Abstract
Background & Aims
Colonoscopy is a recommended component of screening for colorectal cancer. We conducted a retrospective study of Medicare data to determine the frequency of anesthesiologist involvement and to identify patient and provider characteristics and cost implications associated with anesthesiologist involvement.
Methods
We used the linked Surveillance, Epidemiology, and End Results Medicare dataset to identify patients without cancer who received a screening colonoscopy examination from July 2001 through 2006 (n=16,268). The outcome variable was anesthesiologist involvement, which was identified by searching Medicare claims. Logistic regression was used to explore the association between patient and provider characteristics and anesthesiologist involvement. Costs associated with the use of an anesthesiologist were derived based on a cost assessment by the Agency for Healthcare Research and Quality.
Results
Of the screening colonoscopies assessed, 17.2% involved an anesthesiologist. The screening colonoscopy rate more than doubled during the study period. The frequency of anesthesiologist involvement increased from 11.0% of screening colonoscopies in 2001 to 23.4% in 2006. Surgeons involved an anesthesiologist in 24.2% of colonoscopies, compared with 18.0% of gastroenterologists and 11.3% of primary care providers. The percentage of colonoscopies that involved an anesthesiologist varied among regions, ranging from 1.6% in San Francisco to 57.8% in New Jersey. Anesthesiologist involvement increased the cost by approximately 20% per screening colonoscopy.
Conclusion
An increase in the involvement of anesthesiologists has significantly increased the cost of screening colonoscopies. Studies are needed to assess the effects of anesthesiologists on risks and benefits of colonoscopy, to determine the most safe and cost-effective approaches.
Keywords: anesthesia, endoscopy, procedure, SEER
Introduction
In the United States, nearly 50,000 people die of colorectal cancer (CRC) each year, the second highest rate of all cancer deaths.1 Screening colonoscopy provides the ability to identify and remove precancerous polyps, and its use as a CRC screening modality continues to rise.2 Screening colonoscopies have been deemed cost effective and are one of the modalities recommended for CRC screening in national guidelines.3–4 Currently, screening colonoscopies are underutilized for a variety of reasons including patient concerns regarding sedation and discomfort during the procedure.5 As a result, there is strong interest in both sedation practices and the involvement of anesthesiologists in screening colonoscopies.
Traditionally, sedation in screening colonoscopies has been provided with midazolam and an opioid.6 Over the past decade, newer options have become available, and based on a nationwide survey distributed in 2004 to the members of the American College of Gastroenterology, approximately one quarter of patients now undergo sedation with propofol instead.7 Because an anesthesiologist usually administers propofol, the involvement of anesthesiologists in screening colonoscopies may be increasingly common. However, little is known about the degree to which anesthesiologists have been involved in recent years. An evaluation of the Medicare population would be beneficial given that Medicare has provided reimbursement for screening colonoscopies since 2001, and Medicare beneficiaries represent a large population of older adults who are eligible for screening colonoscopy.
It is unclear which patient and provider factors are associated with anesthesiologist assistance in screening colonoscopies. A population-level analysis of outpatient colonoscopies performed in Canada demonstrated that patients in low-volume community hospitals were more likely to have anesthesiologist-assisted endoscopy. It was also shown that surgeons were more likely to perform anesthesiologist-assisted endoscopy compared to gastroenterologists.8 However, there still remains a need for an evaluation of patient and provider factors related to anesthesiologist involvement within the United States, both to understand current practice and to help guide future directions relating to the optimal use of anesthesiologist involvement in screening colonoscopies.
Although anesthesiologist involvement has theoretical benefits, including comfort and potentially safety, there is concern about the associated incremental costs. Traditionally, in the absence of an anesthesiologist, there has not been a fee for the sedation of average-risk patients undergoing a screening colonoscopy. Incorporating an anesthesiologist into the colonoscopy, however, results in added costs. More current cost estimates specifically looking at screening colonoscopies in the Medicare population are needed to better understand the financial implications associated with anesthesiologist involvement in screening colonoscopies.
To address these knowledge gaps, we evaluated anesthesiologist involvement in screening colonoscopies in a large population-based sample of Medicare beneficiaries in the United States. Specifically, we assessed overall trends in screening colonoscopy use as well as the proportion with anesthesiologist involvement, patient and provider characteristics, and cost implications associated with anesthesiologist involvement.
