Abstract
Links between positive affect (PA) and health have predominantly been investigated by using measures of recollected emotional states. Ecological momentary assessment is regarded as a more precise measure of experienced well-being. We analyzed data from the English Longitudinal Study of Aging, a representative cohort of older men and women living in England. PA was assessed by aggregating momentary assessments over a single day in 3,853 individuals aged 52 to 79 y who were followed up for an average of 5 y. Respondents in the lowest third of PA had a death rate of 7.3%, compared with 4.6% in the medium-PA group and 3.6% in the high-PA group. Cox proportional-hazards regression showed a hazard ratio of 0.498 (95% confidence interval, 0.345–0.721) in the high-PA compared with the low-PA group, adjusted for age and sex. This was attenuated to 0.646 (95% confidence interval, 0.436–0.958) after controlling for demographic factors, negative affect, depressed mood, health indicators, and health behaviors. Negative affect and depressed mood were not related to survival after adjustment for covariates. These findings indicate that experienced PA, even over a single day, has a graded relationship with survival that is not caused by baseline health status or other covariates. Momentary PA may be causally related to survival, or may be a marker of underlying biological, behavioral, or temperamental factors, although reverse causality cannot be conclusively ruled out. The results endorse the value of assessing experienced affect, and the importance of evaluating interventions that promote happiness in older populations.
Keywords: positive well-being, mortality, aging
Subjective well-being is being increasingly seen as an indicator of societal progress (1), and some countries are beginning to establish national well-being surveys (2). There is evidence that positive affective states and other measures of well-being are associated prospectively with longer survival and reduced risk of diseases of older age (3–9). Effects are maintained after initial health status and established risk factors are taken into account, and may also be independent of negative states such as depression (3, 10).
To date, studies relating positive well-being with mortality have mainly relied on assessments of recollected emotional states, in which people are asked to rate their feelings of happiness or well-being in general, either without any time frame (5, 6, 9, 11, 12) or over a specific time period such as the previous 4 wk (4, 8, 10, 13, 14). Psychological research has established that recollected affect may diverge from actual experience because it is influenced by errors in recollection, recall biases, focusing illusions, and salient memory heuristics (15, 16). This “memory–experience gap” between life as it is remembered and life as it is experienced may be important to the processes through which the past impacts on future behavior (17).
Methods of overcoming the limitations of retrospective measures include the use of ecological momentary assessment (EMA) (18), and methods involving recall of the day before such as the day reconstruction method (19) and single or repeated assessments of the previous day (20, 21). EMA is the only “real-time” procedure involving the collection of a number of ratings of how a person feels over a period of time. It allows variations in mood over time and in relation to events to be explored (22). Here, we report the association between PA measured by using EMA and mortality over an average 5-y follow-up period in a large sample of men and women aged 52 to 79 y. We also evaluated the prognostic significance of negative affective states.
Results
Participants in the English Longitudinal Study of Aging (ELSA) who completed EMA over one 24-h period were divided into three PA groups based on the average of the momentary ratings. Those reporting higher PA were slightly younger and more likely to be male and married (Table 1). There were no differences in ethnicity, paid employment, or education, but a marginal difference in wealth. Higher PA was associated with less negative affect over the same day, lower depression scores, and less diagnosed depression in the previous 2 y. People with higher PA also reported better self-rated health, but there were no differences in the prevalence of serious illnesses including cancer, coronary heart disease (CHD), stroke, diabetes, and chronic lung disease. The groups did not differ in alcohol consumption, but smoking was less common and regular physical activity more common among individuals with higher PA.
Table 1.
