Abstract
To describe a non-penetrating TASER gun injury resulting in a small exudative retinal detachment but significant visual acuity and retinal function loss as demonstrated by electroretinography (ERG). A 39-year-old man presented to the emergency department with a TASER barb embedded in his right lower lid. A complete clinical ophthalmologic examination and surgical extrication were performed, as well as radiologic imaging and Ganzfeld electroretinography. No scleral penetration was observed on surgical exploration. Retinal examination showed a peripheral exudative detachment. Subsequent follow-up revealed progressive resolution of the detachment and improvement in visual acuity. The ERG showed a 63–70% decrease in rod a- and b-waves, while isolated cone responses were reduced by only 10%, with a minimal increase in implicit time. This case shows that periocular TASER injuries, even if apparently superficial, may result in significant ocular damage. ERG may be useful in the diagnosis of visual loss attributed to disturbance in photoreceptor function, in the absence of anatomically evident damage.
Keywords: Electrical injury, Electroretinogram, Eye, Ocular injury, Retinal detachment, TASER, Trauma
Introduction
Thomas A. Swift's electric rifle—TASER (TASER International, Scottsdale, AZ)—is a battery-powered unit that uses a nitrogen cartridge to propel two darts up to 35 ft at a rate of 160 ft/s. The darts, connected by a wire, attach to the individual's skin or clothing, delivering up to 50,000 V of electricity for up to 5 s [1]. The completed circuit incapacitates the subject by causing involuntary muscular contraction and tetany. It is considered a safer alternative to more conventional weapons. A recent prospective, multicenter trial showed that less than 1.4% of TASER victims experienced significant injury, which most often was associated with penetration of face, neck, or groin [2]. TASERs are used as a form of sublethal force by law enforcement agencies to subdue violent or agitated offenders. The National Institute of Justice reports that more than 260,000 officers carry a TASER. Additionally, more than 120,000 US citizens are estimated to carry a TASER for personal protection. The increasing popularity of the TASER may lead to increasing incidence of related ocular injuries.
Case report
A 39-year-old man was brought to the emergency department after being subdued with a TASER gun by the police. The TASERing resulted in immediate loss of consciousness. Three TASER prongs were found on the patient's clothing, and a fourth was found firmly embedded medially in his right lower lid (Fig. 1). His visual acuity on presentation was 20/400 in the right eye and 20/20 in the left eye. Pupil reactions and confrontational visual fields were normal. Ocular motility was full, with mild pain on upgaze. The intraocular pressures were 20 and 14 mmHg in the right and left eyes, respectively. A TASER probe was embedded in the right lower eyelid with a corresponding laceration and surrounding ecchymosis. However, no electrical burn was observed on the eyelid skin. A small subconjunctival hemorrhage was noted nasally in the right eye. Corneas and lenses were clear, and irides intact. Anterior chambers were formed without inflammation. Dilated fundus examination of the right eye showed a string of retinal hemorrhages surrounding a large area of subretinal hemorrhage inferonasally, measuring approximately 3 disk-diameters in extent (Fig. 2). No retinal tear was identified. The vitreous was clear with no evidence of cells in the anterior vitreous. A CT scan of the orbits showed intact globes, and localized the prong in the right lower lid, extending into the anterior orbit, with the tip terminating in the right lacrimal fossa. There was no radiographic evidence of rectus muscle involvement (Figs. 3, 4).
Fig. 1.

External photograph of the right eye showing the TASER dart firmly embedded in the lower lid
Fig. 2.
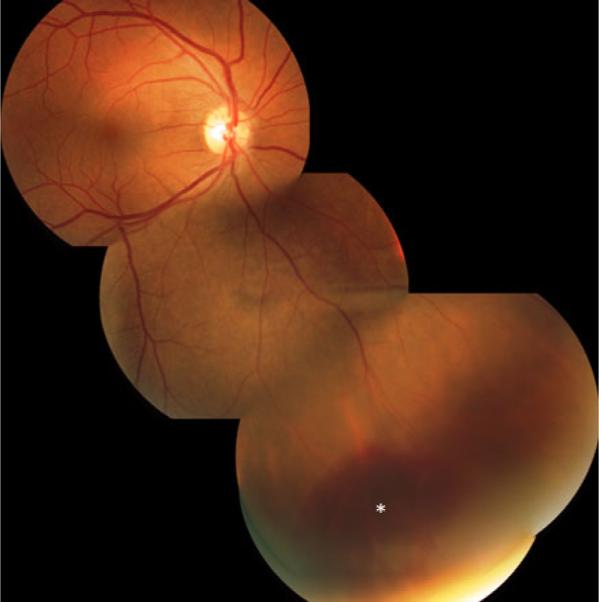
Fundus photograph taken after the resolution of the exudative retinal detachment induced by the TASER. The resolving subretinal hemorrhage, as well as the adjacent smaller retinal hemorrhages, and pigmented scars are seen (asterisk). The montage shows the size and location of the detachment in relation to the posterior pole
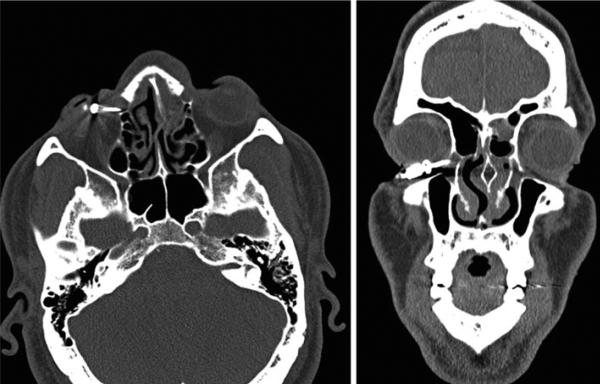
Fig. 3.