Methods
Data Source and Study Sample
We used the National Cancer Institute’s Surveillance, Epidemiology, and End Results (SEER)-Medicare linked database. The SEER database is a premier source for cancer statistics in the United States and provides a compilation of data from geographic areas that represent approximately 28% of the U.S. population.9 The linked SEER-Medicare database provides Medicare claims for patients in the SEER database who are 65 years of age and older. Data is also available for a 5% random sample of Medicare beneficiaries without cancer who reside within the SEER areas.
We derived our cohort from the 5% random sample of Medicare beneficiaries without cancer. For each year 2001 through 2005, we selected all patients aged 68–94 and randomly assigned a month within that year to serve as the patient’s date of entry into the study. Patients who were eligible in multiple years were randomly assigned to one of the years. Because the Medicare reimbursement policy for screening colonoscopy changed in July of 2001, we excluded patients with a start date in the first half of 2001. We then selected patients who received a screening colonoscopy within 2 years of study entry. From this sample, we excluded patients who did not have continuous enrollment in Medicare Parts A and B with fee-for-service coverage from 3 years prior to study entry through the date of screening colonoscopy to ensure they did not have another screening colonoscopy during that time.
To identify screening colonoscopies, we used Healthcare Common Procedure Coding System (HCPCS) and International Classification of Diseases, 9th Revision, Clinical Modification (ICD-9-CM) colonoscopy codes (Appendix 1). We classified a procedure as a screening, rather than diagnostic, if it was performed in an outpatient setting and there were no ICD-9 diagnosis codes for gastrointestinal tract symptoms, weight loss, iron deficiency anemia, alteration in bowel habits, or gastrointestinal bleeding associated with any physician visits within the previous 3 months.10 Patients who had a colonoscopy or sigmoidoscopy within 3 years prior to the procedure date were excluded, as their colonoscopy would be unlikely to be a screening procedure.
Appendix 1.
Healthcare Common Procedure Coding System (HCPCS) and International Classification of Disease, 9th Revision, Clinical Modification (ICD-9-CM) codes used to identify procedures
| Colonoscopy | |
| HCPCS | 44388, 44389, 44392–4, 45378–80, 45382–5 |
| ICD-9-CM | 45.23, 45.25, 45.41–3, 48.36 |
| Codes used to rule out diagnostic colonoscopies | |
| HCPCS | Sigmoidoscopy: G0104, 45300–27, 45330–42, 45345 |
| ICD-9-CM | Abdominal Pain: 787.3, 789, 789.6 |
| Altered Bowel Habits: 564, 787 | |
| GI Bleeding: 578 | |
| Positive fecal occult blood test: 792.1 | |
| Weight loss: 783.2 | |
| Iron Deficiency Anemia: 280 | |
| Anemia Unspecified: 285.9 | |
| Sigmoidoscopy: 45.24, 48.21–4 | |
| Anesthesia | |
| HCPCS | 00740, 00810, 00902 |
| 99100 + HCFASPEC code of 05 or 43 | |
| Colonoscopy code + HCFASPEC code of 05 or 43 |
Construction of Variables
The outcome variable was anesthesiologist involvement, which we identified by searching claims from the day of procedure for the following criteria: 1) HCPCS procedure codes indicating administration of anesthesia; 2) HCPCS codes indicating screening colonoscopy in which the specialty was listed as an anesthesiologist or certified registered nurse anesthetist (CRNA). We determined specialty using the Health Care Financing Administration Specialty (HCFASPEC) variable (Appendix 1).
The operator specialty was recorded and categorized as gastroenterologist, surgeon, primary care provider, or other/unknown, based on HCFASPEC codes. Race categories included white, black, and other. Comorbid conditions were identified by searching claims in the 2 years prior to study entry for diagnosis codes for the conditions used by Elixhauser et al (Appendix 2).11 ICD-9 codes were only included if they were present on at least one inpatient claim or two outpatient or physician claims more than 30 days apart. We created a score representing the number of comorbid conditions each patient had and divided the sample into three groups: 0, 1–2, and ≥3 conditions. As a marker for patient socioeconomic status, we used U.S. Census data to determine the zip code-level median household income for each patient, and this was divided into quintiles. We also explored the setting of service and included the categories of office, ambulatory surgical center, and hospital-based setting.
Appendix 2.
