Abstract
Although a high degree of flexion is necessary for some activities of daily living, most total knee arthroplasty implants are designed to provide only up to 120° of flexion. Some new designs claim to provide greater flexion. In this retrospective study, we evaluated the Sigma rotating-platform high-flex knee against the traditional Sigma rotating-platform knee (DePuy, Warsaw, IN). There were 153 knees evaluated. We matched the subjects primarily on preoperative flexion and had 64 matched pairs. We also evaluated the knees based on their preoperative flexion, either <120° or ≥120°. In comparing the two implants, there were no significant differences in the patients' overall satisfaction, flexion gained or lost, or the need for further surgery. This study was approved by an institutional review board.
INTRODUCTION
Traditional knee replacements have been designed to provide painless range of motion from 0° to about 120° of flexion1. More recently, designs have been introduced to allow up to 155° of flexion, which is necessary and/or helpful for kneeling, squatting, and sitting cross-legged. The P.F.C. Sigma Rotating Platform High Flex (RP-F) is a high-performance posterior-stabilized knee based on the successful P.F.C. Sigma posterior-stabilized design (DePuy, Warsaw, IN). There are a number of differences between the Sigma Rotating Platform (RP) and the RP-F. The RP-F has a reduced sagittal radius of the posterior condyles2; a third articulating surface has been added behind the post-cam mechanism that is supposed to
reduce the high-contact stresses seen in the posterior condyles during deep flexion; the design requires resection of an additional two-to-four millimeters of bone from the posterior femoral condyles; on the tibial side, a pin device has been added to reinforce the post during deep flexion (Figure 1); and the tibial post-and-tray insert has beveled surfaces to reduce the risk of soft-tissue impingement and allow greater rotation of the implant, respectively.3 The RP-F knee does cost more than the RP knee; for the patients in this study, the difference in cost was $1,100.
Figure 1.
Radiographs of the two knee systems: The Sigma rotating-platform knee (right) and the Sigma rotating-platform high-flex knee (left) are seen in a patient who received one of each knee type (not simultaneously). This patient did not notice any difference between the two implants.
There have been two previous studies evaluating this knee system. In both studies, knees implanted with the RP-F device had significantly greater postoperative flexion than those with the RP knee.1,3 However, there were no significant differences in knee society scores, and one of the studies showed only a 1° difference in flexion between the two knee types.
In studies evaluating other brands of high-flex implants, conclusions regarding flexion were varied. Some studies found significant differences in flexion between the traditional and high-flex knees4,5 while others did not show a significant difference.6-10 Most of these studies also used standard follow-up forms to assess the performance of the knee designs. In all but one of these studies, there were no significant differences between the high-flex and standard knee systems.4-7,10 Nutton et al. found that patients with high-flex implants had a slight advantage when squatting and getting into a bathtub. However, they concluded that this difference was too small to be clinically relevant8 No study has specifically evaluated the effect of high-flexion knee designs on the patients' overall satisfaction with their knee replacement.
In the short term, the RP-F implant has been shown to be as safe as the RP knee, and it is supposed to provide lower levels of wear in deep flexion as compared to the traditional device.2 However, this claim has not been clinically evaluated.
The purpose of this study was to evaluate the performance of the Sigma RP knee versus the Sigma RP-F knee. As the high-flex knee is more expensive than the traditional implant, it is important to critically assess if its increased cost is justified by better performance. Our main research questions were:
Does knee-device type (high-flex vs regular) influence either the flexion measurements from pre-operative to post-operative, or overall patient satisfaction?
Does either the RP or RP-F knee have increased rates of complication leading to further surgery?
Based on the results of this study, is the higher cost of the RP-F implant justified?
