Abstract
Plasmodium vivax malaria has occurred annually in the Republic of Korea (ROK) since its re-emergence in 1993. P. vivax malaria in ROK has been strongly influenced by infected mosquitoes originating from the Democratic People's Republic of Korea. Korean P. vivax malaria has shown typical characteristics of unstable malaria transmitted only during the summer season, and displays short and long incubation periods. The changing pattern of the transmission period can be predicted by analyzing the seasonal characteristics of early primary attack cases with a short incubation period. Such cases began to gradually occur earlier in the 1990s after the re-emergence. Most of the malaria cases after mid-August are presumed to be early primary attack, short incubation period cases. Only primary transmission was possible until the early 2000s, whereas up to fourth or fifth transmission occurred in the mid-2000s. The results indicate that the length of transmission period has been gradually extending, which may be ascribed to a climate change-mediated temperature rise. Malaria and climate data should be integrated to analyze and predict the influence of climate change on malaria occurrence in ROK.
Keywords: Plasmodium vivax malaria, Republic of Korea, Transmission period, Temperature rise, Climate change
INTRODUCTION
Malaria is a vector-borne disease transmitted by the Anopheles mosquito. Plasmodium, the causative agent of malaria, invades erythrocytes of various vertebrates to cause fever, chill, myalgia, hepatosplenomegaly, and, in severe cases, death [1]. Out of the approximately 120 known species of Plasmodium, only four species (P. falciparum, P. vivax, P. ovale, and P. malariae) can cause malaria in humans. Several human cases of P. knowlesi malaria have been reported in Sarawak, Malaysia [2], although whether these cases were transmitted from person to person via infected mosquitoes was not determined.
Approximately 300-500 million cases of malaria occur annually globally among the 2-2.5 billion people living in the affected areas. Among the infected, 1-3 million people die every year, and most of the deaths are children under 5-years-of-age [3]. Therefore, malaria is regarded as a "future threatening" disease in malaria-prevalent countries. P. falciparum and P. vivax malaria account for over 90% of the total malaria cases, and most of the deaths caused by malaria are due to P. falciparum. P. falciparum malaria mostly occurs in tropical areas, whereas P. vivax malaria additionally occurs in subtropical and temperate areas. P. vivax malaria has a wider geographic range than P. falciparum malaria, except for sub-Saharan Africa.
The incidence of malaria decreased sharply following World War II until the 1960s, due to various malaria control projects including aggressive vector control using dichlorodiphenyl-trichloroethane. However, the disease incidence has risen rapidly since the 1990s in many areas in the world including Africa. Temperature rise and rainfall change caused by climate change are suspected of being one of the main causes of the recent malaria spread. Besides climate factors, the end of the cold war by the dismantling of the Soviet Union and the increase of drug-resistant malaria have partially contributed recent malaria spread. Since the 1990s, malaria has increased in many existing malaria endemic areas, and it also re-emerged in some places where malaria had previously been eradicated.
P. vivax malaria was an endemic disease in the Republic of Korea (ROK) until the 1970s. The first scientific description of Korean P. vivax malaria was in 1913 [4]. The manuscript refers to a long protracted incubation period in Korean P. vivax malaria cases. During the Korean War (1950-1953), many soldiers of the United States (U.S.) Army suffered from malaria, which prompted intensive research by the U.S. Army on the disease. Biological and epidemiological characteristics of the long incubation period, which is the most unique feature of the temperate P. vivax strain, were elucidated and a therapeutic regimen utilizing primaquine was established to eradicate the hypnozoites that hibernated in liver cells during the protracted incubation period [5-8]. In the aftermath of the Korean War, malaria decreased sharply in ROK by an aggressive malaria control project supported by the World Health Organization (WHO), a vector control project, and improved nutritional status caused by economic growth. ROK was declared "malaria elimination" in 1979 [9], even though focal indigenous cases continued to be reported until 1984. After re-emergence in 1993, P. vivax malaria has occurred annually in ROK and the epidemiological characteristics have changed since 2000. It is this recent epidemiological change that was the subject of the present study. The relationship to climate change was analyzed.