EMA PA and risk factors
| Factor | High PA (n = 1,399) (%) | Medium PA (n = 1,530) (%) | Low PA (n = 924) (%) | P value (trend) |
| Age at baseline (y) | 64.33 ± 7.13 | 64.07 ± 7.46 | 64.91 ± 7.66 | 0.024 |
| Sex (women) | 720 (51.5) | 868 (56.7) | 518 (56.1) | 0.015 |
| Marital status (married) | 1099 (78.6) | 1148 (75.0) | 653 (70.7) | 0.001 |
| Ethnicity (white) | 1384 (98.9) | 1514 (99.0) | 913 (98.8) | 0.83 |
| Employment status (used) | 450 (32.2) | 518 (33.9) | 280 (30.3) | 0.47 |
| Education | ||||
| Lower | 425 (30.4) | 439 (28.7) | 289 (31.3) | 0.32 |
| Intermediate | 565 (40.4) | 613 (40.1) | 395 (42.7) | |
| Higher | 240 (29.2) | 477 (31.2) | 240 (26.0) | |
| Wealth quintile | ||||
| 1 (Lowest) | 272 (19.5) | 300 (19.6) | 197 (21.3) | 0.07 |
| 2 | 270 (19.3) | 307 (20.1) | 194 (21.0) | |
| 3 | 295 (21.1) | 289 (18.9) | 192 (20.8) | |
| 4 | 285 (20.4) | 288 (18.8) | 193 (20.9) | |
| 5 (Highest) | 276 (19.7) | 344 (22.5) | 148 (16.0) | |
| Negative affect | 3.28 ± 0.69 | 3.41 ± 0.77 | 3.86 ± 1.28 | 0.001 |
| Depression (above threshold) | 61 (4.4) | 147 (9.6) | 208 (22.5) | 0.001 |
| Diagnosed depressive in the past 2 y | 7 (0.5) | 26 (1.7) | 17 (1.8) | 0.003 |
| Fair or poor self-rated health | 204 (14.6) | 306 (20.0) | 270 (29.2) | 0.001 |
| Serious illness at baseline | ||||
| Cancer | 104 (7.4) | 114 (7.5) | 76 (8.2) | 0.51 |
| CHD | 39 (2.8) | 39 (2.5) | 28 (3.0) | 0.79 |
| Stroke | 16 (1.1) | 33 (2.2) | 16 (1.7) | 0.19 |
| Diabetes | 96 (6.9) | 108 (7.1) | 60 (6.5) | 0.77 |
| Heart failure | 3 (0.2) | 1 (0.1) | 2 (0.2) | 0.89 |
| Chronic lung disease | 51 (3.6) | 54 (3.5) | 45 (4.9) | 0.18 |
| Current smoker | 132 (9.4) | 170 (11.1) | 121 (13.1) | 0.006 |
| Vigorous or moderate physical activity ≥1×/wk | 1,214 (86.8) | 1,294 (84.6) | 750 (81.2) | 0.001 |
| Alcohol at least daily | 423 (30.3) | 499 (32.7) | 258 (28.0) | 0.38 |
On average, participants made their first EMA rating on waking in the morning at 7:01 AM ± 67 min (SD), and the second rating at 7:40 AM ± 63 min. These times did not vary among PA groups. Across the population as a whole, PA was lowest on waking and highest at 7:00 PM. The pattern of changes was slightly different across PA groups (P < 0.001), with larger increases across the day in the high and low compared with medium PA groups. There were no interactions between PA group and sex.
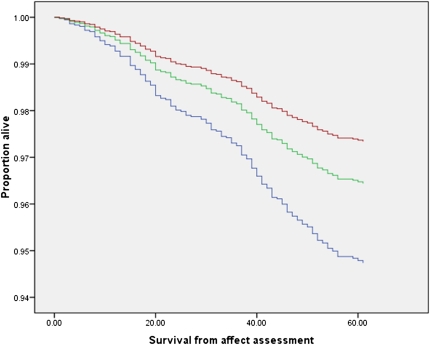
In the high-PA group, 3.6% of subjects (50 of 1,399) died, compared with 4.6% (70 of 1,530) of the medium-PA and 7.3% (67 of 924) of the low-PA group. Compared with the low-PA group, the age- and sex-adjusted hazard ratios (HRs) for high- and medium-PA participants were 0.498 [95% confidence interval (CI), 0.345–0.721] and 0.671 (95% CI, 0.478–0.940; Table 2), respectively, indicating a graded relationship with mortality. Survival curves for the three PA groups are illustrated in Fig. 1. The 50% reduction in risk of death in the high- compared with low-PA group was moderately attenuated when demographic factors, negative affect indicators, health status, and health behaviors were taken into account statistically (Table 2, models 2–5); the HR was 0.646 (95% CI, 0.436–0.958) in the high-affect group in the model adjusted for all these factors, and the HR was 0.800 (95% CI, 0.560–1.142) in the medium-PA group. Other independent predictors of death in the full model were older age, male sex, fair or poor self-rated health, diagnoses of cancer, stroke, and chronic lung disease at baseline, smoking, and lower physical activity levels (Table S1 shows the complete regression model). In addition to the proportional-hazards regression based on tertiles of PA, logistic regression was carried out using the full range of PA scores. The odds ratio was significant (0.842; 95% CI, 0.732–0.969; P = 0.016) in the full model including all covariates, indicating that each unit increase in PA was associated with a reduction in the odds of survival.
