Abstract
Background
Patellofemoral joint kinematics are dependent on a variety of anatomical features. One of the most common causes of patellar instability is malalignment of the quadriceps extensor mechanism. The Southwick-Fulkerson osteotomy focuses on correcting malalignment of the quadriceps extensor mechanism through medialization of the tibial tubercle. MRI, in conjunction with established patellofemoral indices, allows quantitative evaluation of the patellofemoral joint during active quadriceps extension both pre- and postoperatively.
Purpose
This study aims to quantitatively evaluate the effects of extensor mechanism medialization procedures using established patellofemoral indices in order to establish a relationship between tubercle transfer distance and patellar tracking. It is believed that a 15mm medial transfer of the tibial tubercle will produce statistically significant changes in patellar tracking when evaluated during active quadriceps contraction.
Methods
Four fresh-frozen cadavers underwent a modified Fulkerson osteotomy. The central quadriceps tendon was identified and traction was applied with a vector parallel to the femoral diaphysis using sutures, to simulate active quadriceps contraction. MRI images were obtained following Omm (control) and 15mm tibial tubercle medialization. Each knee was evaluated at 30, 20, 10, and 0 degrees of flexion. Results:
Quantitative evaluation of patellar tracking during active quadriceps contraction detected significant changes in patellar translation following 15mm medial transfer of the tibial tubercle as compared to the control. The significantly reduced indices suggest reduced patellar lateralization and improved patellar tracking during the critical range of motion from 30 to 0 degrees of flexion.
Conclusions
The results of this study indicate that significant quantitative changes in patellar tracking occur following 15mm tibial tubercle medialization when evaluated during active quadriceps contraction using MRI in conjunction with established patellofemoral indices. These findings suggest that quantitative evaluation of patellar tracking may be a valuable pre- and postoperative tool when coupled with qualitative clinical findings.
INTRODUCTION
Patellofemoral joint kinematics and patellar tracking describe the relationship between the patella and femur during flexion and extension of the knee. Patellofemoral joint kinematics are dependent on a variety of anatomical features including bony geometry, soft tissues, and the action of the quadriceps.1 While the healthy knee is unlikely to dislocate or undergo severe subluxation,2 any number of anatomical or physiological abnormalities could produce patellar instability. This is especially common in near-full knee extension as the patella moves proximally relative to the increasingly shallow trochlear groove while the tibia externally rotates, resulting in lateral patellar movement even in healthy subjects.1,3,4,5 It is at these lower degrees of flexion (0-30°) where soft tissue restraints and quadriceps muscle action exert the most important patellar stabilizing forces.6,7,8 Misalignment of the extensor mechanism does not allow the patella to properly track in the trochlear groove, producing lateral patellar instability.3,9,10
One of the most common causes of patellar instability is malalignment of the quadriceps extensor mechanism. 9, 10 Malalignment of the extensor mechanism has a wide spectrum of clinical presentations including an increased Q-angle, patellar subluxation as seen on the Merchant view, or more subtle presentations that do not appear until dynamic evaluation during the physical examination, such as a J-sign. A J-sign is defined as the lateral movement of the patella over the lateral femoral condyle during active leg extension. However, these clinical findings do not rule out other anatomic or physiologic factors that may cause patellar instability.11 In order to choose the appropriate surgical intervention, evaluation of the patellofemoral joint during active quadriceps contraction is essential.12 MR images obtained during active quadriceps contraction coupled with established patellofemoral indices (Figures 2 and 3) allow quantitative evaluation of the patellofemoral joint, which is essential for diagnosis of patellofemoral pathology and for postoperative outcome.3,13 This quantitative evaluation allows for assessment of the patellofemoral joint that may otherwise be difficult to obtain solely by clinical means.
Figure 2.
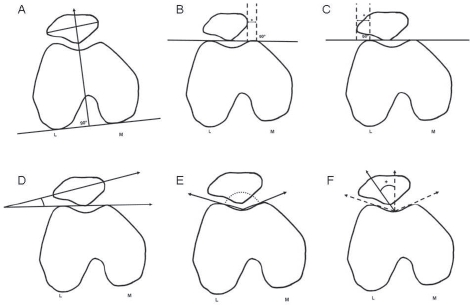
Established patellofemoral indices were measured using MR images of the knee at 30, 20, 10 and 0 degrees of flexion. A) Bisect offset (BSO) measures the percentage of total patellar width lateral to the deepest point of the sulcus. B) Lateral patellar displacement (LPD). Positive values are given when the patellar edge is medial to the perpendicular line created at the apex of the medial femoral condyle. C) Lateral patellar edge (LPE). Positive values are given when the lateral patellar edge lies lateral to the perpendicular line created at the apex of the lateral femoral condyle. D) Patellar tilt angle of Sasaki. E) Sulcus angle. F) Congruence angle. Values are positive when the line connectingthe sulcus to the most posterior aspect of the patella is lateral to thebisector of the sulcus angle.