MAIN SUBJECT
I. Re-Emergence of P. vivax Malaria in ROK
Since the first case was diagnosed in 1993 in a ROK Army soldier stationed in Paju County, near the Demilitarized Zone (DMZ) that divides ROK and the Democratic People's Republic of Korea (DPRK), P. vivax malaria rapidly increased in areas near the DMZ [10]. Based upon epidemiological data, P. vivax malaria in ROK might be directly influenced by infected mosquitoes originating from DPRK. DPRK did not confirm malaria occurrence in their country until 1999, when they asked WHO to support malaria control efforts in the nation. During the 1990s after re-emergence of the disease, more than half of the total annual cases were from active military personnel and veterans within 24 months after discharge from military service. However, since 2000, civilian cases have accounted for over half of the total annual cases, and the geographical areas associated with malaria transmission have expanded southward from the DMZ [11-13].
II. Biological Characteristics of P. vivax Malaria in ROK
Malaria can be transmitted throughout the year in tropical areas despite the difference in malaria incidence between dry and wet seasons. In subtropical and temperate areas, the activity of the vector mosquito is greatly influenced by temperature, which results in seasonal variation. In particular, malaria transmission is restricted or totally impossible during the winter season, a pattern referred to as unstable malaria. Vector efficiency of these areas is lower than in regions where malaria is endemic. During the winter season, when malaria transmission ceases, P. vivax and P. ovale hibernate in liver cells as a hypnozoite. Hypnozoites developed to tissue schizonts when the temperature elevates in the spring, beginning another cycle of malaria transmission. P. vivax exhibits two different kinds of incubation periods: short and long (or intermediate). Sporozoites introduced by an infected female mosquito invade liver cells within 0.5-1 hour after introduction. If the sporozoite develops to a tissue schizont immediately, the incubation period between the introduction of sporozoite and the first symptom onset is typically 10 days to 2 weeks. This is the short incubation period, which results in an early primary attack [1,5]. Conversely, if the sporozoite develops to a hypnozoite rather than a tissue schizont in liver cells, the parasite can dwell in these cells for more than 1 year prior to conversion to the tissue schizont and the onset of illness. This represents the long incubation period and is the late primary attack [1,5]. The length of the incubation period between the introduction of sporozoite and the onset of the first symptom in cases of late primary attack depends upon the geographical region. In subtropical areas, cases having an intermediate incubation period of 4-6 months are frequent, while cases in temperate regions more often have an incubation period exceeding 8 months. It is possible that different kinds of parasites with different incubation periods are mixed in the same sporozoite inoculum. In some cases, malaria can occur after a long incubation period after the symptoms of early primary attack subside; this represents a relapse case. Late primary attack and relapse cases are discriminated only by the existence of early primary attack before relapse [5]. Relapse cases are very rare in ROK due to the extensive use of primaquine to eradicate hypnozoites and the very low primaquine treatment failure rate in Koreans. Therefore, P. vivax malaria cases with a long incubation period that have occurred in ROK after re-emergence are likely mostly late primary attack cases. There is no hypnozoite stage in the life cycle of P. falciparum. Thus, indigenous P. falciparum malaria occurrence remains impossible in ROK, since P. falciparum cannot survive in humans during the winter season.
III. Changing Pattern of P. vivax Malaria Due to Climate Change
It is plausible that P. vivax malaria re-emerged in DPRK, where is less a favorable environment for malaria transmission than ROK due to the higher latitude, earlier than in ROK. The reasons include collapse of the health care system and poorer nutritional status due to the economic crisis that occurred after the dismantling of the Soviet Union in 1990, expansion of Anopheles mosquito habitat caused by deforestation and repeated flood in the mid-1990s. It is also very plausible that climate change has been one of the main drivers of P. vivax malaria re-emergence and spread in DPRK. Malaria is directly influenced by climate, since the number and geographical range of the Anopheles mosquito are affected by rainfall, temperature, and humidity [14]. The temperature rise that has and continues to be caused by climate change results in malaria emergence in highlands of malaria endemic areas or in high latitude areas like DPRK, where it was formerly too cold for the mosquito-mediated transmission of malaria [15,16]. A strong argument can be made that climate change has influenced, perhaps in a primary fashion, P. vivax malaria re-emergence in DPRK, which had been malaria-free area for over a decade previously, and the spread of the disease to ROK. Among the basic epidemiological factors, which include location, time, and human involvement, the first two factors can be influenced by climate change. It is difficult to trace the influence of climate change on location in ROK, since malaria transmission areas have been restricted near the DMZ. Use of malaria data from DPRK is a forlorn hope, since the data is strictly controlled and restricted, and the changing pattern of location could have been altered by the aggressive malaria control project that was undertaken. However, it is possible to analyze the influence of climate change using the time factor (i.e., the 10-day incidence of P. vivax malaria in ROK). Understanding the epidemiological characteristics of late primary attack cases with a long incubation period and early primary attack cases with a short incubation period, which are unique features of temperate P. vivax strains, is a prerequisite to decipher the time factor of P. vivax malaria in ROK.