Table 2.
PA and mortality: Complete sample
| Model | Covariates | PA level | PA-adjusted HR (95% CI) | P value |
| 1 | Age, sex | Low | 1 | |
| Medium | 0.671 (0.478–0.940) | 0.020 | ||
| High | 0.498 (0.345–0.721) | 0.001 | ||
| 2 | Age, sex + demographic factors* | Low | 1 | |
| Medium | 0.689 (0.490–0.967) | 0.031 | ||
| High | 0.514 (0.355–0.744) | 0.001 | ||
| 3 | Age, sex + demographic factors* + negative affect indicators† | Low | 1 | |
| Medium | 0.728 (0.513–1.033) | 0.076 | ||
| High | 0.559 (0.379–0.824) | 0.003 | ||
| 4 | Age, sex + demographic factors* + negative affect indicators† + health indicators‡ | Low | 1 | |
| Medium | 0.794 (0.556–1.132) | 0.202 | ||
| High | 0.633 (0.427–0.938) | 0.023 | ||
| 5 | Age, sex + demographic factors* + negative affect indicators† + health indicators‡ + health behaviors§ | Low | 1 | |
| Medium | 0.800 (0.560–1.142) | 0.22 | ||
| High | 0.646 (0.436–0.958) | 0.030 |
Reference group is low PA; 67 of 924 deaths in low, 70 of 1,530 in medium-PA and 50 of 1,399 in high-PA groups.
*Demographic factors: wealth, education, marital status, and employment status.
†Negative affect indicators: negative affect, elevated CES-D score, and depressive illness in the past 2 y.
‡Health indicators: self-rated health, cancer, CHD, stroke, diabetes, heart failure, and chronic lung disease.
§Health behaviors: smoking, physical activity, and alcohol intake.
Fig. 1.
Proportion of individuals in the high-PA (red), medium-PA (green) and low-PA (blue groups) surviving over the follow-up period (indicated in months from baseline). Values are adjusted for age and sex.
Similar Cox regression analyses were carried out for negative affective states, dividing the population into tertiles of EMA negative affect, and comparing individuals with and without significant depressive symptoms. No associations were observed for EMA distressed affect, but depressive symptoms were related to increased mortality (Table 3). The HR for elevated depressive symptoms was 1.680 (95% CI, 1.061–2.370) after adjustment for age, sex, and demographic factors, but decreased to 1.036 (95% CI, 0.720–1.492) after health indicators were included in the model. These analyses indicate that, unlike PA, the association between depressive symptoms and survival was strongly dependent on participants’ baseline state of health.
Table 3.
Symptoms of depression and mortality: Complete sample
| Model | Covariates | Depression level | Depression-adjusted HR (95% CI) | P value |
| 1 | Age, sex | Low | 1 | |
| High | 1.760 (1.254–2.469) | 0.001 | ||
| 2 | Age, sex + demographic factors* | Low | 1 | |
| High | 1.680 (1.061–2.370) | 0.003 | ||
| 3 | Age, sex + demographic factors* + health indicators† | Low | 1 | |
| High | 1.036 (0.720–1.492) | 0.84 | ||
| 4 | Age, sex + demographic factors* + health indicators† + health behaviors‡ | Low | 1 | |
| High | 1.004 (0.696–1.448) | 0.98 |
Reference group is low depression symptoms (≤ 2): 141 of 3,196 deaths in low depression group, 46 of 657 in high depression group.
*Demographic factors: wealth, education, marital status, and employment status.
†Health indicators: self-rated health, cancer, CHD, stroke, diabetes, heart failure, and chronic lung disease.
‡Health behaviors: smoking, physical activity, and alcohol intake.
We also sought to discover whether the prediction of mortality varied for momentary PA ratings obtained at different times of day. After adjustment for age, sex, demographic factors, negative affect indicators, and health, the association of high PA with lower mortality rate was comparable for ratings taken at different times of day: waking (HR, 0.680; 95% CI, 0.458–1.009), 30 min after waking (HR, 0.708; 95% CI, 0.464–1.080), 7:00 PM (HR, 0.663; 95% CI, 0.456–0.964), and at bedtime (HR, 0.554; 95% CI, 0.366–0.840).
