Abstract
Purpose
Since we reported about a landmark technique to reopen an occluded subclavian artery, we have faced difficulty in using protection devices in the vertebral artery to protect against thromboembolism from the reversed steal phenomenon after angioplasty and stenting. Therefore, we are presenting an optimal solution in using a protection device while recanalizing the occluded subclavian artery.
Materials and Methods
Among 21 cases of stenting for subclavian artery steno-occlusion, we applied the landmark technique at the opposite end of an occluded segment in 4 patients and used a protection device in two patients. Because the embolic protection device was placed in the vertebral artery via the brachial artery, optimal angioplasty and stenting via the brachial route were limited. Therefore, angioplasty via the trans-brachial approach was needed to be followed by stenting through a trans-femoral approach. We estimated the safe and optimal steps for placement and retrieval of the protection devices in addition to stenting.
Results
The procedure was safely performed when a stent was introduced via the femoral artery and a protection device was used via the brachial artery. However, in cases when a guidewire wasn't passed via the transfemoral route, simultaneous use of two systems via the brachial route could cause friction of devices or trapping of protection devices in a stent. When a protection device was trapped in a deployed stent, we retrieved the protection device with a 4F angiocatheter by selectively rotating the catheter tip. To avoid such procedural difficulty, we recommend using a transbrachial angioplasty followed by trans-femoral stenting while placing the protection device in the vertebral artery via the trans-brachial route.
Conclusion
If a guidewire is not passed through using a trans-femoral approach while performing the landmark technique, changing the stenting route from brachial to the femoral artery can be useful after securing the lumen in the occluded subclavian artery after angioplasty via the brachial artery.
Keywords: Subclavian artery, Stents, Endovascular techniques, Embolic Protection, Devices
Subclavian artery (SCA) steno-occlusion is still one of the most common sites prone to atherosclerosis despite its different involvement pattern of atherosclerotic stenosis in Koreans [1-6]. Although surgical treatment for a SCA occlusion has been widely used, percutaneous endovascular technique is another option and may prove efficacious for a broader spectrum of patients, since they allow a direct correction of the hemodynamic insufficiency [7, 8].
Through our previous report, we suggested a more efficacious and safer method of recanalization using a Landmark-wire technique [9]. However, unlike carotid stenting with a protection device, little is known about distal protection methods during stenting procedures [8, 10-12]. Therefore, we will present a safe and effective technique using a protective device in stenting of a symptomatic subclavian artery occlusion and describe how to apply sequential procedural steps of angioplasty followed by stenting while using a protection device with the Landmark-wire technique.
MATERIALS AND METHODS
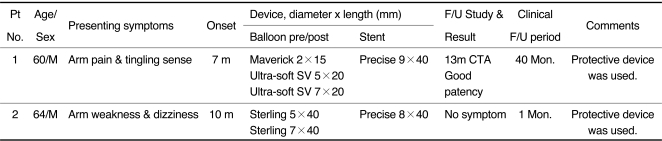
Among 21 consecutive patients who underwent SCA and brachiocephalic artery stent insertion at our institute, there were four patients (three men, one woman; age range, 53-64 years) with symptomatic SCA occlusion from May 2006 to June 2011. Of these patients, we performed the subclavian artery stenting under the vertebral artery protection in two patients (Table 1). Their symptoms were dizziness, arm weakness, coolness and absent or weak pulse and/or blood pressure difference (> 20 mmHg) in both arms.
Table 1.
Summary of Patients
Abbreviation: CTA, CT angiography; DUS, Doppler ultrasound; VA, vertebral artery; F/U, follow-up
Note.-Ultra-soft SV (BostonScientific Scimed Inc. MN, U.S.A.), Maverick (Boston Scientific Corp., Natick, MA, U.S.A.), Precise (Cordis Corp, Miami, FL, U.S.A.). All the lesions were in the left subclavian artery.