Conditions included in comorbidity index
| Congestive heart failure Arrhythmia Valvular Disease Pulmonary Circulation Fluid and Electrolyte Disorders |
Other Neurological Disorders COPD Diabetes Renal Failure Liver disease Weight Loss |
Lymphoma Metastatic Cancer Solid Tumors without Metastasis Rheumatoid Arthritis Coagulopathy Paralysis |
Deficiency Anemia Alcohol Abuse Drug Abuse Psychoses Depression Vascular Disorders AIDS/HIV |
Data Analysis
The annual screening colonoscopy rate was determined for each year 2001 to 2005. The numerator was the number of patients who received a screening colonoscopy within 1 year of study entry. The denominator was the number of patients who were eligible to be screened at study entry and who had continuous fee-for-service Medicare Parts A and B coverage from study entry until the earliest of the following events occurred: receipt of screening colonoscopy, death, or 1 year after study entry had elapsed. Patients were considered eligible to be screened if they had not received a colonoscopy or flexible sigmoidoscopy in the prior 3 years.
Temporal trends in the percentage of screening colonoscopies with anesthesiologist involvement were evaluated based on the year of the screening colonoscopy. Bivariate logistic regression analysis was used to explore the association between anesthesiologist involvement and patient and provider characteristics including age, sex, race, comorbidity, income registry, and operator specialty. Multivariate logistic regression was then used to identify factors independently associated with anesthesiologist involvement. Of note, the setting of service could not be determined for 9.6% of the claims that either had no setting of service or multiple places of service listed. Therefore, this variable was not included in the full model of identifying factors associated with anesthesiologist involvement.
Costs associated with the use of an anesthesiologist were estimated using a multistep approach. First, we obtained the cost of a colonoscopy without the involvement of an anesthesiologist. Based on a cost assessment by the Agency for Healthcare Research and Quality (AHRQ) published in 2007, the Centers for Medicare and Medicaid Services (CMS) cost reimbursement of a colonoscopy without the involvement of an anesthesiologist ranges from approximately $498 to $649 depending on whether or not a polypectomy or biopsy is performed.12 We identified claims associated with biopsy or polypectomy (Appendix 3) and used the percentage of these claims in our sample to determine the overall average cost per procedure without anesthesiologist involvement. Next, we derived an estimate for the cost of anesthesiologist involvement by selecting all physician claims from the day of the screening colonoscopy for the procedures performed in 2005. Using the anesthesia claims, identified by searching for the HCPCS code 00810 (“anesthesia for lower intestinal endoscopic procedures, endoscope introduced distal to duodenum”), we determined the mean claim payment amount associated with anesthesiologist involvement. Then, we used the total number of screening colonoscopies in our study to derive an estimate for the total number of screening colonoscopies performed nationally during the study period among Medicare fee-for-service beneficiaries. We did this by taking into account our 5% sample of Medicare beneficiaries, so we multiplied our total in our sample by 20. In addition, the SEER data only represents approximately 28% of the United States population,9 so we divided our total by 0.28 to derive our national total of screening colonoscopies. We then used our cost per procedure estimates and multiplied by our total number of procedure estimates to derive national cost estimates both with and without anesthesiologist involvement during the study period.
Appendix 3.
Current Procedural Terminology (CPT) and International Classification of Disease, 9th Revision, Clinical Modification (ICD-9-CM) codes used to identify procedures with biopsy or polypectomy
| CPT | 45380, 45384, 45385 |
| ICD-9-CM | 45.25, 45.41, 45.42, 48.24, 48.35, 48.36 |
Statistical analysis was performed using SAS (Version 9.2) and Microsoft Excel (Version 12.2.6).
Results
Screening Colonoscopy Procedures and Anesthesiologist Involvement
During our study period, there were 16,268 screening colonoscopies performed in our sample. Just over half of the patients were female and approximately 40% were 70–74 years of age (Table 1). The majority of patients in the sample were white (90.1%). Over half of the sample had no comorbid conditions (56.5%) and over 75% of the patients had their screening colonoscopy performed by a gastroenterologist. Approximately 4% of screening colonoscopies took place in an office, 39% took place in an ambulatory surgical center, and 57% took place in a hospital-based setting. The proportion of beneficiaries who had a screening colonoscopy increased annually, from 1.1% in 2001 to 2.6% in 2005 (Figure 1).
Table 1.