IV. Epidemiological Characteristics of a Long and a Short Incubation Periods of P. vivax
Epidemiological characteristics of a long incubation period of Korean P. vivax malaria were revealed through the U.S. Army sponsored research during the Korean War. Epidemiological characteristics included relapse and late primary attack cases, biological features of a long incubation period and hypnozoites, and the research established the radical primaquine treatment regimen to eradicate hypnozoites in human liver cells [6-8]. During the Korean War, the use of primaquine had not been fully implemented yet. As a consequence, most of the American soldiers, who served for one year in ROK before being evacuated to the malaria-free confines of U.S., were suitable to investigate the characteristics of a long incubation period. The seasonal occurrence pattern of early and late primary attack cases should be analyzed epidemiologically since they are not discriminated by their clinical features. The current military service condition of the ROK Army is quite different from that of the U.S. Army during the Korean War, making newer methods of investigation necessary. The seasonal occurrence pattern of P. vivax malaria in ROK can be partially analyzed because malaria transmission areas have been restricted near the DMZ after the re-emergence, most military personnel stationed in malaria transmission areas lived in malaria non-transmission areas before their military service, and veterans usually live in malaria non-transmission areas after discharge from military service.
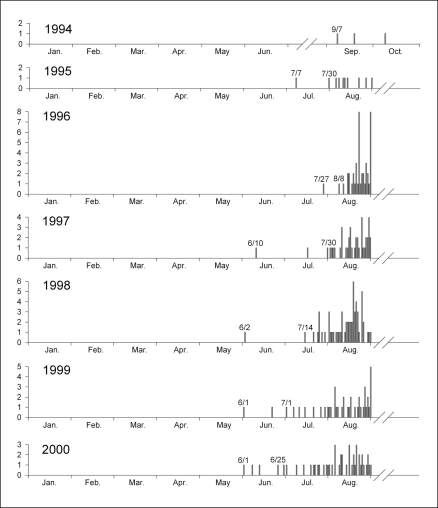
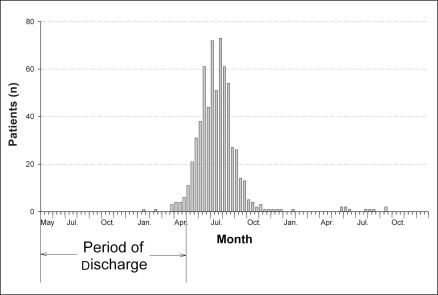
P. vivax malaria cases among soldiers who entered military service in or after November of the previous year might be mostly early primary attack cases with a short incubation period. To determine when malaria transmission had begun, such cases were examined. The first case of early primary attack with a short incubation period occurred in or after late July in the mid-1990s. However, occurrence gradually became earlier, occurring in early June in 2000, and early primary attack cases began to occur in a group in late July (Figure 1) [10]. On the other hand, P. vivax malaria cases among veterans who dwelled in malaria non-transmission areas for two consecutive malaria transmission seasons after their discharge might be mostly late primary attack cases with a long incubation period. The first primary attack cases among veterans began to occur in a group from late March and occurred mainly during the first transmission season after their discharge, with the peak between mid-June and mid-August. Their occurrence fell sharply in late August of the first transmission season after their discharge. Among the total examined first primary attack cases, 98.5% occurred during the year after discharge (Figure 2) [13]. This seasonal pattern of the first primary attack cases of P. vivax malaria in veterans is quite similar to that observed during the Korean War [2], which implies that the basic biological characteristics of P. vivax regarding relapse have been maintained. Based upon the aforementioned seasonal pattern of early and late primary attack cases, it is plausible that late primary attack cases with a long incubation period that were infected in the previous year constituted most of the total cases until mid-July, and that, after mid-August, early primary attack cases with a short incubation period that were infected in the same year predominated. Between late-July and mid-August, early and late primary attack cases occurred together, which was the main reason for the highest incidence during this period. The finding of an earlier time point of the first early primary attack case in 2000 as compared to the mid-1990s is explainable by an earlier commencement of malaria transmission by Anopheles mosquitoes.
Figure 1.
Date of diagnosis for the Republic of Korea military personnel without previous exposure to malaria in the preceding year.
The y-axis of each graph represents the number of patients. Data are from reference [10].
Figure 2.
