Abstract
Matrix metalloproteinases (MMPs) are zinc-dependent endopeptidases that degrade the extracellular matrix and other extracellular proteins. Upregulation of MMPs activity is known to be required for the inflammatory cell infiltration after spinal cord injury (SCI) and most likely contributes to early blood spinal barrier disruption and inflammation, thereby leading to the impairment of functional recovery. Here, we examined the effect of ethanol extract of Bupleurum falcatum (BF) on functional recovery by inhibiting MMP-2 and -9 activation and inflammation after SCI. Rats received a moderate, weight-drop contusion injury to spinal cord were administered orally with BF at a dose of 100 mg/kg for 14 d and functional recovery was measured by Basso-Beattie-Bresnahan locomotor open field behavioral rating test, inclined plane test and foot print analysis. To examine the neuroprotective effect of BF, TUNEL staining and counting were also performed. In addition, the expression and/or activation of MMP-2, MMP-9 and inflammatory mediators such as TNF-α, IL-1β, COX-2, and iNOS were examined by RT-PCR and gelatin zymography using spinal cord tissue from 1 d after injury. Our data showed that BF significantly inhibited the expression and activation of both MMP-2 and MMP-9 after SCI. The mRNA expressions of TNF-α, IL-1β, COX-2, and iNOS were also significantly attenuated by BF. Furthermore, BF reduced apoptotic cell death at 1 d after injury, thereby significantly reduced lesion volume and improved functional recovery. Taken together, these results suggest that BF can be used as a potential therapeutic agent for treating acute spinal injury.
Keywords: matrix metalloproteinase, spinal cord injury, blood brain barrier, zymography
INTRODUCTION
Spinal cord injury (SCI) is a leading cause of permanent disability, resulting in partial or complete loss of motor and sensory function below the lesion site (Wells et al., 2003). Inflammatory and immune responses are one of the major factors exacerbating the pathogenesis after SCI. It is known that blood-brain barrier (BBB) permeability and thereby blood infiltration is increased after SCI. Infiltrated cells such as macrophage and neurophil are also known to be involved in inflammation after SCI. Furthermore, proteinases and in particular, matrix metalloproteinases (MMPs), are likely mediators of early secondary vascular pathogenesis after SCI (Noble et al., 2002; Bareyre and Schwab, 2003).
MMPs are soluble and cell-surface bound zincdependent endopeptidases (Birkedal-Hansen et al., 1993) that degrade the extracellular matrix and other extracellular proteins (Sternlicht and Werb, 2001). MMPs also play important roles in remodeling of the extracellular matrix, tissue morphogenesis, and wound healing (Werb, 1997). However, excessive proteolytic activity of MMPs can be detrimental, leading to numerous pathologic conditions, including BBB disruption (Rosenberg et al., 1998) and inflammation (Mun-Bryce and Rosenberg, 1998). For example, MMPs are significantly upregulated after SCI in mice, rat and human (Noble et al., 2002; Wells et al., 2003; Buss et al., 2007). Furthermore, MMPs mainly expressed during the first weeks after injury are known to be involved in the destructive inflammation events of protein breakdown and phagocytosis by infiltrating neutrophils and macrophages and in enhanced permeability of the blood spinal cord barrier (Noble et al., 2002; Wells et al., 2003; Buss et al., 2007). In particular, the activities of MMP-2 and MMP-9, which degrade types IV and V collagen, and thus modify constituents of basal laminae (Werb, 1997) are known to be increased within 1 d after SCI (Noble et al., 2002; Choi et al., 2010). Moreover, it was clearly demonstrated that the pharmacological blockade of MMPs, limited to the first 3 d after injury, is neuroprotective and promotes long-term recovery of hindlimb function (Noble et al., 2002). However, this beneficial response is lost when treatment is extended beyond the acutely injured cord to include wound healing and tissue remodeling (Trivedi et al., 2005; Hsu et al., 2006). These data suggest that the attenuation of MMP activities in early stage after SCI may exert beneficial effect and improve functional recovery.