(Left) Axial view of the orbital CT scan showing the tip of the TASER dart in the right lacrimal fossa. (Right) Coronal section of the orbital CT scan. No evidence of globe or muscular lesion. The hemorrhagic fluid in left ethmoidal cells is the result of a broken nose, from a fall sustained after being “TASERed”
Fig. 4.

Three-dimensional reconstructed CT image showing the location of the dart in the anterior orbit
The patient was taken to the operating room for extraction of the prong under general anesthesia. The tip of the prong was found in the inferior anterior orbit with intact underlying sclera. Globe exploration and irrigation of the lacrimal system revealed no injury to these structures. An incision was made in the conjunctiva directly over the tip of the prong, and the electrode was removed by pulling it through the incision.
The initial area of subretinal hemorrhage progressed into an exudative retinal detachment over the following 3 days. A Ganzfeld electroretinogram (UTAS-E 2000, LKC Technologies, Inc, Gaithersburg, MD), following the ISCEV standard for clinical electrophysiology [3], was performed on our patient at this time and showed a 63–70% decrease in a- and b-wave amplitudes for rods when compared to the fellow normal eye, but only a 10% reduction in cone amplitudes. Cone responses were also delayed by 1–2 ms (Fig. 5). Over the next 2 months, the retinal detachment gradually resolved, leaving a few residual intraretinal hemorrhages and some hyperpigmented scars. Visual acuity progressively improved over 2 months time to 20/25. No new complications developed over this period of time. Unfortunately, the patient was lost to follow-up, and we were unable to assess for late sequelae of the injury.
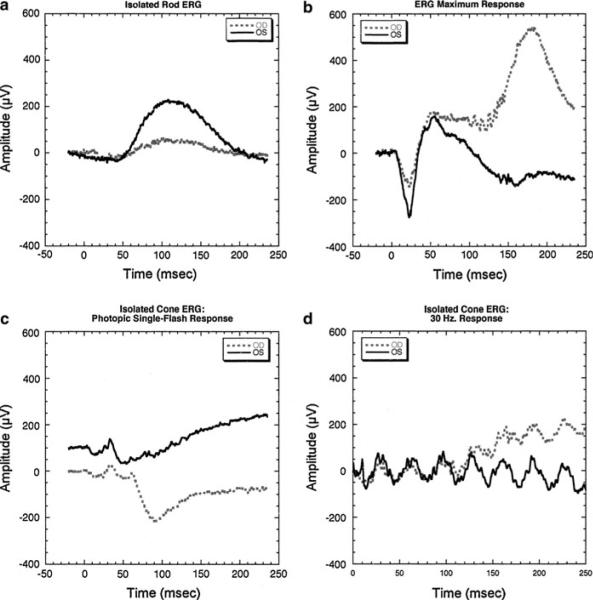
Fig. 5.
Ganzfeld electroretinogram performed 3 days after the TASER injury. a Isolated rod responses of the affected eye (OD; gray dashed line) compared to the concomitant response from the normal eye (OS; dark solid line). There is a 70% reduction in the b-wave amplitude of the affected relative to the fellow eye. b The ERG maximum response shows about a 63% reduction in the rod photoreceptor response, consistent with the b-wave reduction in a, and suggesting that the b-wave reduction results from reduced photoreceptor responses. The reduction in ERG amplitude in a and b is greater than what would be expected from the extent and location of the observed exudative retinal detachment. c Isolated cone responses to a single flash of light. Responses are vertically displaced for comparison. The response from the affected eye is reduced 10% when compared to the normal eye and is minimally delayed by 1–2 ms. d Isolated cone responses to a 30-Hz flickering light reflect the minimal amplitude and timing changes observed in c
Discussion
To our knowledge, there are few reports in the literature describing ocular injuries inflicted by TASERs. One describes an electrical injury to the eye [4], and the remaining, a penetrating mechanical injury to the globe [5–8]. To our knowledge, this is the first report of a non-penetrating injury to the retina caused by a TASER, expanding thus the spectrum of possible injuries caused by the device.
The retinal damage observed in our patient can be theoretically attributed to 3 mechanisms: electrical, thermal, and/or traumatic/mechanical damage.
