Abstract
Background:
No drug, used as adjuvant to spinal bupivacaine, has yet been identified that specifically inhibits nociception without its associated side-effects.
Aims:
This prospective randomized double-blind study was conducted to evaluate the onset and duration of sensory and motor block as well as perioperative analgesia and adverse effects of dexmedetomidine and magnesium sulfate given intrathecally with 0.5% hyperbaric bupivacaine for spinal anesthesia.
Materials and Methods:
A total of 90 patients classified as American Society of Anesthesiologists status I and II scheduled for lower abdominal and lower limb procedures were prospectively studied. Patients were randomly allocated to receive intrathecally either 15 mg hyperbaric bupivacaine plus 0.1 ml (10 μg) dexmedetomidine (group D, n=30) or 15 mg hyperbaric bupivacaine plus 0.1 ml (50 mg) magnesium sulfate (group M, n=30) or 15 mg hyperbaric bupivacaine plus 0.1 ml saline (group C, n=30) as control. The onset time to reach peak sensory and motor level, the regression time for sensory and motor block, hemodynamic changes and side-effects were recorded.
Statistical Analysis Used:
All statistical analyses were performed using INSTAT for windows. Continuous variables were tested for normal distribution by the Kolmogorov-Smirnov test. Data was expressed as either mean and standard deviation or numbers and percentages. Continuous covariates (age, body mass index and height) were compared using analysis of variance (ANOVA). For the times to reach T10 dermatomes, Bromage 3 scale and the regression of the sensory block to S1 dermatome and Bromage scale 0, one-way ANOVA was used to compare the means. The level of significance used was P<0.05.
Results:
The onset times to reach T10 dermatome and to reach peak sensory level as well as onset time to reach modified Bromage 3 motor block were significantly different in the three groups. The onset time to reach peak sensory and motor level was shorter in group D as compared with the control group C, and it was significantly prolonged in group M. We also found that patients in group D had significant longer sensory and motor block times than patients in group M, which was greater than in the control group C.
Conclusion:
It was found that onset of anesthesia was rapid and of prolonged duration in the dexmedetomidine group (D). However, in the magnesium sulfate group (M), although onset of block was delayed, the duration was significantly prolonged as compared with the control group (C), but to a lesser degree than in the dexmedetomidine group (D). The groups were similar with respect to hemodynamic variables and there were no significant side-effects in either of the groups.
Keywords: Bupivacaine, dexmedetomidine, lower abdominal surgery, magnesium sulfate, spinal anesthesia lower limb surgery
Introduction
Lower abdominal and lower limb surgeries may be performed under local, regional (spinal or epidural) or general anesthesia, but neuraxial blockade is the preferred mode of anesthesia. Spinal block is still the first choice because of its rapid onset, superior blockade, low risk of infection as from catheter in situ, less failure rates and cost-effectiveness, but has the drawbacks of shorter duration of block and lack of postoperative analgesia. In recent years, use of intrathecal adjuvants has gained popularity with the aim of prolonging the duration of block, better success rate, patient satisfaction, decreased resource utilization compared with general anesthesia and faster recovery. Adequate pain management is essential to facilitate rehabilitation and accelerate functional recovery, enabling patients to return to their normal activity more quickly. The quality of the spinal anesthesia has been reported to be improved by the addition of opioids (such as morphine, fentanyl and sufentanil) and other drugs [such as dexmedetomidine (DXM), clonidine, magnesium sulfate (Mg), neostigmine, ketamine and midazolam], but no drug to inhibit nociception is without associated adverse effects.
DXM, a highly selective a-2 agonist drug, is approved as an intravenous sedative and co-analgesic drug. Its use is often associated with a decrease in heart rate and blood pressure.[1] Intrathecal and epidural characteristics of DXM have been studied in animals.[2,3] Most clinical studies about intrathecal a-2 adrenoreceptor agonist are related to clonidine. Kanazi et al.[4] found that 3 μg DXM and 30 μg clonidine are equipotent intrathecally when added to bupivacaine in patients undergoing urology procedures. The same author found that DXM and clonidine significant reduced the onset time of sensory and motor block while its use significantly prolonged the duration of sensory and motor block without serious side-effects.