The roots of Bupleurum falcatum have been used in Oriental countries as a herbal medicine for treating hepatitis, nephritis, influenza, inflammation, and bacterial and viral infections (Kumazawa et al., 1990). The extract of Bupleurum falcatum (BF) contains various compounds including a series of triterpene saponins namely saikosaponins (Ebata et al., 1996). Previous reports showed that saikosaponins exhibit a variety of pharmacological activites including anti-inflammatory, immunomodulatory and anti-bacterial activites in vitro and in vivo (Yamaguchi et al., 1985; Kumazawa et al., 1990). Furthermore, saikosaponins have been shown to modulate the gene expression or activation of MMP-2 in endothelial cells and spleen cells from picryl chloride-induced ear contact sensitivity mice (Shyu et al., 2004; Zhang et al., 2006). These observations suggest that BF may exert anti-inflammatory effect by inhibiting MMPs activity.
In this study, we showed that the systemic administration of BF significantly improves functional recovery after SCI in part by inhibiting the expression and/or activation of MMP-2, MMP-9 and inflammatory mediators, thereby inhibiting apoptotic cell death and reducing lesion volume.
MATERIALS AND METHODS
Spinal cord injury
Adult male Sprague Dawley [Sam:TacN (SD) BR; Samtako, Osan, Korea] rats were subjected to moderate contusion injury (10 g×25 mm) as described previously (Yune et al., 2007). For the sham-operated controls, the animals underwent a T10 laminectomy without weight-drop injury. Surgical interventions and postoperative animal care were performed in accordance with the Guidelines and Policies for Rodent Survival Surgery provided by the Animal Care Committee of the Kyung Hee University.
Preparation of BF
The dried roots of Bupleurum falcatum were extracted with 70% ethanol as described previously (Kim et al., 2001). The ethanol filtrate was evaporated in vacuo, and powdered BF was stored at -20℃ until use. By HPLC analysis, BF contains saikosaponin A, B1, B2, B3, B4, C, D, G, H and I.
BF administration
Powdered BF were suspended in sterile deionized water and administrated orally at a dose of (100 mg/kg) beginning at 2 h after SCI and then once a day for 14 d.
RNA isolation and RT-PCR
RNA isolation using TRIZOL Reagent (Invitrogen, Carlsbad, CA) and cDNA synthesis were performed as described previously (Lee et al., 2010). The primers used for MMP-2, MMP-9, iNOS, COX-2, TNF-α, IL-1β and GAPDH were synthesized by the Genotech Corp (Daejeon, Korea). Details of primers used for PCR in this study are shown in Table 1. GAPDH was used as an internal control. Experiments were repeated three times and the values obtained for the relative intensity were subjected to statistical analysis. The gels shown in figures are representatives of results from three separate experiments.
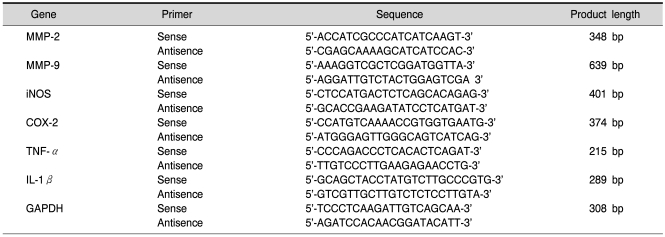
Table 1.
Primers used in the present study
Gelatin zymography
Total protein extracts from spinal cord samples at 1 d after injury were prepared as described previously (Yune et al., 2007). Spinal cord tissues (1 cm) were homogenized in a lysis buffer and the tissue homogenates were incubated for 20 min at 4℃, and centrifuged at 25,000×g for 30 min at 4℃. The protein level of the supernatant was determined using the BCA assay (Pierce, Rockford, IL). Gelatin zymography was performed by using 10% zymogram gel (Invitrogen) as previously described (Choi et al., 2010). In brief, 50µg proteins were mixed with sample buffer and loaded without boiling. After electrophoresis, the gel were soaked in 2.5% Triton X-100, rinsed, and incubated for 24 h at 37℃ in developing buffer (50 mM Tris-HCl, pH 8.5, 0.2 M NaCl, 5 mM CaCl2, 0.02% Brii35). After incubation, gels were stained with 0.5% Coomassie blue and then destained. Clear bands on the zymogram were indicative of gelatinase activity.