Number of the first late primary attack cases of Plasmodium vivax malaria among veterans discharged from the military between May 2003 and April 2006, during two consecutive malaria-transmission seasons after their discharge.
Data are from reference [13].
V. Changing Pattern of Transmission Period of P. vivax Malaria in ROK
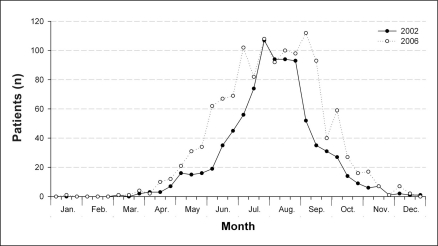
After mid-August, there occurs a meaningful change in the seasonal pattern of malaria occurrence, when early primary attack cases account for most of the total cases. Seasonal pattern of P. vivax malaria among military personnel may be distorted, since mass chemoprophylaxis has been performed in the military on a large scale since 1997 [17]. The seasonal pattern of P. vivax malaria among veterans also cannot reflect the natural appearance, since most of the cases are late primary attack cases with a long incubation period. For these reasons, P. vivax malaria cases among civilians represent the most adequate model to accurately analyze the seasonal pattern of P. vivax malaria in ROK. The 10-day incidence peaked between late-July and mid-August until the early 2000s [10,11]. Henceforth, the 10-day incidence in late-August or later has increased, reaching its highest peak in early September of 2006 (Figure 3) [12,13]. We can conclude that more early primary attack cases have occurred in or after late-August in the new millennium compared to the 1990s, and that the first early primary cases have been gradually occurring earlier. This means that the time point of early primary attack case occurrence has been extended in an oscillating fashion, with the malaria transmission period becoming gradually extended. The climatic factor that is the most likely influence on malaria transmission in high latitude areas like ROK is temperature rise, which can extend the season adequate for flight and feeding activity of the vector mosquito. In high latitude areas, increased rainfall may result in increased malaria incidence during a short period caused by the increased vector population during that period, whereas temperature rise may result in increased incidence during early summer (or late spring) and autumn seasons caused by the extended transmission period.
Figure 3.
Number of Plasmodium vivax malaria cases among civilians reported at 10-day intervals, in 2002 and 2006 in the Republic of Korea.
Data are from reference [13].
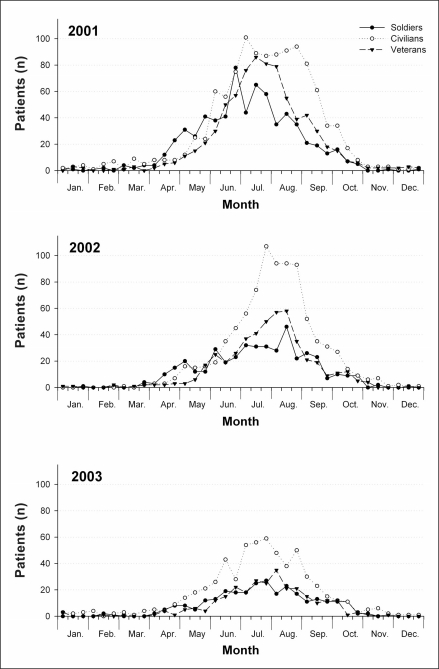
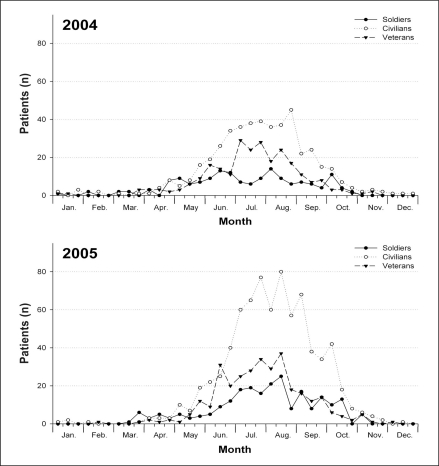
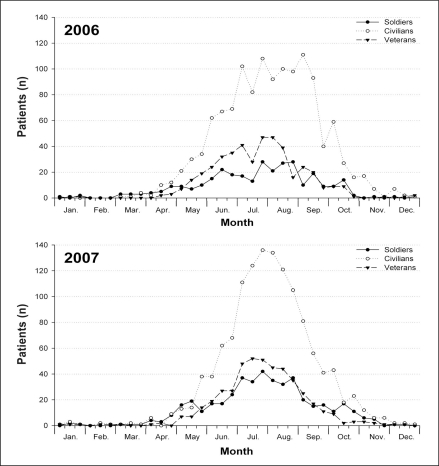
Considering the time required for parasite development in the vector mosquito and the length of a short incubation period, the period of transmission from malaria patients (via vector mosquito) to manifestation as early primary attack cases would be 3-4 weeks. Therefore, continuous transmission by an extended transmission period could register as a minor peak of incidence in the same time interval. The 10-day incidence had decreased steadily after late August until 2004, despite a minor peak in mid-September of that year (Figure 4,5) [11,12]. However, minor peaks were found two times in early September and early October in 2005, and in 2006, they were found four times in early September, early October, early November, and early December (Figure 6) [12,13]. A minor peak was not evident in 2007, because of the effects of an aggressive intervention campaign involving mass chemoprophylaxis with primaquine on five million people in DPRK during the first half of 2007. P. vivax malaria occurrence in ROK is still strongly influenced by the malaria situation in DPRK, and the overall transmission cycle was affected in 2007, since the mass primaquine chemoprophylaxis in DPRK may have eradicated hypnozoites under a long incubation period, removing the primary infection source for early primary attack cases in ROK.