Sample characteristics
| Sample Characteristics | N | Percentage of Sample | |
|---|---|---|---|
| Age Group | 68–69 | 3128 | 19.2 |
| 70–74 | 6688 | 41.1 | |
| 75–79 | 4295 | 26.4 | |
| 80–84 | 1761 | 10.8 | |
| 85–94 | 396 | 2.4 | |
| Sex | Male | 7558 | 46.5 |
| Female | 8710 | 53.5 | |
| Race | White | 14657 | 90.1 |
| Black | 715 | 4.4 | |
| Other | 896 | 5.5 | |
| Comorbid conditions | 0 | 9195 | 56.5 |
| 1–2 | 5856 | 36.0 | |
| ≥3 | 1217 | 7.5 | |
| Income | < $34,795 | 3154 | 19.4 |
| $34,808–$42,344 | 3155 | 19.4 | |
| $42,393–$51,738 | 3157 | 19.4 | |
| $51,740–$65,514 | 3152 | 19.4 | |
| > $65,523 | 3152 | 19.4 | |
| Unknown | 498 | 3.1 | |
| Registry | San Francisco | 503 | 3.1 |
| Connecticut | 1518 | 9.3 | |
| Detroit | 1212 | 7.5 | |
| Hawaii | 298 | 1.8 | |
| Iowa | 1397 | 8.6 | |
| New Mexico | 465 | 2.9 | |
| Seattle | 1073 | 6.6 | |
| Utah | 724 | 4.5 | |
| Atlanta | 559 | 3.4 | |
| San Jose | 385 | 2.4 | |
| Arizona Indians | 147 | 0.9 | |
| Los Angeles | 833 | 5.1 | |
| Rural Georgia | 35 | 0.2 | |
| Greater California | 2804 | 17.2 | |
| Kentucky | 1254 | 7.7 | |
| Louisiana | 993 | 6.1 | |
| New Jersey | 1893 | 11.6 | |
| Other | 175 | 1.1 | |
| Operator Specialty | GI | 12313 | 75.7 |
| Surgery | 1493 | 9.2 | |
| Primary Care | 1813 | 11.1 | |
| Other/unknown | 649 | 4.0 |
Figure 1.
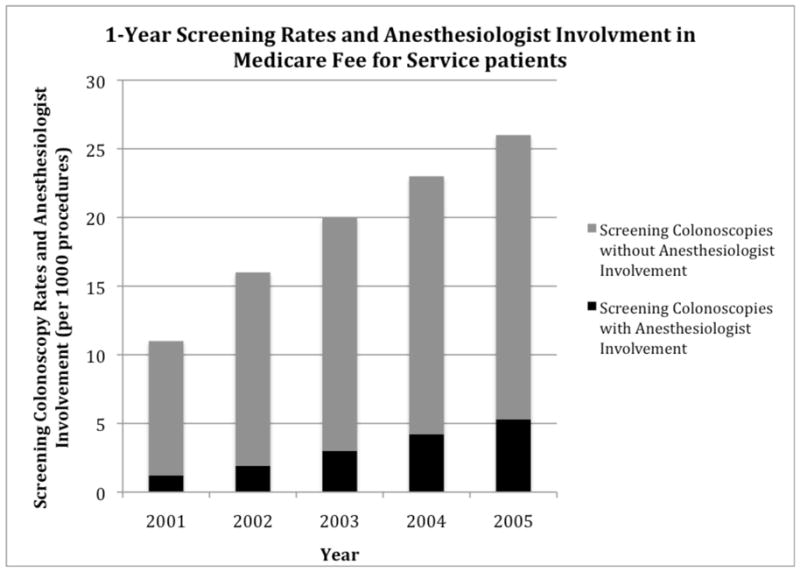
1-Year Screening Rates and Anesthesiologist Involvement in Medicare Fee for Service Patients
Overall, 17.2% of screening colonoscopies had claims that identified anesthesiologist involvement between 2001 and 2006. However, the frequency of anesthesiologist involvement increased each year, more than doubling from a low of 11.0% in 2001 to a high of 23.4% in 2006 (Figure 1).
Patient and Provider Characteristics
Anesthesiologist involvement was quite similar across age groups and sexes (Table 2). However, there was variation in the likelihood of anesthesiologist involvement based on race, comorbidity, and region. White patients had anesthesiologist involvement in 17.8% of screening colonoscopies compared to 21.7% in black patients. However, after adjusting for confounding factors, black patients were significantly less likely to have anesthesiologist involvement (adjusted OR: 0.76; 95% CI: 0.61–0.94). There was an upward trend in anesthesiologist involvement in those with higher comorbidity (Table 2). Anesthesiologist involvement by registry ranged from 1.6% in San Francisco to 57.8% in New Jersey (Figure 2).
Table 2.