Behavioral tests
Examination of functional deficits after injury was conducted by using the 21-point Basso-Beattie-Bresnahan (BBB) locomotion scale, inclined plane test and foot print analysis as previously described (Yune et al., 2007).
Tissue preparation
After SCI, spinal cord sections were prepared as described previously (Yune et al., 2007). In brief, animals were perfused via cardiac puncture with 4% paraformaldehyde. A 20-mm section of the spinal cord, centered at the lesion site, was dissected out, post-fixed and placed in 30% sucrose. The segment was embedded in OCT for frozen sections, and longitudinal or transverse sections were then cut at 10 or 20µm on a cryostat (CM1850; Leica, Germany).
Terminal deoxynucleotidyl transferase-mediated deoxyuridine triphosphate-biotin nick end labeling (TUNEL)
One day after injury, serial spinal cord sections (20µm thickness) were collected and every 100 µm section was processed for TUNEL as previously described (Yune et al., 2007). Only those cells showing morphological features of nuclear condensation and/or compartmentalization only in the gray matter (GM) were counted as a TUNEL-positive. Quantitation of TUNEL-positive cells was accomplished by counting the number of cells labeled positively as described previously (Yune et al., 2009).
Assessment of lesion volume
Lesion volume, using rats employed for behavioral analyses, was assessed as described previously (Yune et al., 2008). In brief, serial longitudinal sections (10µm) through the dorsoventral axis of the spinal cord were used to determine lesion volume. Every 50µm, sections were stained with Cresyl violet acetate and studied with light microscopy. Areas at each longitudinal level were determined, and the total lesion volume derived by means of numerical integration of sequential areas.
Statistical analysis
Data presented as the mean±SD values. Comparisons between vehicle and BF treated groups were made by unpaired Student's t test. Behavioral scores from BBB analysis and inclined plane tests were analyzed by repeated measures ANOVA (time vs treatment). Tukey's multiple comparison was used as Post hoc analysis. Statistical significance was accepted with p<0.05. All statistical analyses were performed by using SPSS 15.0 (SPSS Science, Chicago, IL).
RESULTS
BF inhibits MMP-2 and MMP-9 expression and activation after SCI
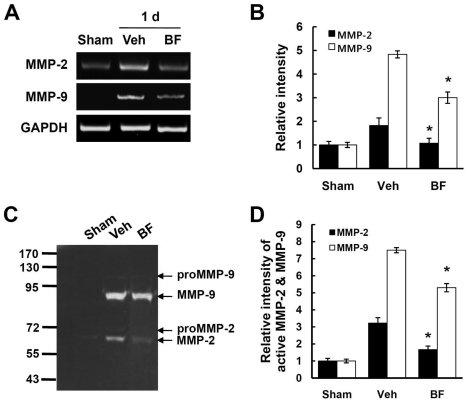
It has been known that saikosaponins modulates the gene expression or activation of MMP-2 in endothelial cells and spleen cells from picryl chloride-induced ear contact sensitivity mice (Shyu et al., 2004; Zhang et al., 2006). To test the hypothesis whether BF may inhibit MMP-2 and MMP-9 activation after SCI, we first examined the effect of BF on the expression of MMP-2 and MMP-9 by RT-PCR at 1 d after injury. A basal level of MMP-2 expression was detected in sham control. A significant upregulation of MMP-2 expression was observed at 1 d after SCI and BF treatment significantly reduced the MMP-2 mRNA expression (Fig. 1A, B). Similarly, MMP-9 mRNA was markedly increased at 1 d after SCI and BF treatment also significantly attenuated the MMP-9 mRNA expression (Fig. 1A, B). However, MMP-9 expression was not observed in the sham control. Next, we examined the enzyme activities of MMP-2 and MMP-9 by gelatin zymography using spinal cord total extract from 1 d after injury. As shown in Figure 1C, active form of MMP-2 and MMP-9 was strongly induced at 1 d after injury. Pro-MMP-2 and pro-MMP-9 were also induced by SCI. Furthermore, BF treatment significantly reduced the degree of activation of MMP-2 and MMP-9 when compared to vehicle-treated control (e.g., active MMP-2; BF 1.66±0.08 vs vehicle 3.22±0.22, p<0.05/active MMP-9; BF 5.3±0.11 vs vehicle 7.5±0.25, p<0.05) (Fig. 1B, D).