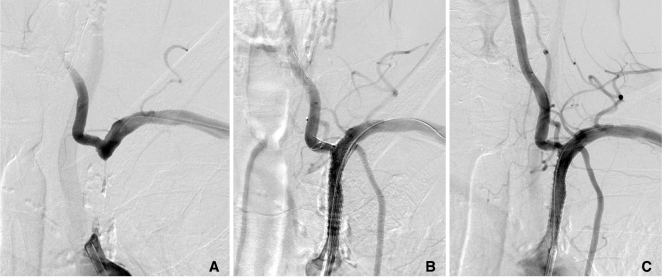
Angiogram revealed both the steal phenomenon and prevertebral segment occlusion in one patient, and occlusion of the left subclavian artery from aortic origin to just before the left vertebral artery origin in another patient (Fig. 1).
Fig. 1.
A 64-year-old male patient presented with dizziness and left arm weakness. He had history of laryngeal cancer which was operated and radiated 12 years ago.
A. Angiogram obtained through both catheters introduced via the trans-femoral and trans-brachial routes reveals the occluded left subclavian artery.
B. The protective device is trapped in the stent strut while deploying the stent via the same trans-brachial route and is retrieved by 4 F Davis angiocatheter.
C. The final angiogram reveals good patency of the recanalized SCA. Note good antegrade flow in the vertebral artery and mild spasm at the vertebral artery ostium.
All patients were given dual antiplatelet medication (100 mg aspirin and 75 mg clopidogrel) at least three days before the procedure [6, 8, 13, 14]. The procedure was performed under local neuroleptic anesthesia. Technical success was defined as angiographic residual stenosis less than 20% and a gradient of less than 5 mmHg across the treated lesion. Patients were evaluated 1-13 months following the procedure. Patency of the stented segment was demonstrated by means of CT angiography (CTA) after one year. Clinical failure was defined as renewed clinical symptoms caused by recurrent obstruction of the SCA.
Protection Device in Landmark-wire Technique
After careful evaluation of the color-coded duplex sonography, CTA, and/or MR angiography of the aortic arch vessels, we initially punctured both the femoral and the brachial arteries. An 8F guiding catheter was placed into the ostium of the left SCA, and a 7F catheter was inserted into the ipsilateral brachial artery. Systemic heparinization was given to make the activated coagulation time more than 250 seconds.
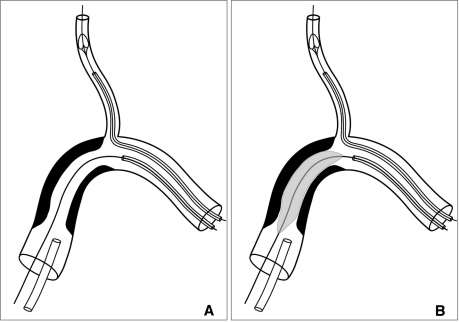
Bilateral selective angiograms or the roadmap were obtained to demonstrate both ends of the occluded left subclavian artery (Fig. 1A). In patient 1, a guidewire was inserted via the femoral guiding catheter into the occluded lesion. Under the landmark of the catheter and/or guidewire which were inserted via the brachial artery into the opposite end of the occluded segment, we probed and crossed through the occluded segment using a catheter via the femoral route. Once a stiff guidewire such as Conquest (Asahi Intecc Co, Ltd, Aichi, Japan), crossed through the occluded segment, a protection device (SpiderFX1, 5-mm, eV3, Plymouth, MN, U.S.A.) was inserted into the vertebral artery via the brachial route (Fig. 2). Then we performed predilation using an angioplasty balloon (Maverick, 2 mm×1.5 cm; Ultrasoft SV, 5×2) followed by stent placement (Precise, Cordis Corp, Miami, FL, U.S.A.). The first balloon was used subsequently to pass the 0.035 guidewire because the occluded lumen was very tight even to pass a balloon. We postdilated with Ultra-soft SV (Boston Scientific Scimed Inc. MN, U.S.A.) via the femoral route.