Patient and Provider Characteristics in Screening Colonoscopy Procedures and Involvement of Anesthesiologist
| Unadjusted | Adjusted* | |||||
|---|---|---|---|---|---|---|
| Patient/Provider Characteristics | Percentage Involving Anesthesiologist | Odds ratio | 95% CI | Odds ratio | 95% CI | |
| Age Group | 68–69 | 18.3 | 1.00 | -- | ||
| 70–74 | 17.2 | 0.93 | 0.83–1.04 | |||
| 75–79 | 17.3 | 0.93 | 0.83–1.05 | |||
| 80–84 | 18.2 | 1.00 | 0.86–1.16 | |||
| 85+ | 17.2 | 0.93 | 0.70–1.22 | |||
| Sex | Male | 17.5 | 1.00 | -- | ||
| Female | 17.5 | 1.00 | 0.92–1.08 | |||
| Race | White | 17.8 | 1.00 | -- | 1.00 | -- |
| Black | 21.7 | 1.28 | 1.07–1.54 | 0.76 | 0.61–0.94 | |
| Other | 10.5 | 0.54 | 0.44–0.67 | 0.56 | 0.43–0.74 | |
| Comorbid conditions | 0 | 16.7 | 1.00 | -- | 1.00 | -- |
| 1–2 | 18.4 | 1.13 | 1.03–1.23 | 1.01 | 0.91–1.11 | |
| ≥3 | 20.0 | 1.25 | 1.07–1.45 | 1.15 | 0.96–1.37 | |
| Income | < $34,795 | 15.7 | 1.00 | -- | 1.00 | -- |
| $34,808–$42,344 | 12.7 | 0.78 | 0.68–0.90 | 0.68 | 0.57–0.79 | |
| $42,393–$51,738 | 14.7 | 0.93 | 0.81–1.06 | 0.66 | 0.56–0.78 | |
| $51,740–$65,514 | 20.2 | 1.36 | 1.19–1.55 | 0.73 | 0.62–0.86 | |
| > $65,523 | 25.0 | 1.79 | 1.58–2.03 | 0.69 | 0.58–0.81 | |
| Unknown | 14.1 | 0.88 | 0.67–1.15 | 0.51 | 0.37–0.70 | |
| Operator Specialty | GI | 18.0 | 1.00 | -- | 1.00 | -- |
| Surgery | 24.2 | 1.46 | 1.28–1.65 | 2.80 | 2.40–3.27 | |
| Primary Care | 11.3 | 0.58 | 0.50–0.68 | 0.82 | 0.69–0.97 | |
| Other/unknown | 11.7 | 0.61 | 0.48–0.77 | 0.78 | 0.59–1.03 | |
Also adjusted for year of procedure
Figure 2.
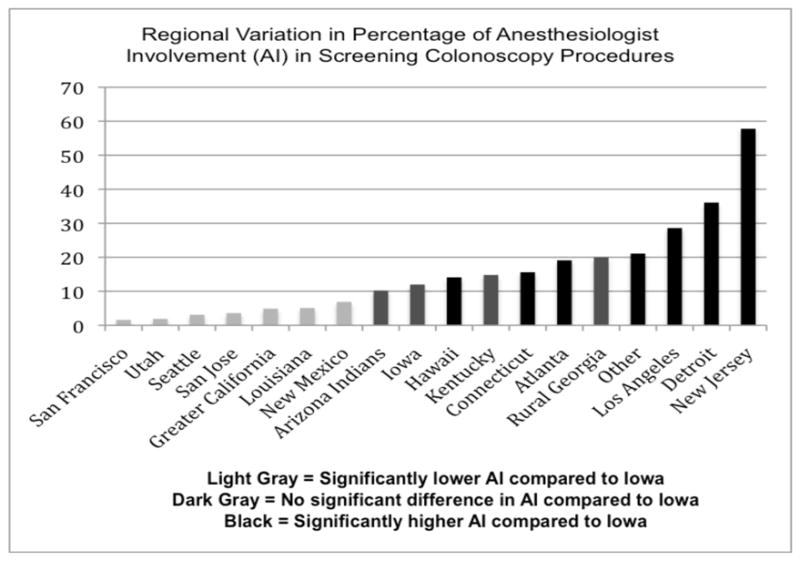
Regional Variation in Percentage of Anesthesiologist Involvement in Screening Colonoscopy Procedures
Upon examination of provider characteristics, we found that surgeons had anesthesiologist involvement in 24.2% of screening colonoscopies compared to 18.0% in gastroenterologists and 11.3% in primary care providers. Anesthesiologist involvement in screening colonoscopies was 24.8% in the office, 21% in an ambulatory surgical center, and 13.8% in the hospital-based setting. The unadjusted association between setting of service and anesthesiologist involvement was significant.