MATERIALS AND METHODS
This was a retrospective, match-controlled study, with some of the data being collected prospectively. We conducted chart reviews on 163 total knee arthroplasties (TKAs) performed between December of 2006 and January of 2008. Inclusion criteria were a TKA performed by the senior author using Sigma rotating platform components. Patients were excluded if they did not have a recorded preoperative range of motion or if they received anything other than Sigma rotating platform components. During this period, 79 RP-F knees were implanted consecutively. The RP surgeries were performed immediately before and after the RP-F knees (43 before and 41 after). Seven subjects were lost to follow-up and three died from causes unrelated to their joint replacement, resulting in an analysis group of 153 subjects. The surgical procedure was similar in all cases, with a medial parapatellar arthrotomy, a tourniquet used
intraoperatively, and DePuy Endurance MV cement for all components. There were 90 females (59%) and 63 males (41%). Mean age at surgery was 64.0 years, mean weight was 99.9 kg, and mean preoperative flexion was 111.9°. All patients were diagnosed with osteoarthritis.
Subjects' postoperative active extension and flexion measurements were taken with a goniometer by clinic workers blinded to the type of implant received. These measurements were then compared to preoperative re-cords to determine net gain or loss in flexion. Follow-ups were at least nine months postoperatively (mean 16.7, range 9-33). Patients also answered a simple survey asking “How happy are you with your implanted knee?” with 1 equaling “completely dissatisfied” and 5 equaling “completely satisfied.” We monitored the patients' charts through 2010 (mean 42.8 months postoperatively, range 35.3-48.8), and any further surgery on the same knee was noted.
In order to minimize sample bias, RP-F knees were matched to RP controls. Sixty-four pairs of subjects were matched primarily on preoperative flexion, and secondarily on duration of follow-up, sex, age, and weight (see Table 1). In addition to this analysis, subjects were also divided into two groups based on preoperative flexion. Both previous studies of the RP-F knee found that it performed best in patients with <120° of preoperative Flexion1,3. Therefore, analysis was performed separately on all patients with preoperative flexion of <120° and those with ≥120°.
TABLE 1.
Demographic data for matched pairs
| Pre-op flexion | Follow-up (months) | Age (years) | Sex (f, m) | Weight (kg) | |
|---|---|---|---|---|---|
| RP | 113.1° | 16.9 | 64.8 | 62.5%, 37.5% | 99.6 |
| RP-F | 113.1° | 16.5 | 63.0 | 53%, 47% | 99.3 |
| P value* | 0.99 | 0.68 | 0.26 | 0.28 | 0.93 |
RP= Sigma Rotating Platform
RP-F= Sigma Rotating Platform High Flex
Two-tailed Student's t-test and chi square test (for sex)
We used independent Student's t-tests for continuous variables and chi square analysis for categorical data. Statistical significance was set at p<0.05.
We performed a power analysis to ensure adequate sample size. At a power of .95 with an alpha of 0.05, at least 53 subjects were needed in each group to see a difference of 10° in flexion gained or lost from preoperative to final measurements. This estimate was based on previous data from the same surgeon, hospital (s), and type of implant.
RESULTS
In the matched-pair analysis, there were no significant differences in gained flexion between the two study groups (p=0.47). Of all subjects whose preoperative flexion was <120°, there were 56 RP knees and 50 RP-F knees. There were no significant preoperative differences between the groups. However, the RP knees showed significantly more flexion gained than the RP-F knees (p=0.004). Of the subjects whose preoperative flexion was =120°, there were 22 RP knees and 25 RP-F knees. For these subjects, there were significantly more women in the RP-F group (60%) than in the RP group (40%; p=0.01). There were no other significant differences between the groups. The majority (77%) of patients in this group lost flexion, but there was no significant difference in the mean flexion lost (0=0.50, see Table 2 and Figure 2).
TABLE 2.