A further set of analyses was carried out with data from individuals who died within 6 mo of the EMA assessment excluded to ensure that effects were not caused by preexisting terminal illness. The proportions of deaths were 3.5% in the high-PA group, 4.1% in the medium-PA group, and 7.0% in the low-PA group. The regression results are summarized in Table S2, and illustrate a very similar pattern to that found in the complete sample, albeit with wider CIs as a result of the smaller number of cases. The age- and sex-adjusted HR of 0.513 (95% CI, 0.354–0.744) in the high-PA group was attenuated to 0.652 (95% CI, 0.439–0.970) after adjustment for demographic factors, negative affect, health indicators, and health behaviors.
Discussion
The analyses described here indicate that the intensity of positive mood states assessed over a single day predicts mortality over the following 5 y in a graded fashion, with high PA being associated with substantially longer survival. The 50% reduction in mortality risk in the high-PA group was reduced to 35% when sociodemographic factors, initial health, indicators of depression, and major health behaviors were taken into account. Trends were very similar when deaths over the first 6 mo were excluded from the analyses, indicating that effects are unlikely to be caused by seriously ill people experiencing low PA before death. By contrast, negative affective states were not associated with greater mortality after covariates had been taken into account.
EMA and other measures of current affect are increasingly being used to investigate variations in positive well-being with age (21), relationships with wealth (20), and psychopathology (22). The association with mortality corroborates findings that have used retrospective questionnaires to measure affect (3). One previous study found that positive emotional experience measured several times a day over 7 d predicted reduced mortality over a 13-y period (23). However, the study was smaller in scale (N = 111) and involved a sample deliberately selected for good health, and the analyses did not take into account socioeconomic status (SES) or preexisting health problems. Interestingly, momentary affect in the present study was relatively independent of sociodemographic factors and preexisting diagnosed illness. As shown in Table 1, there was no association between PA and education and employment, or with the presence of cancer, CHD, stroke, diabetes, heart failure, or chronic lung disease at baseline. This compares with retrospective questionnaire measures of positive moods, which are more consistently associated with lower SES and the presence of serious illness (24, 25).
Although controlling for the presence of diagnosed illnesses at baseline reduces the likelihood of effects being secondary to initial health status, it only partly rules out reverse causality. The reason is that undiagnosed or subclinical health problems and symptoms may impair positive well-being and contribute to mortality risk. We therefore included self-rated health as an additional covariate. Self-rated health has an established association with mortality (26), and is an integrated indicator of subjective physical and mental symptoms and health appraisals (27). However, in this sample, these factors accounted for only approximately 30% of the protective effect of PA. Other recent studies of mortality that used retrospective measures of well-being have demonstrated greater attenuation of effects when sociodemographic factors, health, and health behavior are taken into account (6, 9, 28).
One reason why EMA measures may be more independently associated with health outcomes is that they provide more accurate indications of affective state. Neurobiological studies indicate that positive emotional states are linked with activity in the limbic system, including activation of central striatal dopaminergic systems (29). These same regions of the central nervous system control biological processes such as autonomic regulation, neuroendocrine activation, and inflammatory responses (30). It is notable that associations between PA and reduced cortisol output over the course of the day, as well as cardiovascular and cortisol responses to stress, have been more consistent when assessments have involved EMA or measures of affect over the day than with retrospective measures of positive well-being (31).
An important issue in studies of positive well-being and health is the role of depression and other negative affective states (32, 33). Depressed mood is known to be associated with CHD (34), cancer (35), diabetes (36), and other conditions. However, in the present analyses, the protective effect of PA remained after controlling for depression and EMA negative affect. Additionally, neither negative affect nor depressive symptoms were independent predictors of mortality after health indicators had been taken into account. This suggests that, in this older general population cohort, the absence of PA may be more important to health outcomes than the presence of negative affective states.