Cost Associated with Anesthesiologist Involvement
The cost of a screening colonoscopy with anesthesiologist involvement ranged from approximately $601 to $752 depending on whether an intervention such as a biopsy or polypectomy was performed. The mean allowed charge estimate was $103 per case for anesthesiologist involvement in a screening colonoscopy based on the cases in our sample that were done in 2005. The total number of procedures was derived to be 1,162,000 screening colonoscopies during the study period. We explored the costs associated with no anesthesiologist involvement, anesthesiologist involvement based on the 17.2% average of our sample, and 100% anesthesiologist involvement if all cases in our sample had anesthesiologist involvement (Table 3). The additional cost was approximately $20 million during the study period and would be approximately $120 million if all cases had anesthesiologist involvement.
Table 3.
Screening Colonoscopy Costs
| Average cost of procedure without anesthesiologist involvement (A) | Average cost of procedure with anesthesiologist involvement (B) | Total number of procedures in our sample | Total number of procedures in US Medicare (C) | National Medicare cost with no anesthesiologist involvement (D) | National Medicare cost with 17.2% anesthesiologist involvement (E) | National Medicare cost with 100% anesthesiologist involvement (F) | |
|---|---|---|---|---|---|---|---|
| Screening Colonoscopy | $575.20 | $678.20 | 16,268 | 1,162,000 | $668,382,400 | $688,968,392 | $788,068,400 |
8,365 of 16,268 screening colonoscopies involved biopsy or polypectomy at $648.52 while the remaining 7,903 had no intervention at $497.59 per procedure
Mean allowed charge estimate $103 per case for anesthesiologist involvement
16,268 (total number of procedures in our sample) multiplied by 20 (our cohort was derived from 5% sample of Medicare beneficiaries) divided by 0.28 (SEER data represents only 28% of US population)
1,162,000 (total number of procedures in US Medicare) × $575.20 (average cost of procedure without anesthesiologist involvement)
1,162,000 (total number of procedures in US Medicare) × $575.20 (average cost of procedure without anesthesiologist involvement) × 0.828 (percentage without anesthesiologist involvement) + 1,162,000 (total number of procedures in US Medicare) × $678.20 (average cost of procedure with anesthesiologist involvement) × 0.172 (percentage with anesthesiologist involvement)
1,162,000 (total number of procedures in US Medicare) × $678.20 (average cost of procedure with anesthesiologist involvement)
Discussion
Anesthesiologist involvement in screening colonoscopies among Medicare beneficiaries increased substantially from 2001 to 2006. This trend was compounded by the doubling of the screening colonoscopy rate. As a result, there has been a profound increase in the number of screening colonoscopies with anesthesiologist involvement at the population level. This represents a significant change in practice. At the same time, it has yet to be determined whether patient outcomes are actually improved by anesthesiologist involvement.
The involvement of anesthesiologists in screening colonoscopies has attracted substantial interest amongst gastroenterologists, anesthesiologists, and payers given the financial implications associated with anesthesiologist involvement. A more recent Medicare estimate from 2009 is that the national mean allowed charge for code 00810 is $120 per case (CMS), which raises the financial impact compared to the estimate of $103 per case used in our study.
This shift in care patterns raises the question of the degree to which screening colonoscopy’s cost is affected by anesthesiologist involvement. A cost-effectiveness analysis for CRC screening that was performed for the United States Preventive Services Task Force (USPSTF) estimated the cost of a colonoscopy without polypectomy to range from $285 to $69513 with an average of $490, which is very close to the approximately $498 value that we used based on the 2007 AHRQ analysis. This analysis also showed that incremental cost effectiveness ratios for screening colonoscopy every 10 years ranged from $10,997 to $12,271 per life-year saved.13 With our estimate of a rise in cost of approximately 20% with anesthesiologist involvement, a thorough assessment of the cost effectiveness of screening colonoscopy with the added cost of anesthesiologist involvement warrants further attention.
There was no significant difference found in anesthesiologist involvement across age groups in our study period. It is often speculated that older persons receive higher levels of anesthesiologist involvement. However, it is possible that this reflects a difference between patients under versus over 65 years and does not apply to increasing ages among patients over 65 years of age.
Variation exists across regions in terms of the percentage of screening colonoscopies that involve an anesthesiologist or CRNA. In fact, a patient undergoing a screening colonoscopy in San Francisco or New Jersey had 0.18 and 15.43 fold odds, respectively, of having anesthesiologist involvement compared to a patient in Iowa. One explanation for the variation in the amount of reimbursement to anesthesiologists across regions may be due to local payor policy.14 Patient income and cost associated with anesthesiologist involvement also carry financial implications and have an effect on practice patterns.