Antinociceptive of Mg effects appear to be relevant not only to chronic pain[5] but it also determines, in part, the duration and intensity of postoperative pain.[6] These effects are primarily based on the regulation of calcium influx into the cell, i.e. natural physiological calcium antagonism. Mg is a noncompetitive antagonist to NMDA receptors and has the potential to prevent central sensitization from peripheral nociceptive stimulation. Intravenous (i.v.) administration of Mg, even at high doses, is associated with limited passage across the blood–brain barrier.[7] In previous studies, it was demonstrated that intrathecally administered Mg prolonged spinal opioid analgesia both in rats and in humans.[8,9] The addition of Mg to spinal anesthesia improved postoperative analgesia in an orthopedic setting.[10,11] The addition of intrathecal magnesium sulfate (MgSO4) to 10 mg bupivacaine plus 25 μg fentanyl prolonged spinal anesthesia in patients undergoing lower extremity surgery.[11]
Materials and Methods
After obtaining institutional ethical committee approval and written informed consent, 90 ASA physical status I and II patients aged 18–45 years, of either gender, height 160–190 cm and weight 50–90 kg, scheduled for lower abdominal and lower limb surgery under spinal anesthesia were included in this prospective randomized, double-blinded study. Patients with a history of uncontrolled, labile hypertension, patients with allergy to the study drugs, opium addiction, sedative drugs consumption, contraindication for spinal anesthesia, failure of spinal block and the need for general anesthesia were excluded from the study. Patients received no premedication and, upon arrival of patients into the operating room, ECG, pulse oximetry (SpO2) and noninvasive blood pressure (NIBP) were monitored. Following infusion of 500 mL lactated Ringer's solution and with the patient in the sitting position, lumbar puncture was performed at the L3-L4 level through a midline approach using a 25G Quincke spinal needle (Spinocan, B Braun Medical, Melsungen, Germany). Using computer-generated random numbers, patients were allocated into three groups:
Group D received 15 mg hyperbaric bupivacaine and 0.1 ml (10 μg) DXM
Group M received 15 mg hyperbaric bupivacaine and 0.1 ml (50 mg) Mg
Group C received 15 mg hyperbaric bupivacaine and 0.1 ml normal saline as control
After intrathecal injection, patients were positioned in supine position and oxygen 2 L/min was given through a face mask. The anesthesiologist performing the block was blinded to the study drug and recorded the intraoperative data. Sensory block was assessed bilaterally by using analgesia to pin prick with a short hypodermic needle in the midclavicular line. Motor blockade was assessed by using the modified Bromage scale[12] (Bromage 0, the patient is able to move the hip, knee and ankle; Bromage 1, the patient is unable to move the hip but is able to move the knee and ankle; Bromage 2, the patient is unable to move the hip and knee but able to move the ankle; Bromage 3, the patient is unable to move the hip, knee and ankle). The time to reach T10 dermatome sensory block, peak sensory level and Bromage 3 motor block were recorded before surgery. The regression time for sensory and motor block were recorded in a postanesthesia care unit (PACU). All durations were calculated considering the time of spinal injection as time zero. Patients were discharged from the PACU after sensory regression to S1 dermatome and Bromage 0.
The three groups were monitored preoperatively, intraoperatively and during shifting for heart rate, NIBP and SpO 2. Hypotension was defined as systolic blood pressure <90 mmHg or >30% decrease in baseline values. Tachycardia was defined as heart rate >100/min and bradycardia was defined as heart rate <60/min. Intraoperative nausea, vomiting, pruritus, additive analgesia, sedation or any other side-effects were recorded.
Results
There were no differences in age, height, body weight and body mass index (BMI) between the groups [Figure 1]. These groups were similar in the maximal dermatome height achieved. Systolic, diastolic arterial blood pressures, heart rates and oxygen saturations remained stable, and there was no significant difference between the groups.
Figure 1.