The present study has several limitations. EMA was carried out by only a subset of participants in ELSA; men and women who were in frail condition or aged 80 y or older were not asked to take part. The analyses were based on total mortality, and further research is required to explore associations with specific causes of death such as cardiovascular disease and cancer. The number of health behaviors included in the models was limited, and measures of food intake and body mass were not available. EMA was carried out over a single day, and only four sets of ratings were completed. The assessments were taken using pencil-and-paper diaries, so they lack the temporal precision of electronic techniques (18). This protocol was constrained by the times needed for the assessment of cortisol, and measures at more times of day would have been desirable for measuring the profile of mood change with greater precision.
These results do not establish that effects are causal. Momentary PA may be a marker of underlying biological processes, or unmeasured behavioral or temperamental factors that are responsible for the survival effects. Nevertheless, the present study lends weight to the value of assessing experienced affect, by indicating robust and graded associations with future mortality. The present findings provide further reason to target the positive well-being of older people. In addition to addressing the health status and material circumstances of older people, efforts to improve affective states may have beneficial health consequences.
Materials and Methods
Participants.
The present data were collected as part of the ELSA, a longitudinal panel study of noninstitutionalized men and women aged 50 y or older living in England in 2002 (37). The core ELSA sample was drawn from households participating in the Health Survey for England over the years 1998, 1999, and 2001 (19,924 eligible individuals), of whom 2,605 had died before 2002. The baseline core sample consisted of 11,391 individuals. Comparison of the sociodemographic characteristics of participants against results from the national census showed that the sample was representative of the English population.
The data analyzed here collected in wave two of ELSA (2004), when the response rate was 81.5% (38). A subset of participants aged less than 80 y was asked to take four saliva samples at home over a single day for the assessment of cortisol, and to complete a logbook at the same time. The cortisol data are not currently available, but the EMA data are derived from the logbooks. The number of individuals who provided saliva samples was 4,732, of whom 3,853 (83%) completed the EMA assessments, consented to mortality follow-up, and provided data on wealth, longstanding illness, and other relevant variables. Individuals who completed EMA were younger on average (mean, 64.30 ± 7.40 y vs. 68.21 ± 7.23 y; t-statistic = 10.92; P < 0.001) and more likely to be married (74.2% vs. 54.9%; χ2 = 73.13; P < 0.001), in paid employment (32.0% vs. 15.4%; χ2 = 62.60; P < 0.001), and wealthier (χ2 = 82.05; P < 0.001) than those who failed to complete the logbooks.
EMAs of Affect.
Affect measures were obtained at four time points over the course of the day: on waking, 30 min after waking, at 7:00 PM, and at bedtime. At each time, participants were asked to rate the extent to which they felt happy, excited, content, worried, anxious, and fearful on four-point scales ranging from 1, indicating “not at all,” to 4, indicating “extremely.” PA was computed by summing the three positive states (happy, excited, and content), and negative affect by summing worried, anxious, and fearful states. The internal consistency for positive and negative affect measures was good (Cronbach α-values of 0.90 and 0.92, respectively). It should be noted that the moods incorporated into the negative affect measure centered on anxiety and worry, rather than on other aspects of negative affect such as sadness or anger (39), so we also included a measure of depressive symptoms in the analyses. Ratings for the four time points were averaged to generate aggregate EMA positive and distressed affect measures, ranging from three to 12, with higher scores indicating greater affect.
Mortality.
Mortality data were obtained through linkage with the National Health Service Central Data Registry from completion of wave-two assessments (2004/2005) until October 2009. The mean follow-up period was 60.6 ± 2.7 mo.
Other Measures.
Information was available about age, sex, ethnicity, paid employment, and marital status. SES was indexed by total wealth, net of debt, including the value of any home and other property (less mortgage), financial assets covering all types of savings available in England, and the value of any business assets and physical wealth such as artwork and jewelry. Wealth is the most robust indicator of socioeconomic circumstances in ELSA (37). Quintiles of wealth were computed separately for participants younger than age 65 y and 65 y or older. Depression was measured using the eight-item Center for Epidemiologic Studies Depression Scale (CES-D). Participants reporting three or more symptoms were classified as having significant symptoms of depression. This scale has been found to have acceptable internal reliability (α = 0.90 in this sample) and validity (40). Participants were also categorized on whether they had been diagnosed with a depressive illness in the previous 2 y.
Health was assessed with two sets of measures. First, information was collected about diagnoses of cancer, CHD, stroke, diabetes, heart failure, and chronic lung disease. Second, self-rated health was used as an indicator of subclinical or undiagnosed health problems (27). Participants were categorized into those who rated their health as excellent, very good, or good in comparison with fair or poor. Current smoking, participation in vigorous or moderate activity at least once per week, and drinking alcohol at least daily were also assessed.