Our study does have limitations. SEER provides data for 17 registries; however, this remains a representative sample of approximately 28% of the United States population and does not include all areas that Medicare covers.10 It does not take into account the competition among gastroenterology practices in specific regions, specific volume of cases per session per practitioner, an in-depth look at cases being performed side by side with patients of other third-party payors, or non-screening colonoscopy cases. The claims data has limitations in its ability to determine settings in which a nurse anesthetist practices independently for anesthesia services without the presence of an anesthesiologist. Also, this study focuses on utilization data and does not take into account any data on the patient perspective on the sedation being administered by an anesthesiologist in comparison to endoscopist-directed administration. Prior studies have demonstrated that a significant barrier to CRC screening for patients is the fear of pain or complications associated with the procedure.15–16 It is unclear whether anesthesiologist involvement is associated with increased safety. One study reported a peri-procedural mortality rate of approximately 1 in 14,000,17 and it is unknown whether anesthesiologist involvement further decreases the mortality rate.
As a result of the high cost estimates associated with anesthesiologist involvement, there has been evaluation of endoscopist-directed administration of propofol, which has been shown to be safe.18 A recent position statement by the American Society for Gastrointestinal Endoscopy (ASGE) states that the use of anesthesiologist-administered propofol for healthy individuals undergoing elective endoscopy is very costly without demonstrated improvement in patient safety or procedural outcome.19 On the other hand, anesthetists continue to urge for the administration of propofol only by persons trained in the administration of general anesthesia who are not simultaneously involved in the surgical or diagnostic procedure.20
We found that nearly a quarter of screening colonoscopies being performed in the Medicare population have anesthesiologist involvement and that the involvement varies dramatically across regions. Future research is needed to assess the impact on patients and outcomes associated with anesthesiologist involvement. The patient perspective regarding comfort and willingness to undergo the procedure with anesthesiologist involvement warrants further evaluation. An investigation of the potential benefits, including polyp detection rate, and potential risks, including the complication rate, with and without anesthesiologist involvement may help to determine the most safe and cost-effective approach to screening colonoscopies.
Acknowledgments
Funding/Support
This work was supported by funding from the National Institutes of Health (grant number 5R21HS017624).
This study used the linked SEER-Medicare database. The interpretation and reporting of these data are the sole responsibility of the authors. The authors acknowledge the efforts of the Applied Research Program, NCI; the Office of Research, Development and Information, CMS; Information Management Services (IMS), Inc.; and the Surveillance, Epidemiology, and End Results (SEER) Program tumor registries in the creation of the SEER-Medicare database.
Footnotes
Disclosures: The authors have no conflict of interest disclosures.
Author Contributions: Vijay S. Khiani – Study concept and design; Analysis/Interpretation; Drafting/Revision
John Gancayco – Study concept and design; Revision
Pamela Soulos – Analysis/Interpretation; Revision
Cary P. Gross – Study concept and design; Analysis/Interpretation; Revision; Supervision
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Greenwood A. Experts recommend steps to increase colorectal cancer screening in primary care. National Cancer Institute Bulletin. 2010 Feb;7(3) [cited 2010 Nov 30] Available from URL: http://www.cancer.gov/ncicancerbulletin/020910/page5.