Patient characteristics in the three groups. Data are given as mean (SD)
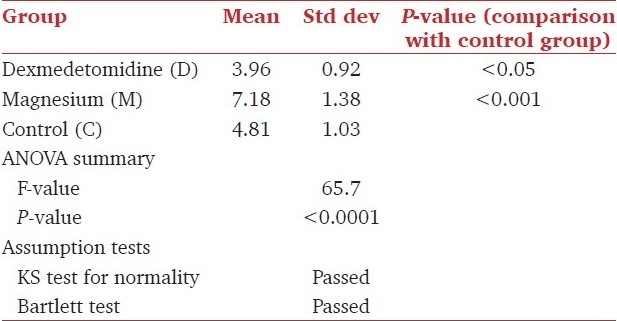
The onset time of block, both sensory up to T10 dermatome and motor to Bromage 3 scale, was rapid in the DXM group D (2.27 ± 1.09 and 3.96 ± 0.92) and delayed in the Mg group M (6.46 ± 1.33 and 7.18 ± 1.38) in comparison with the control group C (4.14 ± 1.06 and 4.81 ± 1.03). The difference between the groups conducted through one-way ANOVA with post tests was statistically significant in both sensory (F=97.118, P<0.0001) and motor (F=65.7, P<0.0001) [Tables 1 and 2].
Table 1.
Onset times of sensory blocks for sample groups
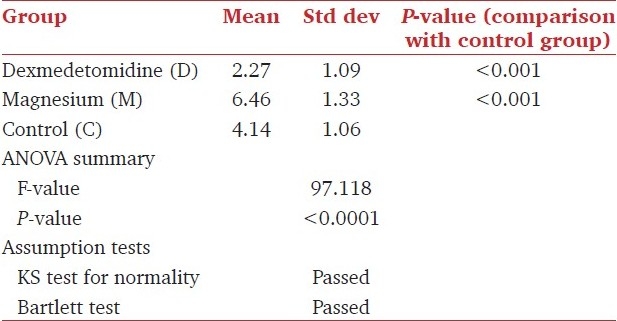
Table 2.
Onset times of motor blocks for sample groups
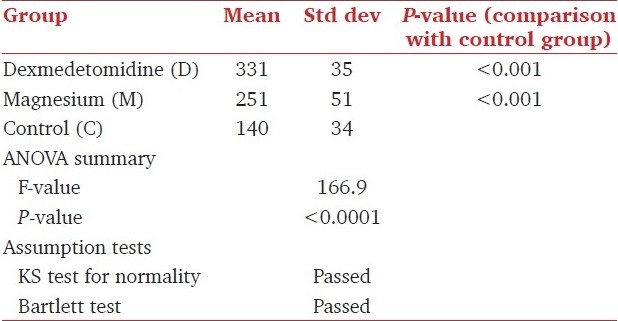
The regression time of block, both sensory up to T10 dermatome and motor to bromage 3 scale, was prolonged in the DXM group D (352 ± 45 and 331 ± 35) and in the Mg group M (265 ± 65 and 251 ± 51) when compared with the control group C (194 ± 55 and 140 ± 34). However, the duration was longest in the DXM group among the three groups. The difference between the groups conducted through one-way ANOVA with post tests was statistically significant in both sensory (F=60.3, P<0.0001) and motor (F=166.9, P<0.0001) [Tables 3 and 4].
Table 3.
Regression times of sensory blocks for sample groups
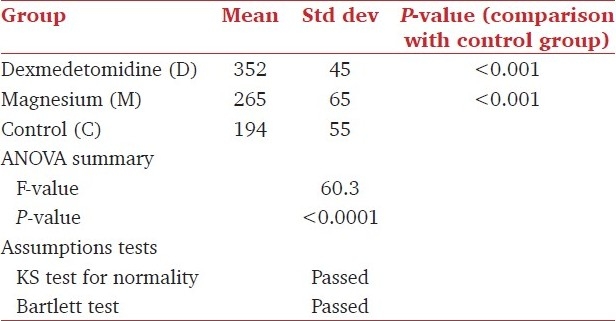
Table 4.
Regression times of motor blocks for sample groups
There was no significant difference in the mean values of heart rate and mean arterial pressures in the first hour after performing the spinal anesthesia and the first hour in the PACU between the three groups. The SpO2 was higher than 95% in all patients in the three groups, either in the intraoperative or in the PACU time. Twenty-four hours and 2 weeks following discharge, follow-up did not show any neurological impairment related to spinal anesthesia such as back, buttock or leg pain, headache or any neurological deficit.