Results for all groups, with 95% confidence intervals
| Number | Gain in flexion | Satisfaction | ||
|---|---|---|---|---|
| Matched Pairs | RP | 64 | 3.1° (-0.3—6.5) | 4.4 (4.2—4.7) |
| RP-F | 64 | 1.6° (-1.3—4.4) | 4.5 (4.3—4.7) | |
| p value* | — | 0.47 | 0.82 | |
| Pre-op flexion <120° | RP | 56 | 11.4° (8.2—14.5) | 4.5 (4.3—4.7) |
| RP-F | 50 | 4.8° (1.7—7.9) | 4.3 (4.1—4.6) | |
| p value* | — | 0.004 | 0.26 | |
| Pre-op flexion ≥120° | RP | 22 | -8.3 (-12.6—4.1) | 4.5 (4.0—4.9) |
| RP-F | 25 | -6.6° (-9.5—3.7) | 4.6 (4.2-5.0) | |
| p value* | — | 0.50 | 0.57 | |
RP= Sigma Rotating Platform
RP-F= Sigma Rotating Platform High Flex
Two-tailed Student's t-test
Figure 2.
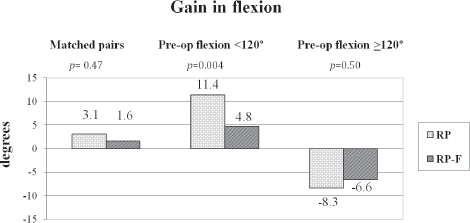
Gain in flexion from pre-operative measurement to follow-up (9-33 months postoperatively)
There were no significant differences in satisfaction scores between any of the analysis groups (see Table 2).
Of the 64 matched pairs, four of the RP-F patients later had additional surgery on the same knee. Three of these were arthroscopies for painful patellar clunk syndrome, and one was a revision because of a loose cement fragment. In the RP group, one patient had further surgery on the knee, an arthroscopy for painful patellar clunk. Although there were more surgeries in the RP-F group, this was not statistically significant (p= 0.17).
There were three patients who had non-simultaneous bilateral TKAs with one implant of each type. When asked if they felt a difference between their two implanted knees, they all said that they did not notice any difference.
DISCUSSION
Postoperative range of motion is an important out-come measure after TKA, as patients generally need a high degree of flexion if they want to engage in activities which include kneeling and squatting. Although there are many brands of high-flex knee implants which claim to improve flexion after TKA, past studies have shown mixed results as to whether or not the new designs actually increase flexion.1,3-10 With this study, we aimed to evaluate one of these high-flex designs by conducting a matched-pair study. The matched-pair study design is helpful in eliminating some of the extraneous variables that can cause bias. We matched subjects primarily on preoperative flexion, as this has been shown to be the primary factor affecting postoperative flexion.11
From their preoperative examination to the time of last follow-up, the matched RP and RP-F subjects both gained a small amount of flexion, 3.1° and 1.6° on average, respectively. It is interesting that the RP-F knee did not even provide a small increase in flexion over the RP knee, as was the case in a previous study.1
In one of the other studies comparing Sigma RP and RP-F knees, there were 50 matched pairs; results showed that the RP-F knee increased flexion by an average of 12° 3. The other Sigma flex knee study was a simultaneous, bilateral, randomized controlled trial of 93 subjects. They still found that the RP-F knee increased flexion, although this increase only averaged l°.1
In both of the previous studies conducted on the Sigma knees, results showed that the RP-F provided better results in patients whose preoperative flexion was less than 120°.1,3 However, we found the opposite to be true. For all patients whose preoperative flexion was less than 120°, the RP knee patients actually averaged 6.6° more flexion gained than the RP-F patients (p=0.004). For subjects whose preoperative flexion was greater than or equal to 120°, the majority of subjects (77%) lost flexion. The RP-F patients, on average, lost 1.7° less flexion than the RP knee patients; however, this result was not significant (p= 0.50).
Overall patient satisfaction did not seem to be affected by knee design, as the RP-F knee did not significantly increase or decrease satisfaction in any of the analysis groups.
It is also interesting to note that in the matched-pairs group, four RP-F subjects had further surgeries on their affected knee, while there was only one in the RP group; however, this result was also not statistically significant (p=0.17). Greater subject numbers and a study of longer term would be needed to investigate the relationship between the RP-F implant and its effect on the need for subsequent surgery on the knee.