Procedure.
Wave two of ELSA involved a computer-assisted personal interview, a self-completed questionnaire, and a nurse visit to each participant's home. At the nurse visit, the saliva sampling procedure and logbook were explained to participants, and they were instructed to return the samples and logbooks in a prepaid envelope. Participants were asked to carry out the assessments on a weekday. The saliva samples have not yet been analyzed.
Statistical Analysis.
Participants were divided into low-, medium-, and high-PA groups of aggregate EMA. Grouping was based on tertiles, but group sizes differed because of ties in ratings. Comparisons between groups on covariates were carried out by using χ2 analysis for categorical data and ANOVA for continuous variables. Patterns of PA over the course of the day were analyzed by using repeated-measures ANOVA with sex and PA group as between-person factors and time of day as the within-person factor. Cox proportional-hazards regression models were used to estimate HRs of death and 95% CIs associated with higher PA. In the full sample, five models were tested. Model 1 was adjusted for age and sex. Demographic factors (wealth, education, marital status, and employment status) were added in model 2; ethnicity was excluded from this model because the proportion of ethnic minority participants was very small. Indicators of negative affect (EMA negative affect, CES-D scores, and diagnosis of depression) were added in model 3 to discover whether associations between PA and mortality were independent of negative mood states. Model 4 added health indicators (limiting longstanding illness, cancer, CHD, stroke, diabetes, and chronic lung disease at baseline), and health behaviors (smoking, physical activity, alcohol intake) were included in model 5. In addition, further analyses were carried out on participants who survived for at least 6 mo. To determine whether associations between EMA PA and survival were present across the complete distribution of affect scores, logistic regression on mortality involving mean PA ratings was also carried out. Cox regression analysis was also carried out comparing tertiles of negative affect, and participants with and without elevated depressive symptoms. Analyses were carried out using SPSS version 18 and STATA version 8 programs.
Supplementary Material
Acknowledgments
The English Longitudinal Study of Ageing was developed by a team of researchers based at University College London, the Institute of Fiscal Studies, and the National Centre for Social Research. The data are lodged with the UK Data Archive. Funding was provided by National Institute on Aging Grants 2R01AG7644-01A1 and 2R01AG017644 and a consortium of UK government departments coordinated by the Office for National Statistics. A.S. is funded by the British Heart Foundation. J.W. is funded by Cancer Research UK.
Footnotes
The authors declare no conflict of interest.
This article is a PNAS Direct Submission.
This article contains supporting information online at www.pnas.org/lookup/suppl/doi:10.1073/pnas.1110892108/-/DCSupplemental.
References
- 1.Stiglitz J. Report by the Commission on the Measurement of Economic Performance and Social Progress. 2009. Available at http://www.stiglitz-sen-fitoussi.fr/documents/rapport_anglais.pdf. Accessed July 5, 2011.
- 2.Waldron S. Measuring Subjective Wellbeing in the UK. Newport, UK: Office for National Statistics; 2010. [Google Scholar]
- 3.Chida Y, Steptoe A. Positive psychological well-being and mortality: a quantitative review of prospective observational studies. Psychosom Med. 2008;70:741–756. doi: 10.1097/PSY.0b013e31818105ba. [DOI] [PubMed] [Google Scholar]
- 4.Boehm JK, Peterson C, Kivimaki M, Kubzansky L. A prospective study of positive psychological well-being and coronary heart disease. Health Psychol. 2011;30:259–267. doi: 10.1037/a0023124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Xu J, Roberts RE. The power of positive emotions: It's a matter of life or death—subjective well-being and longevity over 28 years in a general population. Health Psychol. 2010;29:9–19. doi: 10.1037/a0016767. [DOI] [PubMed] [Google Scholar]