Discussion
DXM reduces opioid and inhalational anesthetic requirements when used intravenously during anesthesia.[13] Compared with clonidine, the affinity of DXM to a-2 receptors has been reported to be 10-times more than clonidine.[14] Kalso et al.[2] and Post et al.[14] reported a 1:10 dose ratio between intrathecal DXM and clonidine in animals. Kanazi et al.[4] found that 3 μg DXM or 30 μg clonidine added to 13 mg spinal bupivacaine equally prolonged the duration of sensory and motor block with minimal side-effects in urologic surgical patients as found in our study also. Intrathecal DXM when combined with spinal bupivacaine prolongs the sensory block by depressing the release of C-fiber transmitters and by hyperpolarization of post-synaptic dorsal horn neurons.[15] Motor block prolongation by a-2 adrenoreceptor agonists may result from binding these agonists to motor neurons in the dorsal horn of the spinal cord.[16] Intrathecal a-2-receptor agonists have antinociceptive action for both somatic and visceral pain.[17] Kanazi et al.[4] found in their study that the supplementation of bupivacaine (12 mg) spinal block with a low-dose DXM (3 μg) produces a significantly shorter onset of motor block and a significantly longer sensory and motor block than bupivacaine alone. The results of Al-Mustafa et al.[18] and Al-Ghanem et al.[19] used higher doses of DXM (5 μg and 10 μg), and found that its effect is dose-dependent and that the onset of sensory block to reach T10 dermatome was shorter with the use of DXM. We had a similar result in our study. We used a higher dose of DXM and a larger volume was injected into the subarachnoid space. The most significant side-effects reported with the use of intrathecal a-2 adrenoreceptor agonists are bradycardia and hypotension. In the present study, these side-effects were not significant probably because we used the drug intrathecally, instead of using the intravenous route.
On the other hand, in the Mg group, it was found that the onset and resolution of motor blockade and the time to attain maximum sensory level were longer. Ozalevli et al. observed a similar delay in onset of spinal anesthesia when adding intrathecal Mg to fentanyl and isobaric bupivacaine (we used hyperbaric bupivacaine in our study).[11] They suggested that the difference in pH and baricity of the solution containing Mg contributed to the delayed onset, which may also be the case in the study by Malleeswaran et al. on mild preeclampsia patients.[20] In our study, there was prolongation of the motor and sensory block, although less than that with intrathecal DXM. Arcioni et al. also observed that intrathecal and epidural Mg potentiated and prolonged motor block.[10] These results are consistent with a previous study conducted in patients undergoing lower extremity surgery during spinal anesthesia, in which the addition of intrathecal Mg (50 mg) to 10 mg bupivacaine plus 50 μg fentanyl prolonged the period of spinal anesthesia.[9] Intrathecal Mg was used in order to increase the analgesic duration of opioids in humans, and they demonstrated that addition of 50 mg intrathecal Mg to intrathecal fentanyl led to better analgesia during painless delivery. These results were comparable with those of animal studies, where intrathecal Mg increased the analgesic time of opioids.[21]