Fig. 2.
(Modified from reference 9). Procedure diagram of the Landmark-wire technique using a protective device as well as angioplasty balloon via the brachial artery (A) A guidewire passes through the occluded segment via the trans-brachial route. Not a protection device deployed via the same route. (B) Angioplasty is performed via transbrachial route with a protective device in the vertebral artery. Final stenting procedure is performed via transfemoral route (not shown).
In patient 2 who had 3.5 cm long segment occlusion, we probed and crossed through the occluded segment via the brachial route because a guidwire was not crossed the occluded segment from the femoral access route (Fig. 1). To prevent a thromboembolic complication, we placed a protection device (SpiderFX1, 5-mm, eV3, Plymouth, MN, U.S.A.) over another microwire via the brachial route. Via the brachial route, we performed pre-dilatation angioplasty with a balloon of 2 cm diameter and 12 mm length followed by stent placement (Precise, Cordis Corp, Miami,FL, U.S.A.) and postdilated by 7×4 Sterling® Balloon Dilatation Catheter (Boston Scientific Corporation, Natick, MA, U.S.A.)
After the procedure, the patients received 100 mg of aspirin once daily as a permanent medication and 75 mg of clopidogrel once daily for at least six months following the procedure [6, 8, 13].
RESULTS
Technical success was achieved in two patients. We uneventfully crossed the guidewire through the occlusive lesion using the Landmark-wire technique via the femoral catheter in one patient and via the brachial route in another patient. We then predilated stenotic segment with a balloon followed by stenting along the guidewire.
Failure of guidewire passage along the trans-femoral route prevented from the subsequent introduction of both protection device and stenting systems. However, both systems could not be smoothly performed via the 7F sheath of trans-brachial route (Fig. 2). A problem via brachial route was that protection device is prone to be pulled down and caught in the stent strut (Fig. 1B). So the removal of protection device was done using 4F angiocatheter after removal of stent introducer. The post-procedural angiogram showed regained antegrade flow without significant residual stenosis after stenting (Fig. 1C). There were no adverse events during the procedure and no symptom recurrence. CTA of patient 1 showed a good patency with disappearance of symptoms on 13 month follow-up. There was no symptom in patient 2 on one month clinical follow-up.
DISCUSSION
Even though endovascular treatment for subclavian artery stenosis is widely performed [15], endovascular recanalization of subclavian occlusion is confined to a small number of case series [16-20]. This is mostly due to the frequent failed attempts to navigate the occluded segment by transfemoral or trans-brachial approach alone resulting in approximately 70% treatment success rate compared with the 90-100% success rate of subclavian artery stenosis [21, 22].
Recently Liu et al [9]. described Landmark-wire technique that can overcome the difficulties encountered in subclvian revascularization in occlusion cases. Even after crossing through the occluded segment with Landmark-wire technique, there is still a problem how to protect thromboembolism in the reversed vertebral arterial flow. Although patients with SCA occlusion have embolization protection effect due to both subclavian steal phenomenon and delayed restoration of antegrade vertebral flow from 20 seconds up to several minutes [23], the neurological complication rate of subclavian artery angioplasty is in between 0.4% and 4.7% [24-26]. Beck et al [25]. reported the rate of 1% neurological complication rate in 423 subclavian interventions, whereas Angle et al [26]. reported aphasia in one of 21 patients (4.7%) undergoing subclavian angioplasty.
Despite using a distal protection device for carotid artery stenting [27], the use of the protection device in subclavian occlusive disease in a Landmark-wire technique has not been clearly established and how to protect embolism in the vertebral artery is another key aspect of successful subclavian occlusion revascularization procedures.
