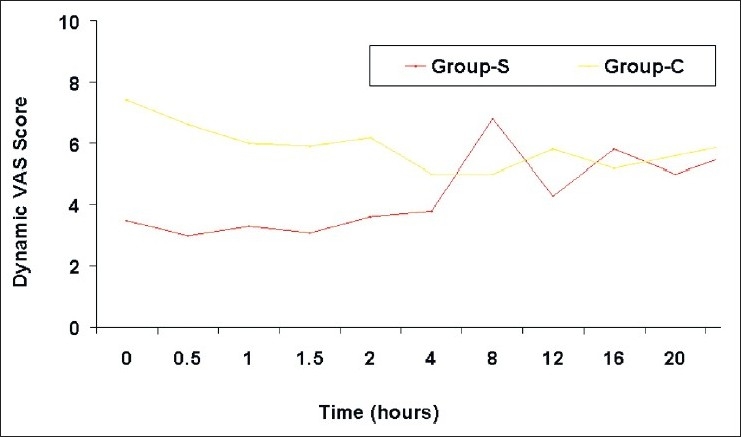
Mean dynamic VAS pain score
Table 2.
Comparison of analgesic efficacy and side-effects between two groups

Discussion
Pain is an unpleasant sensory and emotional experience associated with the actual or potential tissue damage which can result in an increase in the sympathetic response of the body with subsequent rise in heart rate, cardiac work, oxygen consumption, and respiratory complications. It has been hypothesized that the pain after PCNL surgery, which requires insertion of nephrostomy tube, could be due to structures beyond the skin puncture site like renal capsule. Placement of the nephrostomy tube is the last surgical step in PCNL and it provides hemostasis along the tract, avoids urinary extravasation, and maintain adequate drainage of the kidney. The nephrostomy tube produces local inflammatory reaction which causes the post operative pain and discomfort in PCNL. Dalela et al.[1] performed PCNL under renal capsular block by infiltrating renal capsule with 2% lignocaine. They emphasized that most of the pain during PCNL is felt at the time of dilatation of renal capsule and parenchyma as it is richly innervated by pain conducting neurons . Aravantinos et al.[2] also performed PCNL under assisted local anesthesia in selected patients. They placed a 16 Fr nephrostomy tube under local anesthesia and kept it for 1 week. After infiltration of the tract and renal parenchyma with lignocaine, PCNL was performed later. They found this method safe and effective in selected patients.
Various studies have been done to reduce the pain by reducing the size of the nephrostomy tube or performing tubeless PCNL. The tubeless approach is safe in selected patients with uncomplicated percutaneous procedure and has a low calculus burden. Bellman et al.,[3] Karami et al.,[4] and Lojanapiwat et al.[5] performed tubeless PCNL in 50, 60, and 37 selected patients, respectively, and concluded that tubeless PCNL reduces postoperative patient discomfort, analgesic requirement, hospital stay, and cost to the patient.
Placement of small size nephrostomy tube is another option to reduce pain after PCNL. A small bore (8-12 Fr) nephrostomy tube is preferred in patients in whom the incidence of stent dysuria is likely or who may require percutaneous access for subsequent calculus manipulation, while conventional large bore nephrostomy tube drainage may be reserved for procedures with a large complex calculus, significant bleeding, prolonged procedure, infected calculi, or major perforations. In our institute, it is routine pass a nephrostomy tube of 22-24 Fr in size in all PCNL patients. Desai et al.[6] did comparative study of type of nephrostomy drainage following PCNL, i.e., large bore (20 Fr) versus small bore (9 Fr) versus tubeless PCNL. Large bore nephrostomy tube patients had significantly higher analgesic requirement (218 mg of diclofenac sodium) than small bore and tubeless patients (140 and 88 mg of diclofenac sodium, respectively). Pietrow et al[7] used 10 Fr and 22 Fr catheter for drainage after PCNL in 30 patients. They found lower pain score in immediate postoperative period with less narcotic requirement in small drainage catheter after PCNL.
The other modalities of pain relief after PCNL are subcutaneous infiltration, tract infiltration, systemic analgesics, etc. Halebian et al.[8] studied subcutaneous infiltration of 1.5 mg/kg, of 0.25% bupivacaine in 25 patients. Their results showed reduced rescue analgesia requirement but no significant difference in VAS score and pain relief around nephrostomy site area after PCNL. Ugras et al.[9] assessed the effect of local anesthetic infiltration on postoperative pain status and pulmonary functions using either 0.2% ropivacaine or saline into renal puncture site, nephrostomy tract, and skin. Patients received parental metamizol (500 mg/dose) on demand. Their results showed that the combination of ropivacaine instillation with metamizol decreased pain and analgesic use and improved peak expiratory flow more than the use of metamizol alone. Gokten et al.[10] studied the efficacy of the levobupivacaine infiltration to nephrostomy tract in combination with intravenous paracetamol on postoperative analgesia in patients of PCNL and concluded that levobupivacaine infiltration through the nephrostomy tract in combination with intravenous paracetamol infusion was safe and effective as an analgesia method after PCNL.