Figure 4.
Number of Plasmodium vivax malaria cases of soldiers, civilians, and veterans, reported at 10-day intervals, from 2001 through 2003 in the Republic of Korea.
Data are from reference [11].
Figure 5.
Number of Plasmodium vivax malaria cases of soldiers, civilians, and veterans, reported at 10-day intervals, from 2004 through 2005 in the Republic of Korea.
Data are from reference [12].
Figure 6.
Number of Plasmodium vivax malaria cases of soldiers, civilians, and veterans, reported at 10-day intervals, from 2006 through 2007 in the Republic of Korea.
Data are from reference [13].
Active transmission of P. vivax malaria can start by the occurrence of late primary attack cases over a certain level and the existence of a sufficient population of vector mosquitoes. Considering these conditions, active transmission may begin in or after early-July and, consequently, malaria incidence increases in early- to mid-August. These increased cases may act as an infection source for the subsequent transmission cycle, which results in the appearance of a minor peak every 3-4 weeks thereafter. Until 2003, the second and the third transmission cycles after the first transmission cycle seldom occurred. However, increased transmission has become possible as the malaria transmission period has been extended. The scanty presence of a minor peak in mid-September in 2004 is consistent with the scenario that the weak second transmission might have occurred in that year, and the second and the third transmission cycles might have actively occurred in 2005. Active transmission cycles were evident five times in 2006, and P. vivax malaria could be transmitted even in early November in 2006 in certain malaria transmission areas.
VI. Forecast of Future Changing Pattern of Malaria Occurrence in ROK by Climate Change
It is questionable whether malaria can be transmitted even during the winter season in ROK as the malaria transmission period becomes extended. The mean temperature during the winter season (from December to March of the following year) is too low for Anopheles mosquito activity. Under this climate condition, malaria transmission throughout the year would not be possible and indigenous cases of P. falciparum malaria will not occur in ROK in the near future. However, focal P. falciparum malaria outbreaks by imported cases may be possible, since the Anopheles mosquito is the dominant genus in most ROK rural areas even if the transmission efficacy of this species is quite low in ROK. However, P. falciparum cannot survive during the winter season, given the absence of the hypnozoite stage in their life cycle. If the climatic conditions of the southern part of ROK transform to subtropical, the distribution of the Anopheles mosquito will be affected, enabling indigenous P. falciparum malaria to become established. The transmission period and transmission areas of P. vivax malaria in ROK will also appreciably extended under that climatic condition comparing to the present.
CONCLUSIONS
The changing seasonal incidence pattern of P. vivax malaria after re-emergence shows that malaria transmission period has been extended in ROK, mainly due to temperature rise caused by climate change. The first early primary attack case had begun to occur gradually earlier in the 1990s, which is closely related to the start point of annual malaria transmission. Since the mid-2000s, more transmission cycles up to the fifth cycle have occurred and, consequently, P. vivax malaria has been actively transmitted in ROK during the autumn season, a time when transmission seldom occurred. The transmission environment has become increasingly favorable for the activity of vector mosquitoes. An extended transmission period might be ascribed to temperature rise caused by climate change, which increases the likelihood of Anopheles-mediated transmission during the autumn season. The specter of continued climate change means that this trend will also continue. Analysis of malaria and weather data should be integrated to further investigate the relationship between climate change and changing pattern of malaria occurrence in ROK.