- 6.Koopmans TA, Geleijnse JM, Zitman FG, Giltay EJ. Effects of happiness on all-cause mortality during 15 years of follow-up: The Arnhem Elderly Study. J Happiness Stud. 2010;11:113–124. [Google Scholar]
- 7.Davidson KW, Mostofsky E, Whang W. Don't worry, be happy: Positive affect and reduced 10-year incident coronary heart disease: The Canadian Nova Scotia Health Survey. Eur Heart J. 2010;31:1065–1070. doi: 10.1093/eurheartj/ehp603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kubzansky LD, Thurston RC. Emotional vitality and incident coronary heart disease: Benefits of healthy psychological functioning. Arch Gen Psychiatry. 2007;64:1393–1401. doi: 10.1001/archpsyc.64.12.1393. [DOI] [PubMed] [Google Scholar]
- 9.Shirai K, et al. Japan Public Health Center-Based Study Group. Perceived level of life enjoyment and risks of cardiovascular disease incidence and mortality: The Japan public health center-based study. Circulation. 2009;120:956–963. doi: 10.1161/CIRCULATIONAHA.108.834176. [DOI] [PubMed] [Google Scholar]
- 10.Penninx BW, et al. The protective effect of emotional vitality on adverse health outcomes in disabled older women. J Am Geriatr Soc. 2000;48:1359–1366. doi: 10.1111/j.1532-5415.2000.tb02622.x. [DOI] [PubMed] [Google Scholar]
- 11.Koivumaa-Honkanen H, et al. Self-reported life satisfaction and 20-year mortality in healthy Finnish adults. Am J Epidemiol. 2000;152:983–991. doi: 10.1093/aje/152.10.983. [DOI] [PubMed] [Google Scholar]
- 12.Brummett BH, et al. Ratings of positive and depressive emotion as predictors of mortality in coronary patients. Int J Cardiol. 2005;100:213–216. doi: 10.1016/j.ijcard.2004.06.016. [DOI] [PubMed] [Google Scholar]
- 13.Blazer DG, Hybels CF. What symptoms of depression predict mortality in community-dwelling elders? J Am Geriatr Soc. 2004;52:2052–2056. doi: 10.1111/j.1532-5415.2004.52564.x. [DOI] [PubMed] [Google Scholar]
- 14.Ostir GV, Markides KS, Peek MK, Goodwin JS. The association between emotional well-being and the incidence of stroke in older adults. Psychosom Med. 2001;63:210–215. doi: 10.1097/00006842-200103000-00003. [DOI] [PubMed] [Google Scholar]
- 15.Kahneman D, Krueger AB, Schkade D, Schwarz N, Stone AA. Would you be happier if you were richer? A focusing illusion. Science. 2006;312:1908–1910. doi: 10.1126/science.1129688. [DOI] [PubMed] [Google Scholar]
- 16.Miron-Shatz T, Stone A, Kahneman D. Memories of yesterday's emotions: Does the valence of experience affect the memory-experience gap? Emotion. 2009;9:885–891. doi: 10.1037/a0017823. [DOI] [PubMed] [Google Scholar]
- 17.Kahneman D, Riis J. Living, and thinking about it: Two perspectives on life. In: Huppert FA, Baylis N, Keverne EB, editors. The Science of Well-Being. Oxford: Oxford Univ Press; 2005. pp. 285–305. [Google Scholar]
- 18.Shiffman S, Stone AA, Hufford MR. Ecological momentary assessment. Annu Rev Clin Psychol. 2008;4:1–32. doi: 10.1146/annurev.clinpsy.3.022806.091415. [DOI] [PubMed] [Google Scholar]
- 19.Kahneman D, Krueger AB, Schkade DA, Schwarz N, Stone AA. A survey method for characterizing daily life experience: The day reconstruction method. Science. 2004;306:1776–1780. doi: 10.1126/science.1103572. [DOI] [PubMed] [Google Scholar]
- 20.Kahneman D, Deaton A. High income improves evaluation of life but not emotional well-being. Proc Natl Acad Sci USA. 2010;107:16489–16493. doi: 10.1073/pnas.1011492107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Stone AA, Schwartz JE, Broderick JE, Deaton A. A snapshot of the age distribution of psychological well-being in the United States. Proc Natl Acad Sci USA. 2010;107:9985–9990. doi: 10.1073/pnas.1003744107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Myin-Germeys I, et al. Experience sampling research in psychopathology: opening the black box of daily life. Psychol Med. 2009;39:1533–1547. doi: 10.1017/S0033291708004947. [DOI] [PubMed] [Google Scholar]