Our study demonstrated combined use of Landmark-wire technique with a protection device in the vertebral artery. When crossing through the occluded segment was possible with trans-femoral route, as in patient 1, trans-brachial protection device placement followed by trans-femoral presenting balloon and stenting could be done without any problem. However, when crossing through the occluded segment was done via trans-brachial route instead of trans-femoral route as in patient 2, distal protection device together with ballooning and stenting should be done via trans-brachial route. This might result in traction of the protection device during stenting procedure leading to difficult retrieval of the system due to trapping in the stent strut. To avoid such a trapping of the protection device in the stent, final stenting should be done via tran-femoral route after securing the lumen in the occluded segment by angioplasty via trans-brachial route. However, in case there is inadvertent trapping of the protection device as in our patient 2, we recommend using 4F angiocatheter to retrieve the trapped protection device in the stent because a simple angled 4F angiocatheter can be manipulated multidirectionally. Although simultaneous usage of both protection device and stent with 8F trans-brachial could solve these problems, puncture site management can be problematic due to post-procedural hematoma formation.
Regarding the operator's position, we recommend that ordinary position of the operator at the right side of the patient beside the right femoral puncture site would be better. The separate positioning at the femoral as well as the brachial puncture sites would be very inconvenient for the operator to move to two different positions of two puncture sites unless two operators are involved. For such simultaneous operation at two puncture sites, the patient's arm needs to be set just close to the body so that the operator can handle both sites in the parallel direction beside the right femoral puncture site.
If we avoid these problems, there are several advantages of endovascular treatment over surgery. That includes avoidance of surgical complications that is reported as high as 21% including numerous neurologic events, lymphatic fistula, and need for repeat surgery due to postoperative hemorrhage in 3.3% of patients [28]. Other clinical advantages are to reduce the hospital stay and to achieve more rapid postoperative recovery with functional recovery [29].
When occluded segment is crossed via a trans-brachial route in subclavian artery occlusion with Landmark-wire technique, it is more desirable to perform stenting via transfemoral route with a protection device advanced via trans-brachial route. In this way, neither puncture site problem nor friction of the stent and protection device will occur.
Acknowledgement
We acknowledge Sun Moon Whang, B.S. and Eun Hye Kim, R.N. in the patient data collection and the assistance of Eun Ja Yoon in manuscript preparation. This study was supported by a grant from the Korea Healthcare Technology R&D Project, Ministry of Health & Welfare, Republic of Korea. (A080201)
References
- 1.Suh DC, Lee SH, Kim KR, Park ST, Lim SM, Kim SJ, et al. Pattern of atherosclerotic carotid stenosis in Korean patients with stroke: different involvement of intracranial versus extracranial vessels. AJNR Am J Neuroradiol. 2003;24:239–244. [PMC free article] [PubMed] [Google Scholar]