The strengths of this study include data from a single surgeon and similar surgical practices, for each patient However, this data may be difficult to generalize to other surgical or hospital practices. Consecutive surgeries and matched-pair analysis served to minimize selection bias, although the study would have been stronger if a prospective, randomized selection process had been used.
It is recommended that the efficacy of high-flex knee devices be systematically evaluated prior to their routine use in TKA. In this study, we did not see any improvement in functional or qualitative outcomes for patients with the RP-F knee versus the RP knee. Therefore, in this population, the increased cost of the RP-F implant was not justified.
REFERENCES
- 1.Dennis D., et al. “Does Implant Design Affect Knee Flexion? A Simultaneous Bilateral TKA Randomized Controlled Trial”. Poster presentation at the Orthopaedic Research Society Annual Meeting; New Orleans, LA. 2010. [Google Scholar]
- 2.Ranawat A.S., Gupta S.K., Ranawat C.S. “The P.F.C. Sigma RP-F Total Knee Arthroplasty: Designed for Improved Performance”. Orthopedics. 2006;29(9):S28–S29. [PubMed] [Google Scholar]
- 3.Gupta S.K., et al. “The P.F.C. Sigma RP-F TKA Designed for Improved Performance: A Matched-pair Study”. Orthopaedics. 2006;29(9) Suppl:S49–S52. [PubMed] [Google Scholar]
- 4.Bin S.I., Nam T.S. “Early results of high-flex total knee Arthroplasty: comparison study at 1 year after surgery”. Knee Surg Sports Traumatol Arthrosc. 2007;15:350–355. doi: 10.1007/s00167-006-0202-y. [DOI] [PubMed] [Google Scholar]
- 5.Huang H., et al. “The Early Results of High-Flex Total Knee Arthroplasty: A Minimum of 2 Years of Follow-up”. J Arthroplasty. 2005;20(5):674–679. doi: 10.1016/j.arth.2004.09.053. [DOI] [PubMed] [Google Scholar]
- 6.Kim Y., et al. “Range of Motion of Standard and High-Flexion Posterior Stabilized Total Knee Prostheses: A Prospective, Randomized Study”. J Bone Joint Surg Am. 2005;87(7):1470–1475. doi: 10.2106/JBJS.D.02707. [DOI] [PubMed] [Google Scholar]
- 7.McCalden R.W., et al. “A RCT Comparing Hi-flex versus Standard Posterior Cruciate Substituting Polyethylene Tibial Inserts in TKR”. American Academy of Orthopaedic Surgeons Annual Meeting; Las Vegas, NV. 2009. [Google Scholar]
- 8.Nutton R.W., et al. “A prospective randomized double-blind study of functional outcome and range of flexion following total knee replacement with the NexGen standard and high flexion components”. J Bone Joint Surg Br. 2008;90(1):3742. doi: 10.1302/0301-620X.90B1.19702. [DOI] [PubMed] [Google Scholar]
- 9.Okamoto N., et al. “In Vivo Knee Kinematics in Patients With Bilateral Total Knee Arthroplasty of Two Designs”. Poster presentation at the Orthopaedic Research Society Annual Meeting; New Orleans, LA: 2010. [Google Scholar]
- 10.Seon J.K., et al. “Range of Motion in Total Knee Arthroplasty: A Prospective Comparison of High-Flexion and Standard Cruciate-Retaining Designs”. J Bone Joint Surg Am. 2009;91(3):672–679. doi: 10.2106/JBJS.H.00300. [DOI] [PubMed] [Google Scholar]
- 11.Ritter M.A., Campbell E.D. “Effect of Range of Motion on the Success of a Total Knee Arthroplasty”. J Arthroplasty. 1987;2(2):95–97. doi: 10.1016/s0883-5403(87)80015-3. [DOI] [PubMed] [Google Scholar]