Footnotes
This article is available from: http://e-eht.org/
References
- 1.Sinden RE, Gilles HM. The malaria parasites. In: Warrell DA, Gilles HM, editors. Essential Malariology. 4th ed. London: Arnold; 2002. pp. 8–34. [Google Scholar]
- 2.Cox-Singh J, Singh B. Knowlesi malaria: newly emergent and of public health importance? Trends Parasitol. 2008;24(9):406–410. doi: 10.1016/j.pt.2008.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sachs J, Malaney P. The economic and social burden of malaria. Nature. 2002;415(6872):680–685. doi: 10.1038/415680a. [DOI] [PubMed] [Google Scholar]
- 4.Hasegawa Y. Malaria in Korea. Chosun Igakkai Zasshi. 1913;4:53–69. [Google Scholar]
- 5.Hankey DD, Jones R, Jr, Coatney GR, Alving AS, Coker WG, Garrison PL, et al. Korean vivax malaria. I. Natural history and response to chloroquine. Am J Trop Med Hyg. 1953;2(6):958–969. [PubMed] [Google Scholar]
- 6.Alving AS, Hankey DD, Coatney GR, Jones R, Jr, Coker WG, Garrison PL, et al. Korean vivax malaria. II. Curative treatment with pamaquine and primaquine. Am J Trop Med Hyg. 1953;2(6):970–976. [PubMed] [Google Scholar]
- 7.Jones R, Jr, Jackson LS, Lorenzo AD, Marx RL, Levy BL, Kenny EC, et al. Korean vivax malaria. III. Curative effect and toxicity of primaquine in doses from 10 to 30 mg. daily. Am J Trop Med Hyg. 1953;2(6):977–982. [PubMed] [Google Scholar]
- 8.Coatney GR, Alving AS, Jones R, Jr, Hankey DD, Robinson DH, Garrison PL, et al. Korean vivax malaria. V. Cure of the infection by primaquine administered during long-term latency. Am J Trop Med Hyg. 1953;2(6):985–988. [PubMed] [Google Scholar]
- 9.World Health Organization. Synopsis of the world malaria situation in 1979. Wkly Epidemiol Rec. 1981;56:145–149. [Google Scholar]
- 10.Park JW, Klein TA, Lee HC, Pacha LA, Ryu SH, Yeom JS, et al. Vivax malaria: a continuing health threat to the Republic of Korea. Am J Trop Med Hyg. 2003;69(2):159–167. [PubMed] [Google Scholar]
- 11.Yeom JS, Ryu SH, Oh S, Lee WJ, Kim TS, Kim KH, et al. Status of Plasmodium vivax malaria in the Republic of Korea during 2001-2003. Am J Trop Med Hyg. 2005;73(3):604–608. [PubMed] [Google Scholar]
- 12.Yeom JS, Kim TS, Oh S, Sim JB, Barn JS, Kim HJ, et al. Plasmodium vivax malaria in the Republic of Korea during 2004-2005: Changing patterns of infection. Am J Trop Med Hyg. 2007;76(5):865–868. [PubMed] [Google Scholar]
- 13.Jun G, Yeom JS, Hong JY, Shin EH, Chang KS, Yu JR, et al. Resurgence of Plasmodium vivax malaria in the Republic of Korea during 2006-2007. Am J Trop Med Hyg. 2009;81(4):605–610. doi: 10.4269/ajtmh.2009.09-0111. [DOI] [PubMed] [Google Scholar]
- 14.Snow RW, Gilles HM. The Anopheles vector. In: Warrell DA, Gilles HM, editors. Essential Malariology. 4th ed. London: Arnold; 2002. pp. 59–84. [Google Scholar]
- 15.Martens WJ, Niessen LW, Rotmans J, Jetten TH, McMichael AJ. Potential impact of global climate on malaria risk. Environ Health Perspect. 1995;103(5):458–464. doi: 10.1289/ehp.95103458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Martens P, Kovats RS, Nijhof S, de Vries P, Livermore MTJ, Bradley DJ, et al. Climate change and future population at risk of malaria. Glob Environ Change. 1999;9:S89–S107. [Google Scholar]
- 17.Yeom JS, Ryu SH, Oh S, Choi DH, Song KJ, Oh YH, et al. Evaluation of anti-malarial effects of mass chemoprophylaxis in the Republic of Korea army. J Korean Med Sci. 2005;20(5):707–712. doi: 10.3346/jkms.2005.20.5.707. [DOI] [PMC free article] [PubMed] [Google Scholar]