- 23.Carstensen LL, et al. Emotional experience improves with age: Evidence based on over 10 years of experience sampling. Psychol Aging. 2011;26:21–33. doi: 10.1037/a0021285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Steptoe A, O'Donnell K, Marmot M, Wardle J. Positive affect and psychosocial processes related to health. Br J Psychol. 2008;99:211–227. doi: 10.1111/j.2044-8295.2008.tb00474.x. [DOI] [PubMed] [Google Scholar]
- 25.Wikman A, Wardle J, Steptoe A. Quality of life and affective well-being in middle-aged and older people with chronic medical illnesses: A cross-sectional population based study. PLoS ONE. 2011;6:e18952. doi: 10.1371/journal.pone.0018952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Idler EL, Benyamini Y. Self-rated health and mortality: A review of twenty-seven community studies. J Health Soc Behav. 1997;38:21–37. [PubMed] [Google Scholar]
- 27.Jylhä M. What is self-rated health and why does it predict mortality? Towards a unified conceptual model. Soc Sci Med. 2009;69:307–316. doi: 10.1016/j.socscimed.2009.05.013. [DOI] [PubMed] [Google Scholar]
- 28.Steptoe A, Wardle J. Enjoying life and living longer: A prospective analysis from the English Longitudinal Study of Ageing. Arch Intern Med. doi: 10.1001/archinternmed.2011.1028. in press. [DOI] [PubMed] [Google Scholar]
- 29.Burgdorf J, Panksepp J. The neurobiology of positive emotions. Neurosci Biobehav Rev. 2006;30:173–187. doi: 10.1016/j.neubiorev.2005.06.001. [DOI] [PubMed] [Google Scholar]
- 30.Critchley HD. Neural mechanisms of autonomic, affective, and cognitive integration. J Comp Neurol. 2005;493:154–166. doi: 10.1002/cne.20749. [DOI] [PubMed] [Google Scholar]
- 31.Steptoe A, Gibson EL, Hamer M, Wardle J. Neuroendocrine and cardiovascular correlates of positive affect measured by ecological momentary assessment and by questionnaire. Psychoneuroendocrinology. 2007;32:56–64. doi: 10.1016/j.psyneuen.2006.10.001. [DOI] [PubMed] [Google Scholar]
- 32.Bostock S, Hamer M, Wawrzyniak AJ, Mitchell ES, Steptoe A. Positive emotional style and subjective, cardiovascular and cortisol responses to acute laboratory stress. Psychoneuroendocrinology. 2011;36:1175–1183. doi: 10.1016/j.psyneuen.2011.02.009. [DOI] [PubMed] [Google Scholar]
- 33.Sloan RP. Virtue and vice in health and illness: The idea that wouldn't die. Lancet. 2011;377:896–897. doi: 10.1016/s0140-6736(11)60339-5. [DOI] [PubMed] [Google Scholar]
- 34.Nicholson A, Kuper H, Hemingway H. Depression as an aetiologic and prognostic factor in coronary heart disease: A meta-analysis of 6362 events among 146 538 participants in 54 observational studies. Eur Heart J. 2006;27:2763–2774. doi: 10.1093/eurheartj/ehl338. [DOI] [PubMed] [Google Scholar]
- 35.Pinquart M, Duberstein PR. Depression and cancer mortality: A meta-analysis. Psychol Med. 2010;40:1797–1810. doi: 10.1017/S0033291709992285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Moussavi S, et al. Depression, chronic diseases, and decrements in health: Results from the World Health Surveys. Lancet. 2007;370:851–858. doi: 10.1016/S0140-6736(07)61415-9. [DOI] [PubMed] [Google Scholar]
- 37.Marmot M, Banks J, Blundell R, Lessof C, Nazroo J, editors. Health, Wealth and Lifestyles of the Older Population in England. London: Institute for Fiscal Studies; 2003. [Google Scholar]
- 38.Banks J, Breeze E, Lessof C, Nazroo J. Retirement, Health and Relationships of the Older Population in England: the 2004 English Longitudinal Study of Ageing. London: Institute for Fiscal Studies; 2006. [Google Scholar]
- 39.Steptoe A, Leigh ES, Kumari M. Positive affect and distressed affect over the day in older people. Psychol Aging. 2011 doi: 10.1037/a0023303. 10.1037/a0023303. [DOI] [PubMed] [Google Scholar]
- 40.Steffick DE. Documentation of Affective Functioning Measures in the Health and Retirement Study. Ann Arbor: Univ Michigan; 2000. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.