Mg blocks N-Methyl-D-aspartate (NMDA) channels in a voltage-dependent way and produces a dramatic reduction of NMDA-induced currents.[22] Noxious stimulation leads to the release of glutamate and aspartate neurotransmitters, which bind to the NMDA receptor. Activation of these receptors leads to calcium entry into the cell and initiates a series of central sensitization such as wind-up and long-term potentiation in the spinal cord in the response of cells to prolonged stimuli.[23] NMDA receptor signalling may be important in determining the duration of acute pain.[6] Mg blocks calcium influx and noncompetitively antagonizes NMDA receptor channels.[24]
Conclusion
Intrathecal DXM supplementation of spinal block seems to be a good alternative to intrathecal Mg as it produces earlier onset and prolonged duration of sensory and motor block without associated significant hemodynamic alterations. Ten micrograms of DXM as adjuvant to spinal bupivacaine in surgical procedures of long duration has minimal side-effects, and provides excellent quality of postoperative analgesia. Intrathecal Mg also prolongs the duration of spinal analgesia, but this is less than intrathecal DXM and is with a delayed onset. Further studies are required to determine whether larger doses of intrathecal Mg can produce greater potentiation of analgesia and reduce opioid requirements.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Venn RM, Grounds RM. Comparison between dexmedetomidine and propofol for sedation in the intensive care unit: Patient and clinician perceptions. Br J Anaesth. 2001;87:684–90. doi: 10.1093/bja/87.5.684. [DOI] [PubMed] [Google Scholar]
- 2.Kalso E, Poyhia R, Rosemberg P. Spinal antinociceptive by dexmedetomidine, a highly selective 2-adrenergic agonist. Pharmacol Toxicol. 1991;68:140–3. doi: 10.1111/j.1600-0773.1991.tb02052.x. [DOI] [PubMed] [Google Scholar]
- 3.Savola M, Woodley J, Kending J, Maze M. Alpha2B adrenoreceptor activation inhibits nociceptor response in the spinal cord of the neonatal rat. Eur J Pharmacol. 1990;183:740. [Google Scholar]
- 4.Kanazi GE, Aouad MT, Jabbour-Khoury SI, Al Jazzar MD, Alameddine MM, Al-Yaman R, et al. Effect of lowdose dexmedetomidine or clonidine on the characteristics of bupivacaine spinal block. Acta Anesthesiol Scand. 2006;50:222–7. doi: 10.1111/j.1399-6576.2006.00919.x. [DOI] [PubMed] [Google Scholar]
- 5.Tramer MR, Schneider J, Marti RA, Rifat K. Role of magnesium sulfate in postoperative analgesia. Anesthesiology. 1996;84:340–7. doi: 10.1097/00000542-199602000-00011. [DOI] [PubMed] [Google Scholar]
- 6.Woolf CJ, Thompson WN. The induction and maintenance of central sensitization is dependent on N-methyl-d-aspartate acid receptor activation: Implications for the treatment of post-injury pain hypersensitivity states. Pain. 1991;44:293–9. doi: 10.1016/0304-3959(91)90100-C. [DOI] [PubMed] [Google Scholar]
- 7.Ko SH, Lim HR, Kim DC, Han YJ, Choe H, Song HS. Magnesium sulphate does not reduce postoperative analgesic requirements. Anesthesiology. 2001;95:640–6. doi: 10.1097/00000542-200109000-00016. [DOI] [PubMed] [Google Scholar]
- 8.Kroin JS, McCarthy RJ, Von Roenn N, Schwab B, Tuman KJ, Ivankovich AD. Magnesium sulfate potentiates morphine antinociception at the spinal level. Anesth Analg. 2000;90:913–7. doi: 10.1097/00000539-200004000-00025. [DOI] [PubMed] [Google Scholar]
- 9.Buvanendran A, McCarthy RJ, Kroin JS, Leong W, Perry P, Tuman KJ. Intrathecal magnesium prolongs fentanyl analgesia: A prospective, randomized, controlled trial. Anesth Analg. 2002;95:661–6. doi: 10.1097/00000539-200209000-00031. [DOI] [PubMed] [Google Scholar]
- 10.Arcioni R, Palmisani S, Santorsola C, Sauli V, Romano S, Mercieri M, et al. Combined intrathecal and epidural magnesium sulfate supplementation of spinal anesthesia to reduce post-operative analgesic requirements: A prospective, randomized, double-blind, controlled trial in patients undergoing major orthopedic surgery. Acta Anaesthesiol Scand. 2007;51:482–9. doi: 10.1111/j.1399-6576.2007.01263.x. [DOI] [PubMed] [Google Scholar]