Fig. 1.
BF inhibits the expression and activation of MMP-2 and -9 after SCI. Total RNA and protein extracts from spinal cord samples at 1 d after injury were prepared as described in the Methods section. (A) RT-PCR of MMP-2 and MMP-9 and (B) quantitative analysis (intensity relative to sham value) of RT-PCR (n=3/group). *p<0.05. (C) Gelatine zymography of MMP-2 and MMP-9. (D) Quantitative analysis (intensity relative to sham value) of zymography (n=3/group). Data are presented as means±SD from three separate experiments. *p<0.05.
BF inhibits the expression of inflammatory mediators after SCI
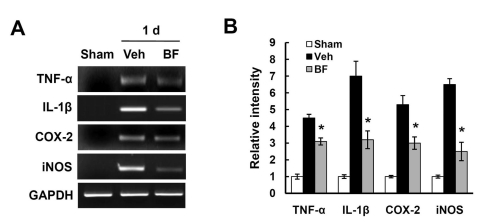
It has been known that BBB disruption by MMPs including MMP-2 and MMP-9 induces blood infiltration and thereby contributes to inflammation after SCI. Since BF reduced the expression and activity of MMP-2 and MMP-9 after SCI (Fig. 1), we hypothesized that BF would inhibit the expression of inflammatory factors after SCI. As shown in Fig. 2A, TNF-α, IL-1β, COX-2 and iNOS mRNA expression were markedly increased after SCI as reported (Lee et al., 2004; Yune et al., 2009). In particular, BF treatment significantly alleviated the expression levels of pro-inflammatory cytokines and mediators when compared with those of vehicletreated control at 1 d after injury (Fig. 2).
Fig. 2.
BF inhibits the expression of inflammatory factors after SCI. (A) Total RNA isolation from spinal cord samples at 1 d after injury were processed as described in the Method section (n=3/group). (A) RT-PCR for TNF-α, IL-1β, COX-2 and iNOS at 1 d after SCI. (B) Quantitative analysis shows that the expression of proinflammatory factors was significantly reduced by BF treatment. Data represent mean±SD from three separate experiments. *p<0.05.
BF inhibits apoptotic cell death after SCI
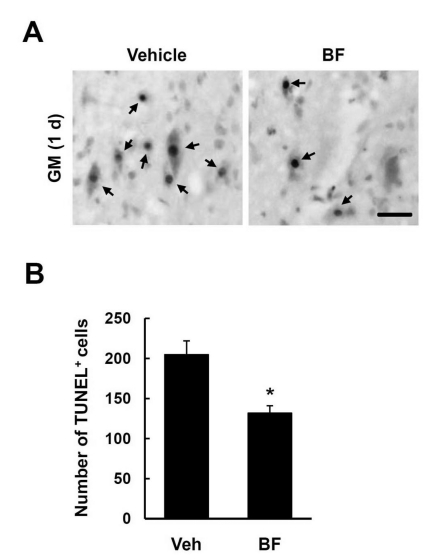
Trauma to the spinal cord results in extensive apoptotic cell death (Liu et al., 1997; Lee et al., 2003). Based on the anti-inflammatory effects of BF in the injured spinal cord (Fig. 2), we hypothesized that BF would inhibit apoptotic cell death after SCI. Many TUNEL-positive cells were seen mostly within the lesion area in the gray matter (GM) at 1 d after injury. As shown in Fig. 3, BF treatment significantly decreased the number of TUNEL-positive cells when compared to the vehicle-treated control (BF 132±9 vs. Vehicle 205±17 cells, p<0.05) (Fig. 3B). Thus, our results indicate that BF inhibits apoptotic cell death after injury.
Fig. 3.
The effect of BF on apoptotic cell death after SCI. Spinal cord tissues from 1 d after injury were processed for TUNEL staining as described in the Method section (n=5/group). (A) TUNEL-positive cells in the GM at 1 d after injury. Representative images were from the sections selected 1 mm rostral to the lesion epicenter. Bar, 50µm. (B) Quantitative analysis of TUNEL-positive cells in the GM at 1 d after injury. Serial transverse sections (10µm thickness) were collected every 100 µm from 2 mm rostral to 2 mm caudal to the lesion epicenter (total 40 sections for neurons). Data represent mean±SD obtained from five separate experiments. *p<0.05.