- 2.Nelson RS, Thorson AG. Colorectal cancer screening. Curr Oncol Rep. 2009;11(6):482–9. doi: 10.1007/s11912-009-0065-8. [DOI] [PubMed] [Google Scholar]
- 3.Sonnenberg A, Delco F, Inadomi JM. Cost-effectiveness of colonoscopy in screening for colorectal cancer. Ann Intern Med. 2000;133(8):573–84. doi: 10.7326/0003-4819-133-8-200010170-00007. [DOI] [PubMed] [Google Scholar]
- 4.Center for Disease Control and Prevention. Colorectal cancer screening guidelines. CDC; 2010. Aug, [cited 2010 Nov 30]; Available from URL: http://www.cdc.gov/cancer/colorectal/basic_info/screening/guidelines.htm. [Google Scholar]
- 5.Imaeda A, Bender D, Fraenkel L. What is most important to patients when deciding about colorectal screening? J Gen Intern Med. 2010;25(7):688–93. doi: 10.1007/s11606-010-1318-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hayee B, Dunn J, Loganayagam A, et al. Midazolam with meperidine or fentanyl for colonoscopy: results of a randomized trial. Gastrointest Endosc. 2009;69(3):681–7. doi: 10.1016/j.gie.2008.09.033. [DOI] [PubMed] [Google Scholar]
- 7.Cohen LB, Wecsler JS, Gaetano JN, et al. Endoscopic Sedation in the United States: Results from a Nationwide Survey. Am J Gastroenterol. 2006;101:967–974. doi: 10.1111/j.1572-0241.2006.00500.x. [DOI] [PubMed] [Google Scholar]
- 8.Alharbi O, Rabeneck L, Paszat L, et al. A Population-based Analysis of Outpatient Colonoscopy in Adults Assisted by an Anesthesiologist. Anesthesiology. 2009;111:734–40. doi: 10.1097/ALN.0b013e3181b786d4. [DOI] [PubMed] [Google Scholar]
- 9.Surveillance Epidemiology and End Results. Overview of the SEER Program. National Cancer Institute; 2010. Nov, [cited 2010 Nov 30]; Available from URL: http://seer.cancer.gov/about/overview.html. [Google Scholar]
- 10.Ko CW, Kreuter W, Baldwin LM. Effect of Medicare Coverage on Use of Invasive Colorectal Cancer Screening Tests. Arch Int Med. 2002;162:2581–2586. doi: 10.1001/archinte.162.22.2581. [DOI] [PubMed] [Google Scholar]
- 11.Elixhauser A, Steiner C, Harris DR, et al. Comorbidity Measures for Use with Administrative Data. Med Care. 1998;36(1):8–27. doi: 10.1097/00005650-199801000-00004. [DOI] [PubMed] [Google Scholar]
- 12.Zauber AG, Lansdorp-Vogelaar I, Wilschut J, et al. Cost-Effectiveness of DNA Stool Testing to Screen for Colorectal Cancer: Report to AHRQ and CMS from the Cancer Intervention and Surveillance Modeling Network (CISNET) for MISCAN and SimCRC Models. 2007 Available from: https://www.cms.hhs.gov/mcd/viewtechassess.asp?from2=viewtechassess.asp&id=212&. [PubMed]
- 13.Pignone M, Saha S, Hoerger T, et al. Cost-Effectiveness Analyses of Colorectal Cancer Screening: A Systematic Review for the U.S. Preventive Services Task Force. Ann Intern Med. 2002;137:96–104. doi: 10.7326/0003-4819-137-2-200207160-00007. [DOI] [PubMed] [Google Scholar]
- 14.Aisenberg JA, Brill JV, Ladabaum U, et al. Sedation for gastrointestinal endoscopy: New Practices, New Economics. Am J Gastroenterol. 2005;100:996–1000. doi: 10.1111/j.1572-0241.2005.50034.x. [DOI] [PubMed] [Google Scholar]
- 15.Green A, Peters-Lewis A, Percac-Lima S, et al. Barriers to Screening Colonoscopy for Low-income Latino and White Patients in an Urban Community Health Center. J Gen Intern Med. 2008;23(6):834–40. doi: 10.1007/s11606-008-0572-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Shan-Rong C, Su-Zhan Z, Hong-Hong Z, et al. Barriers to colorectal cancer screening: A case-control study. World Journal of Gastroenterology. 2009;15(20):2531–6. doi: 10.3748/wjg.15.2531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rabeneck L, Paszat L, Hilsden R, et al. Bleeding and Perforation After Outpatient Colonoscopy and Their Risk Factors in Usual Clinical Practice. Gastroenterology. 2008;135:1899–1906. doi: 10.1053/j.gastro.2008.08.058. [DOI] [PubMed] [Google Scholar]
- 18.Rex DK, Deenadayalu V, Eid E, et al. Endoscopist-Directed Administration of Propofol: A Worldwide Safety Experience. Gastroenterology. 2009;137(4):1229–37. doi: 10.1053/j.gastro.2009.06.042. [DOI] [PubMed] [Google Scholar]
- 19.Vargo J, Cohen L, Rex D, et al. Position statement: nonanesthesiologist administration of propofol for GI endoscopy. Gastrointest Endosc. 2009;70(6):1053–9. doi: 10.1016/j.gie.2009.07.020. [DOI] [PubMed] [Google Scholar]
- 20.Reimbursement issues. ASAP; 2006. Anesthetists for the safe administration of propofol. [cited 2010 Nov 30]; Available from URL: http://www.safepropofol.org/speakout.html. [Google Scholar]