- 11.Ozalevli M, Cetin TO, Unlugence H, Guler T, Isik G. The effect of adding intrathecal magnesium sulphate to bupivacaine fentanyl spinal anaesthesia. Acta Anaesthesiol Scand. 2005;49:1514–9. doi: 10.1111/j.1399-6576.2005.00793.x. [DOI] [PubMed] [Google Scholar]
- 12.Bromage PR. A comparison of the hydrochloride and carbon dioxide salts of lidocaine and prilocaine in epidural analgesia. Acta Anesthesiol Scand Suppl. 1965;16:55–69. doi: 10.1111/j.1399-6576.1965.tb00523.x. [DOI] [PubMed] [Google Scholar]
- 13.Martin E, Ramsay G, Mantz J, Sum-Ping ST. The role of the alpha2-adrenreceptor agonist dexmedetomidine in post-surgical sedation in the intensive care unit. J Intensive Care Med. 2000;18:29–34. doi: 10.1177/0885066602239122. [DOI] [PubMed] [Google Scholar]
- 14.Post C, Gordh T, Minor G, Archer T, Freedman J. Antinociceptive effects and spinal cord tissue concentrations after intrathecal injection of guanfacine or clonidine into rats. Anesth Analg. 1987;66:317–24. [PubMed] [Google Scholar]
- 15.Smith MS, Schumbra UB, Wilson KH, Page SO, Hulette C, Light AR, et al. Alpha 2 adrenergic receptor in human spinal cord: Specific localized expression of mRNA encoding alpha-2 adrenergic receptor subtypes at four distinct levels. Brain Res Mol Brain Res. 1995;34:109–17. doi: 10.1016/0169-328x(95)00148-l. [DOI] [PubMed] [Google Scholar]
- 16.Smith C, Birnbaum G, Carter JL, Greenstein J, Lublin FD. Tizanidine treatment of spasticity caused by multiple sclerosis: results of a double-blind, placebo-controlled trial. US Tizanidine Study Group. Neurology. 1994;44:34–43. [PubMed] [Google Scholar]
- 17.Yaksh TL, Reddy SV. Studies in primate on the analgesic effects associated with intrathecal actions of opiates, alpha-adrenergic agonists, and baclofen. Anesthesiology. 1981;54:451–67. doi: 10.1097/00000542-198106000-00004. [DOI] [PubMed] [Google Scholar]
- 18.Al-Mustafa MM, Abu-Halaweh SA, Aloweidi AS, Murshidi MM, Ammari BA, Awwad ZM, et al. Effect of dexmedetomidine added to spinal bupivacaine for urological procedures. Saudi Med J. 2009;30:365–70. [PubMed] [Google Scholar]
- 19.Al-Ghanem SM, Massad IM, Al-Mustafa MM, Al-Zaben KR, Qudaisat IY, Qatawneh AM, et al. Effect of adding dexmedetomidine versus fentanyl to intrathecal bupivacaine on spinal block characteristics in gynaecological procedures-a double blind controlled study. Am J Applied Sci. 2009;6:882–7. [Google Scholar]
- 20.Malleeswaran S, Panda N, Mathew P, Bagga R. Magnesium as an intrathecal adjuvant in mild pre-ecclampsia. Int J Obstet Anesth. 2010;19:161–6. doi: 10.1016/j.ijoa.2009.08.007. [DOI] [PubMed] [Google Scholar]
- 21.Ishizaki K, Sasaki M, Karasawa S, Obata H, Nara T, Goto F. The effect of intrathecal magnesium sulfate on the nociception in rats acute pain models. Anesthesia. 1999;54:241–6. doi: 10.1046/j.1365-2044.1999.00741.x. [DOI] [PubMed] [Google Scholar]
- 22.Liu HT, Hollmann MW, Liu WH, Hoenemann CW, Durieux ME. Modulation of NMDA receptor function by ketamin and magnesium: Part 1. Anesth Analg. 2001;92:1173–81. doi: 10.1097/00000539-200105000-00019. [DOI] [PubMed] [Google Scholar]
- 23.Pockett S. Spinal cord synaptic plasticity and chronic pain. Anesth Analg. 1995;80:173–9. doi: 10.1097/00000539-199501000-00026. [DOI] [PubMed] [Google Scholar]
- 24.Fawcett VY, Haxby EJ, Male DA. Magnesium; physiology and pharmacology. Br J Anaesth. 1999;83:302–20. doi: 10.1093/bja/83.2.302. [DOI] [PubMed] [Google Scholar]