A wide range of ocular disorders have been described following electrical injury [9]. These occur by direct transmission of the electrical current through the tissue, conversion of electrical energy into thermal energy absorbed by the tissue, end-organ ischemia caused by generalized vascular constriction, or a combination of these mechanisms. In our patient, the localized peripheral retinal injury could have resulted from thermal damage, resulting in an exudative retinal detachment similar to what may be seen after diathermy. Skin burns near the probe location are frequently observed in TASER injuries.
While ocular mechanical trauma from the TASER dart could potentially explain the observed clinical findings, the ERG changes and the significant drop in visual acuity experienced by our patient make it less likely to be the exclusive etiology. On ERG, the rod a-wave reduction localizes function loss to the photoreceptor layer. The large reduction in rod photoreceptor function appears to be out of proportion to the observed anatomical damage. Notably, the changes in ERG implicit times were minimal, which indicates that retinal sensitivity remained normal as the size of the response declined. This pattern of ERG loss is more consistent with a large area of retina being affected or a diffuse retinal injury, and not the focal injury seen in the peripheral retina. According to the Hood and Birch model of rod photoreceptor transduction [10], possible mechanisms may include complete loss of a large area of rod photoreceptors with normal photoreceptors elsewhere, a reduction in outer segment length, or a loss of membrane conductance. A proposed mechanism of lightning strike–induced retinal damage is prolonged neural depolarization, which could affect the strength of the photoreceptor response through a change in membrane conductance. Similar ERG findings were previously described following electrical lightning injury [11]. The lack of evidence of further electrical injury to the eye, like cataracts, may be attributed to the relatively short duration of follow-up.
In conclusion, periocular TASER injuries, even if apparently superficial, may result in significant ocular damage. ERG may be useful in the diagnosis of visual loss attributed to disturbance in photoreceptor function, especially in the absence of a significant amount of anatomically evident damage.
Acknowledgments
This work was supported in part by a grant from Research to Prevent Blindness (MAJ) and by National Institutes of Health grant #1KO8EY016357-01A2 (MKM).
References
- 1.TASER promotional literature. http://taser.com/products/personal-safety/taser-c2. Accessed 1 May 2009.
- 2.Bozeman WP, Hauda WE, II, Heck JJ, Graham DD, Jr, Martin BP, Winslow JE. Safety and injury profile of conducted electrical weapons used by law enforcement officers against criminal suspects. Ann Emerg Med. 2009;53:480–489. doi: 10.1016/j.annemergmed.2008.11.021. [DOI] [PubMed] [Google Scholar]
- 3.Marmor MF, Fulton AB, Holder GE, Miyake Y, Brigell M, Bach M. ISCEV Standard for full-field clinical electroretinography (2008 update) Doc Ophthalmol. 2009;118:69–77. doi: 10.1007/s10633-008-9155-4. [DOI] [PubMed] [Google Scholar]
- 4.Seth RK, Abedi G, Daccache AJ, Tsai JC. Cataract secondary to electrical shock from a Taser gun. J Cataract Refract Surg. 2007;33:1664–1665. doi: 10.1016/j.jcrs.2007.04.037. [DOI] [PubMed] [Google Scholar]
- 5.Teymoorian S, San Filippo AN, Poulose AK, Lyon DB. Perforating globe injury from Taser trauma. Ophthal Plast Reconstr Surg. 2010;26:306–308. doi: 10.1097/IOP.0b013e3181c15c36. [DOI] [PubMed] [Google Scholar]
- 6.Han JS, Chopra A, Carr D. Ophthalmic injuries from a TASER. CJEM. 2009;11:90–93. doi: 10.1017/s1481803500010976. [DOI] [PubMed] [Google Scholar]
- 7.Chen SL, Richard CK, Murthy RC, Lauer AK. Perforating ocular injury by Taser. Clin Experiment Ophthalmol. 2006;34:378–380. doi: 10.1111/j.1442-9071.2006.01228.x. [DOI] [PubMed] [Google Scholar]
- 8.Ng W, Chehade M. Taser penetrating ocular injury. Am J Ophthalmol. 2005;139:713–715. doi: 10.1016/j.ajo.2004.11.039. [DOI] [PubMed] [Google Scholar]
- 9.Miller BK, Goldstein MH, Monshizadeh R, Tabandeh H, Bhatti MT. Ocular manifestations of electrical injury: a case report and review of the literature. CLAO J. 2002;28:224–227. doi: 10.1097/01.ICL.0000032345.79593.24. [DOI] [PubMed] [Google Scholar]
- 10.Hood DC, Birch DG. A computational model of the amplitude and implicit time of the b-wave of the human ERG. Vis Neurosci. 1992;8:107–126. doi: 10.1017/s0952523800009275. [DOI] [PubMed] [Google Scholar]
- 11.Yi C, Liang Y, Jiexiong O, Yan H. Lightning-induced cataract and neuroretinopathy. Retina. 2001;21:526–528. doi: 10.1097/00006982-200110000-00017. [DOI] [PubMed] [Google Scholar]