BF improves functional recovery after SCI
Previous report showed that pharmacological inhibition of MMPs at a early stage after SCI improves locomotor recovery (Noble et al., 2002). Since BF treatment inhibited the expression and activity of MMP-2 and MMP-9 and also attenuated apoptotic cell death after injury (Fig. 1 and 3), we expected that BF would improve functional recovery following injury. Injured rats were treated with BF (100 mg/kg) for 14 consecutive days and functional recovery was then evaluated for 35 d using the BBB rating scale, inclined plane test and footprint analysis. The hindlimbs paralyzed immediately after injury were spontaneously recovered within 7 to 14 d after injury (Fig. 4A) as in previous report (Yune et al., 2007). The BBB scores were significantly higher in rats treated with 100 mg/kg of BF by 14 to 35 d after SCI than in vehicle-treated rats (35 d, BF 11.25±0.5 vs Vehicle 9.0±1.0, p<0.05) (Fig. 4A). The angle of incline, determined 1~4 weeks after injury, was also significantly higher in BFtreated rats than in vehicle-treated rats at 4 weeks after SCI (4 weeks, BF 60±2.1 vs Vehicle 53±2.2, p<0.05) (Fig. 4B). Finally, footprint analyses obtained from sham-treated, vehicle-treated and BFtreated rats at 35 d after SCI revealed that BFtreated rats show more consistent forelimb-hindlimb coordination and less toe drag than in vehicle control (Fig. 4C). With the 25 mm insult used in the present study, the hind paws as well as the central pads of vehicle-treated animals were not clearly recorded because of the hindlimb drags (Fig. 4C). Thus, we didn't quantify footprint analysis using toe spread and ipsilateral distances (limb coordination) in this study.
Fig. 4.
BF improves functional recovery and reduces lesion volume after SCI. After SCI, BF was administered orally at a dose of 100 mg/kg beginning at 2 h after SCI and then once a day for 14 d. Functional recovery was assessed by BBB, inclined plane test and footprint analysis (n=10/group). (A) BBB scores. (B) Inclined plane test. Note that BF treatment significantly increased BBB score and angle of incline after SCI. Data represent mean±SD. *p<0.05. (C) Representative footprints obtained from each group at 35 d after SCI. (D) Quantitative analysis of lesion volumes at 38 d after injury (n=5/group). Data are presented as means±SD from five separate experiments. *p<0.05.
BF reduces lesion volume after SCI
The functional deficit after SCI is known to be correlated with the massive tissue loss (Basso et al., 1996). To examine whether BF preserves spinal cord tissue after injury, we measured the lesion volume using rats tested for behavioral analysis. As shown in Fig. 4D, BF treatment significantly reduced the lesion volume at 38 d after injury than in vehicle-treated rats (BF 4.2±1.2 mm3 vs Vehicle 8.5±0.7 mm3, p<0.05).
DISCUSSION
In this study, we demonstrated the first time that after moderate contusion injury to the rat spinal cord, BF treatment improved functional recovery by inhibiting the expression and/or activation MMP-2, MMP-9 and inflammatory mediators, thereby attenuating apoptotic cell death.
A critical finding in this study is that BF can effectively inhibit MMP upregulation, thereby improve locomotor function after SCI. The functional impairment after SCI may be attributed to the early involvement of MMPs in secondary pathogenesis after injury. It has been known that in brain and injured spinal cord, MMPs including MMP-2 and MMP-9, contribute to early secondary pathogenesis by disrupting the BBB and promoting inflammation (Rosenberg et al., 1998; Noble et al., 2002), oxidative stress (Gasche et al., 2001) and demyelination (Asahi et al., 2001). It was also known that animals treated with an MMP inhibitor within the first 3 d after injury showed less disruption of the BBB, attenuation of neutrophil infiltration, and significant locomotor recovery compared with vehicletreated control (Noble et al., 2002). Our data indicate that BF treatment significantly inhibited the expression and activity of MMP-2 and MMP-9 after SCI (Fig. 1). Also, the expression of inflammatory mediators such as TNF-α, IL-1β, COX-2 and iNOS was significantly decreased following BF treatment (Fig. 2). In addition, the number of TUNELpositive cells in the GM at 1 d and the lesion volume at 35 d after injury was significantly inhibited by BF treatment (Fig. 3, 4). Thus, these results suggest that the effect of neuroprotection followed functional recovery by BF are likely mediated in part by inhibiting MMP-2 and MMP-9, then attenuating the increase of BBB permeability and blood infiltration after SCI. However, we did not examine whether BF inhibits BBB disruption and blood infiltration after injury in this study. Further study may be required to elucidate the effects of BF on BBB permeability and blood infiltration after SCI.