- 2.Suh DC, Ko YB, Park ST, Yoon KH, Lim OK, Oh JS, et al. Computational flow dynamics of the severe M1 stenosis before and after stenting. Neurointervention. 2011;6:13–16. doi: 10.5469/neuroint.2011.6.1.13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.In HS, Lee HY, Park JY, Kim SY, Jung JH, Kim JS, et al. Intracranial stenting in patients with atherosclerotic stenosis associated with various aneurysms in the same diseased arterial segment. AJNR Am J Neuroradiol. 2010;31:1895–1898. doi: 10.3174/ajnr.A2208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Choi JW, Kim JK, Choi BS, Lim HK, Kim SJ, Kim JS, et al. Angiographic pattern of symptomatic severe M1 stenosis: comparison with presenting symptoms, infarct patterns, perfusion status, and outcome after recanalization. Cerebrovasc Dis. 2010;29:297–303. doi: 10.1159/000275508. [DOI] [PubMed] [Google Scholar]
- 5.Choi BS, Park JW, Shin JE, Lu PH, Kim JK, Kim SJ, et al. Outcome evaluation of carotid stenting in high-risk patients with symptomatic carotid near occlusion. Interv Neuroradiol. 2010;16:309–316. doi: 10.1177/159101991001600314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Suh DC, Kim JK, Choi JW, Choi BS, Pyun HW, Choi YJ, et al. Intracranial stenting of severe symptomatic intracranial stenosis: results of 100 consecutive patients. AJNR Am J Neuroradiol. 2008;29:781–785. doi: 10.3174/ajnr.A0922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gonzalez A, Gil-Peralta A, Gonzalez-Marcos JR, Mayol A. Angioplasty and stenting for total symptomatic atherosclerotic occlusion of the subclavian or innominate arteries. Cerebrovasc Dis. 2002;13:107–113. doi: 10.1159/000047759. [DOI] [PubMed] [Google Scholar]
- 8.Pyun HW, Suh DC, Kim JK, Kim JS, Choi YJ, Kim MH, et al. Concomitant multiple revascularizations in supra-aortic arteries: short-term results in 50 patients. AJNR Am J Neuroradiol. 2007;28:1895–1901. doi: 10.3174/ajnr.A0706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Liu S, Hee Jung J, Kwon HJ, Kim SM, Suh DC. Landmark-wire technique of symptomatic subclavian artery occlusion. Interv Neuroradiol. 2009;15:401–405. doi: 10.1177/159101990901500404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Park ST, Kim JK, Yoon KH, Park SO, Park SW, Kim JS, et al. Atherosclerotic carotid stenoses of apical versus body lesions in high-risk carotid stenting patients. AJNR Am J Neuroradiol. 2010;31:1106–1112. doi: 10.3174/ajnr.A2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Liu S, Jung JH, Kim SM, Lim HK, Kwon HJ, Kim JK, et al. Simultaneous bilateral carotid stenting in high-risk patients. AJNR Am J Neuroradiol. 2010;31:1113–1117. doi: 10.3174/ajnr.A1970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kim HJ, Choi BS, Choi JW, Kim SJ, Lee HY, Suh DC. Stent implantation of multichanneled pseudoocclusion of the internal carotid artery. J Vasc Interv Radiol. 2009;20:391–395. doi: 10.1016/j.jvir.2008.12.413. [DOI] [PubMed] [Google Scholar]
- 13.Taylor DW, Barnett HJ, Haynes RB, Ferguson GG, Sackett DL, Thorpe KE, et al. ASA and Carotid Endarterectomy (ACE) Trial Collaborators. Low-dose and high-dose acetylsalicylic acid for patients undergoing carotid endarterectomy: a randomised controlled trial. Lancet. 1999;353:2179–2184. doi: 10.1016/s0140-6736(99)05388-x. [DOI] [PubMed] [Google Scholar]
- 14.Suh DC, Kim JK, Choi CG, Kim SJ, Pyun HW, Ahn C, et al. Prognostic factors for neurologic outcome after endovascular revascularization of acute symptomatic occlusion of the internal carotid artery. AJNR Am J Neuroradiol. 2007;28:1167–1171. doi: 10.3174/ajnr.A0492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Schillinger M, Haumer M, Schillinger S, Mlekusch W, Ahmadi R, Minar E. Outcome of conservative versus interventional treatment of subclavian artery stenosis. J Endovasc Ther. 2002;9:139–146. doi: 10.1177/152660280200900201. [DOI] [PubMed] [Google Scholar]