We observed that infiltration of 0.25% bupivacaine in skin, subcutaneous tissue, nephrostomy tract, and renal capsule significantly reduced VAS and DVAS, prolonged the time to demand analgesia, and reduced consumption of rescue analgesic for first 24 hours. Our results are in accordance with the study by Jonnavithula et al.[11] except that in their study duration of block was prolonged in both control as well as study group and the total consumption of tramadol in 24 hours was also less as compared to our study. This difference was probably related to small nephrostomy tube size (14-16 Fr) used by them compared to large nephrostomy tube (22-24 Fr) used in our study.
Conclusion
Peritubal local anesthetic infiltration with bupivacaine is efficacious in providing postoperative analgesia after PCNL as judged by significant reduction in pain score at rest and on movement, prolongation of time to first demand analgesic and reduction in total analgesic requirement during first 24 hours.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Dalela D, Goel A, Singh P, Shankhwar S. Renal capsular block: A novel method performing PCNL under local Anaesthesia. J Endourol. 2004;18:544–6. doi: 10.1089/end.2004.18.544. [DOI] [PubMed] [Google Scholar]
- 2.Aravantinos E, Karatzas A, Gravas S, Tzortzis V, Melekos M. Feasibility of PCNL under assisted local Anaesthesia. Eur Urol. 2007;51:224–8. doi: 10.1016/j.eururo.2006.06.027. [DOI] [PubMed] [Google Scholar]
- 3.Bellman G, Davidoff R, Candella J, Gerspach J, Kurtz S. Tubeless percutaneous renal surgery. J Urol. 1997;157:1578–82. [PubMed] [Google Scholar]
- 4.Karami H, Gholamrezaie H. Totally tubeless percutaneous Nephrolithotomy in selected patients. J Endourol. 2004;18:475–6. doi: 10.1089/0892779041271580. [DOI] [PubMed] [Google Scholar]
- 5.Lojanapiwat B, Soonthornphan S, Wudhikarn S. Tubeless Percutaneous Nephrolithotomy in Selected Patients. J Endourol. 2001;15:711–3. doi: 10.1089/08927790152596299. [DOI] [PubMed] [Google Scholar]
- 6.Desai M, Kukreja R, Desai M, Mhaskar S, Wani K, Patel S, et al. A prospective randomised comparison of type of nephrostomy drainage following percutaneous nephrostomy: Large bore versus small bore versus tubeless. J Urol. 2004;172:565–7. doi: 10.1097/01.ju.0000130752.97414.c8. [DOI] [PubMed] [Google Scholar]
- 7.Pietrow P, Auge B, Lallas C, Santacruz R, Newman G, Albela D. Pain after percutaneous nephrolithotomy: Impect of nephrostomy tube size. J Endourol. 2003;17:411–4. doi: 10.1089/089277903767923218. [DOI] [PubMed] [Google Scholar]
- 8.Halebian GE, Sur RL, Albala DM, Preminger GM. Subcutaneous Bupivacaine infiltration and Postoperative pain perception after PCNL. J Urol. 2007;178:925–8. doi: 10.1016/j.juro.2007.05.025. [DOI] [PubMed] [Google Scholar]
- 9.Ugras M, Ilksen H, Gunen H, Yucel A, Gunes A. Instillation of skin, nephrostomy tract, and renal puncture site with Ropivacaine decreases pain and improves ventilatory function after percutaneous nephrolithotomy. J Endourol. 2007;21:499–503. doi: 10.1089/end.2006.0335. [DOI] [PubMed] [Google Scholar]
- 10.Gokten O, Kilicarslan H, Dogan H, Turker G, Kordan Y. Efficay of Levobupivacaine infiltration to nephrostomy tract in combination with Intraveneous Paracetamol on postoperative Analgesia in percutaneous Nephrolithotomy patients. J Endourol. 2011;25:35–9. doi: 10.1089/end.2010.0346. [DOI] [PubMed] [Google Scholar]
- 11.Jonnavithula N, Pisapati M, Durga P, Krishnamurthy V, Chilumu R, Reddy B. Efficacy of peritubal local Anaesthetic infiltration in Alleviating Postoperative Pain in PCNL. J Endourol. 2009;23:857–60. doi: 10.1089/end.2008.0634. [DOI] [PubMed] [Google Scholar]