It has also been known that the beneficial effect of MMP inhibition is lost by long term blockade of MMPs for the first week after SCI (Trivedi et al., 2005). Hsu et al. (2006) also demonstrated that MMP-2 increased between 7 and 14 d after injury, was involved in wound healing and tissue remodeling after SCI. In this study, we observed the inhibition of MMP-2 by BF at 1 d after injury. In addition, it was reported that the general MMPs blocker, GM6001 treatment for first 3 d after SCI improved functional recovery (Noble et al., 2002). Furthermore, when we examine the effect of BF on MMP-2 at 7 and 14 d after injury, neither gene expression nor gelatinase activity of MMP-2 was changed (data not shown). Therefore we believe that the inhibition of MMP-2 and MMP-9 activity by BF at 1 d after injury may contribute to beneficial to functional recovery. MMP-12 is also known to be upregulated at 5 d and involved in the dysfunction in BBB permeability and inflammation after SCI (Wells et al., 2003). Furthermore, Wells et al. (2003) showed that functional recovery was significantly improved in MMP-12 null mice compared with wild-type controls. Therefore, further study may be needed to examine the effect of BF on MMP-12 after SCI.
We examined the neuroprotective effect of BF after SCI using total ethanol extract in the present study. During the experiment, neither significant side effects nor an increase in mortality by BF treatment were observed (data not shown). As a previous report showed that aikosaponins, the major components in the roots of Bupleurum falcatum, exhibit anti-inflammatory, immunomodulatory activites in vitro and in vivo (Yamaguchi et al., 1985; Kang et al., 2008), further study to find active components exhibiting MMP inhibition and examine their neuroprotection after SCI will be processed.
In summary, our results indicate that the inhibition of MMP-2 and MMP-9 by BF may account for in part its neuroprotective effect and provide an evidence for BF as a potential therapeutic agent after SCI.
ACKNOWLEDGEMENTS
This research was supported by the Kyung Hee University Research Fund in 2006 (KHU-20061247).
References
- 1.Asahi M, Wang X, Mori T, Sumii T, Jung JC, Moskowitz MA, Fini ME, Lo EH. Effects of matrix metalloproteinase-9 gene knock-out on the proteolysis of bloodbrain barrier and white matter components after cerebral ischemia. J Neurosci. 2001;21:7724–7732. doi: 10.1523/JNEUROSCI.21-19-07724.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bareyre FM, Schwab ME. Inflammation, degeneration and regeneration in the injured spinal cord: insights from DNA microarrays. Trends Neurosci. 2003;26:555–563. doi: 10.1016/j.tins.2003.08.004. [DOI] [PubMed] [Google Scholar]
- 3.Basso DM, Beattie MS, Bresnahan JC, Anderson DK, Faden AI, Gruner JA, Holford TR, Hsu CY, Noble LJ, Nockels R, Perot PL, Salzman SK, Young W. MASCIS evaluation of open field locomotor scores: effects of experience and teamwork on reliability. Multicenter Animal Spinal Cord Injury Study. J Neurotrauma. 1996;13:343–359. doi: 10.1089/neu.1996.13.343. [DOI] [PubMed] [Google Scholar]
- 4.Birkedal-Hansen H, Moore WG, Bodden MK, Windsor LJ, Birkedal-Hansen B, DeCarlo A, Engler JA. Matrix metalloproteinases: a review. Crit Rev Oral Biol Med. 1993;4:197–250. doi: 10.1177/10454411930040020401. [DOI] [PubMed] [Google Scholar]