- 16.Duber C, Klose KJ, Kopp H, Schmiedt W. Percutaneous transluminal angioplasty for occlusion of the subclavian artery: short- and long-term results. Cardiovasc Intervent Radiol. 1992;15:205–210. doi: 10.1007/BF02733923. [DOI] [PubMed] [Google Scholar]
- 17.Sharma S, Kaul U, Rajani M. Identifying high-risk patients for percutaneous transluminal angioplasty of subclavian and innominate arteries. Acta Radiol. 1991;32:381–385. [PubMed] [Google Scholar]
- 18.Martinez R, Rodriguez-Lopez J, Torruella L, Ray L, Lopez-Galarza L, Diethrich EB. Stenting for occlusion of the subclavian arteries. Technical aspects and follow-up results. Tex Heart Inst J. 1997;24:23–27. [PMC free article] [PubMed] [Google Scholar]
- 19.Amor M, Eid-Lidt G, Chati Z, Wilentz JR. Endovascular treatment of the subclavian artery: stent implantation with or without predilatation. Catheter Cardiovasc Interv. 2004;63:364–370. doi: 10.1002/ccd.20173. [DOI] [PubMed] [Google Scholar]
- 20.Mathias KD, Luth I, Haarmann P. Percutaneous transluminal angioplasty of proximal subclavian artery occlusions. Cardiovasc Intervent Radiol. 1993;16:214–218. doi: 10.1007/BF02602963. [DOI] [PubMed] [Google Scholar]
- 21.Domenig CM, Linni K, Mader N, Kretschmer G, Magometschnigg H, Holzenbein TJ. Subclavian to carotid artery transposition: medial versus lateral approach. Eur J Vasc Endovasc Surg. 2008;35:551–557. doi: 10.1016/j.ejvs.2007.12.009. [DOI] [PubMed] [Google Scholar]
- 22.Schillinger M, Haumer M, Schillinger S, Ahmadi R, Minar E. Risk stratification for subclavian artery angioplasty: is there an increased rate of restenosis after stent implantation? J Endovasc Ther. 2001;8:550–557. doi: 10.1177/152660280100800603. [DOI] [PubMed] [Google Scholar]
- 23.Ringelstein EB, Zeumer H. Delayed reversal of vertebral artery blood flow following percutaneous transluminal angioplasty for subclavian steal syndrome. Neuroradiology. 1984;26:189–198. doi: 10.1007/BF00342413. [DOI] [PubMed] [Google Scholar]
- 24.McNamara TO, Greaser LE, Fischer JR, Gobin YP, Duckwiler G. Initial and long-term results of treatment of brachiocephalic arterial stenoses and occlusions with balloon angioplasty, thrombolysis, stents. J Invasive Cardiol. 1997;9:372–383. [PubMed] [Google Scholar]
- 25.Becker GJ, Katzen BT, Dake MD. Noncoronary angioplasty. Radiology. 1989;170:921–940. doi: 10.1148/radiology.170.3.2521745. [DOI] [PubMed] [Google Scholar]
- 26.Angle JF, Matsumoto AH, McGraw JK, Spinosa DJ, Hagspiel KD, Leung DA, et al. Percutaneous angioplasty and stenting of left subclavian artery stenosis in patients with left internal mammary-coronary bypass grafts: clinical experience and long-term follow-up. Vasc Endovascular Surg. 2003;37:89–97. doi: 10.1177/153857440303700202. [DOI] [PubMed] [Google Scholar]
- 27.Wholey MH, Wholey M, Mathias K, Roubin GS, Diethrich EB, Henry M, et al. Global experience in cervical carotid artery stent placement. Catheter Cardiovasc Interv. 2000;50:160–167. doi: 10.1002/(sici)1522-726x(200006)50:2<160::aid-ccd2>3.0.co;2-e. [DOI] [PubMed] [Google Scholar]
- 28.Linni K, Ugurluoglu A, Mader N, Hitzl W, Magometschnigg H, Holzenbein TJ. Endovascular management versus surgery for proximal subclavian artery lesions. Ann Vasc Surg. 2008;22:769–775. doi: 10.1016/j.avsg.2008.08.001. [DOI] [PubMed] [Google Scholar]
- 29.Shah N, Nee LM, Raval AN. Percutaneous revascularization of subclavian artery chronic occlusion with dual cerebral artery protection. Catheter Cardiovasc Interv. 2008;71:992–994. doi: 10.1002/ccd.21520. [DOI] [PubMed] [Google Scholar]