- 5.Buss A, Pech K, Kakulas BA, Martin D, Schoenen J, Noth J, Brook GA. Matrix metalloproteinases and their inhibitors in human traumatic spinal cord injury. BMC Neurol. 2007;7:17. doi: 10.1186/1471-2377-7-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Choi DC, Lee JY, Moon YJ, Kim SW, Oh TH, Yune TY. Acupuncture-mediated inhibition of inflammation facilitates significant functional recovery after spinal cord injury. Neurobiol Dis. 2010;39:272–282. doi: 10.1016/j.nbd.2010.04.003. [DOI] [PubMed] [Google Scholar]
- 7.Ebata N, Nakajima K, Hayashi K, Okada M, Maruno M. Saponins from the root of Bupleurum falcatum. Phytochemistry. 1996;41:895–901. doi: 10.1016/0031-9422(95)00720-2. [DOI] [PubMed] [Google Scholar]
- 8.Gasche Y, Copin JC, Sugawara T, Fujimura M, Chan PH. Matrix metalloproteinase inhibition prevents oxidative stress-associated blood-brain barrier disruption after transient focal cerebral ischemia. J Cereb Blood Flow Metab. 2001;21:1393–1400. doi: 10.1097/00004647-200112000-00003. [DOI] [PubMed] [Google Scholar]
- 9.Hsu JY, McKeon R, Goussev S, Werb Z, Lee JU, Trivedi A, Noble-Haeusslein LJ. Matrix metalloproteinase-2 facilitates wound healing events that promote functional recovery after spinal cord injury. J Neurosci. 2006;26:9841–9850. doi: 10.1523/JNEUROSCI.1993-06.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kang OH, Chae HS, Oh YC, Choi JG, Lee YS, Jang HJ, Kim JH, Kim YC, Sohn DH, Park H, Kwon DY. Anti-nociceptive and anti-inflammatory effects of Angelicae dahuricae radix through inhibition of the expression of inducible nitric oxide synthase and NO production. Am J Chin Med. 2008;36:913–928. doi: 10.1142/S0192415X0800634X. [DOI] [PubMed] [Google Scholar]
- 11.Kim YO, Leem K, Park J, Lee P, Ahn DK, Lee BC, Park HK, Suk K, Kim SY, Kim H. Cytoprotective effect of Scutellaria baicalensis in CA1 hippocampal neurons of rats after global cerebral ischemia. J Ethnopharmacol. 2001;77:183–188. doi: 10.1016/s0378-8741(01)00283-5. [DOI] [PubMed] [Google Scholar]
- 12.Kumazawa Y, Kawakita T, Takimoto H, Nomoto K. Protective effect of saikosaponin A, saikosaponin D and saikogenin D against Pseudomonas aeruginosa infection in mice. Int J Immunopharmacol. 1990;12:531–537. doi: 10.1016/0192-0561(90)90117-6. [DOI] [PubMed] [Google Scholar]
- 13.Lee JY, Chung H, Yoo YS, Oh YJ, Oh TH, Park S, Yune TY. Inhibition of apoptotic cell death by ghrelin improves functional recovery after spinal cord injury. Endocrinology. 2010;151:3815–3826. doi: 10.1210/en.2009-1416. [DOI] [PubMed] [Google Scholar]
- 14.Lee SM, Yune TY, Kim SJ, Kim YC, Oh YJ, Markelonis GJ, Oh TH. Minocycline inhibits apoptotic cell death via attenuation of TNF-alpha expression following iNOS/NO induction by lipopolysaccharide in neuron/glia co-cultures. J Neurochem. 2004;91:568–578. doi: 10.1111/j.1471-4159.2004.02780.x. [DOI] [PubMed] [Google Scholar]
- 15.Lee SM, Yune TY, Kim SJ, Park DW, Lee YK, Kim YC, Oh YJ, Markelonis GJ, Oh TH. Minocycline reduces cell death and improves functional recovery after traumatic spinal cord injury in the rat. J Neurotrauma. 2003;20:1017–1027. doi: 10.1089/089771503770195867. [DOI] [PubMed] [Google Scholar]
- 16.Liu XZ, Xu XM, Hu R, Du C, Zhang SX, McDonald JW, Dong HX, Wu YJ, Fan GS, Jacquin MF, Hsu CY, Choi DW. Neuronal and glial apoptosis after traumatic spinal cord injury. J Neurosci. 1997;17:5395–5406. doi: 10.1523/JNEUROSCI.17-14-05395.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mun-Bryce S, Rosenberg GA. Gelatinase B modulates selective opening of the blood-brain barrier during inflammation. Am J Physiol. 1998;274:R1203–R1211. doi: 10.1152/ajpregu.1998.274.5.R1203. [DOI] [PubMed] [Google Scholar]
- 18.Noble LJ, Donovan F, Igarashi T, Goussev S, Werb Z. Matrix metalloproteinases limit functional recovery after spinal cord injury by modulation of early vascular events. J Neurosci. 2002;22:7526–7535. doi: 10.1523/JNEUROSCI.22-17-07526.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rosenberg GA, Estrada EY, Dencoff JE. Matrix metalloproteinases and TIMPs are associated with bloodbrain barrier opening after reperfusion in rat brain. Stroke. 1998;29:2189–2195. doi: 10.1161/01.str.29.10.2189. [DOI] [PubMed] [Google Scholar]
- 20.Shyu KG, Tsai SC, Wang BW, Liu YC, Lee CC. Saikosaponin C induces endothelial cells growth, migration and capillary tube formation. Life Sci. 2004;76:813–826. doi: 10.1016/j.lfs.2004.10.003. [DOI] [PubMed] [Google Scholar]
- 21.Sternlicht MD, Werb Z. How matrix metalloproteinases regulate cell behavior. Annu Rev Cell Dev Biol. 2001;17:463–516. doi: 10.1146/annurev.cellbio.17.1.463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Trivedi AK, Hsu JY, Lin Y, Goussev S, Gan J, Topp KS, Noble-Haeusslein LJ. The effects of acute and extended inhibition of matrix metalloproteinases on demyelination and functional recovery after spinal cord injury. Int J Neuroprotect Neuroregen. 2005;2:30–38. [Google Scholar]
- 23.Wells JE, Rice TK, Nuttall RK, Edwards DR, Zekki H, Rivest S, Yong VW. An adverse role for matrix metalloproteinase 12 after spinal cord injury in mice. J Neurosci. 2003;23:10107–10115. doi: 10.1523/JNEUROSCI.23-31-10107.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Werb Z. ECM and cell surface proteolysis: regulating cellular ecology. Cell. 1997;91:439–442. doi: 10.1016/s0092-8674(00)80429-8. [DOI] [PubMed] [Google Scholar]
- 25.Yamaguchi N, Kohno H, Tawara M, Odashima S, Abe H. Effect of saikosaponin derivatives upon the immune response against T-dependent and T-independent antigens in mice. Int J Immunopharmacol. 1985;7:827–832. doi: 10.1016/0192-0561(85)90044-x. [DOI] [PubMed] [Google Scholar]
- 26.Yune TY, Lee JY, Cui CM, Kim HC, Oh TH. Neuroprotective effect of Scutellaria baicalensis on spinal cord injury in rats. J Neurochem. 2009;110:1276–1287. doi: 10.1111/j.1471-4159.2009.06214.x. [DOI] [PubMed] [Google Scholar]
- 27.Yune TY, Lee JY, Jiang MH, Kim DW, Choi SY, Oh TH. Systemic administration of PEP-1-SOD1 fusion protein improves functional recovery by inhibition of neuronal cell death after spinal cord injury. Free Radic Biol Med. 2008;45:1190–1200. doi: 10.1016/j.freeradbiomed.2008.07.016. [DOI] [PubMed] [Google Scholar]
- 28.Yune TY, Lee JY, Jung GY, Kim SJ, Jiang MH, Kim YC, Oh YJ, Markelonis GJ, Oh TH. Minocycline alleviates death of oligodendrocytes by inhibiting pro-nerve growth factor production in microglia after spinal cord injury. J Neurosci. 2007;27:7751–7761. doi: 10.1523/JNEUROSCI.1661-07.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Zhang L, Dong Y, Sun Y, Chen T, Xu Q. Role of four major components in the effect of Si-Ni-San, a traditional Chinese prescription, against contact sensitivity in mice. J Pharm Pharmacol. 2006;58:1257–1264. doi: 10.1211/jpp.58.9.0013. [DOI] [PubMed] [Google Scholar]