Figure 3.

With the knee in full extension, axial slices containing the apex of the tibial tubercle and the deepest point of the trochlear groove were overlaid to measure the tibial tubercle-trochlear groove (TT-TG). The distance between the tibial tubercle and the depth of the groove was measured as the TT-TG. The measurement was parallel to the line tangential to the posterior femoral condyles.14
The modified Fulkerson osteotomy focuses on correcting malalignment of the quadriceps extensor mechanism through medialization of the tibial tubercle.12 This procedure is commonly used when the tibial tubercle-trochlear groove (TT-TG) distance exceeds 20mm.2,11,14 Rotational abnormalities, severe trochlear dysplasia, and patella alta must also be ruled out using preoperative imaging in order to verify that malalignment of the extensor mechanism is indeed the cause of patellofemoral pathology. Regardless of the medialization procedure performed in an attempt to correct patellar tracking, the degree to which the tibial tubercle is medialized relies on a great deal of clinical judgment intraoperatively.10 In order to reduce the reliance on static preoperative images and passive motion evaluation, intraoperative femoral nerve stimulation has been employed by this senior author to allow dynamic evaluation of the patellofemoral joint intraoperatively to ensure adequacy of the tibial tubercle transfer.10,12 However, in order to determine the efficacy of tibial tubercle transfer on improving patellar tracking, the relationship between tibial tubercle transfer distance and patellar tracking must be assessed.
This study aims to quantitatively evaluate the effects of medialization procedures using established patellofemoral indices to establish a relationship between tibial tubercle transfer distance and patellar tracking. Significant findings will allow a relationship to be determined between tibial tubercle transfer distance and patellar tracking, using several established patellofemoral indices. The alternative hypothesis for this study states that medial tibial tubercle transfer of 15mm, a minimum value in the senior author's(JPA) experience, will significantly affect patellofemoral kinematics.
MATERIALS AND METHODS
Specimens
Four fresh-frozen normal cadaver knees from a total of two donors were used in the study. The knees were both from female donors who were 69 and 76 years of age. The specimens were transected at mid-femur and mid-tibia.
Procedure
Following a 24-hr thawing period, each knee underwent a modified Southwick-Fulkerson osteotomy (as described previously) by the senior author (JPA).12 A single parapatellar incision spanned the length of the specimen in order to expose the distal attachment of the patellar tendon on the tibial tubercle. An oblique osteotomy of approximately 30 degrees in the axial plane was performed using an oscillating saw, and special care was taken to maintain a distal bony attachment (Figure 1A). Proximally, a dovetail cut made parallel to the joint line with an angle of 20-30 degrees in the sagittal plane was performed, 1cm above the insertion of the patellar tendon on the tibial tubercle (Figure 1B). To complete the procedure, the dovetail was then connected to the oblique osteotomy made previously. With the minimal load applied across the knee joint in this study, the dovetail and distal bony attachment provided sufficient support during simulated active quadriceps contraction and bicortical screws were not used. This also eliminated hardware artifact that might have interfered with quantitative measurements of the patellofemoral joint15. In the event that the distal bony bridge could not be maintained, a suture anchor was placed distally to replicate the bony attachment Each knee underwent a 15mm medial transfer of the tibial tubercle which was achieved by light tamping of the bony segment. The proximal ledge created by the dovetail along with the distal bone bridge provided adequate fixation to prevent shifting of the tubercle during dynamic assessment following medial transfer.
Figure 1.
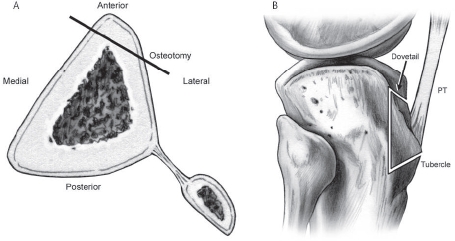
Axial (A) and sagittal (B) images depicting the modified Fulkerson osteotomy. The proximal dovetail and distal bone bridge allow for adequate fixation of the bony segment, making bicortical screws unnecessary and eliminating hardware artifact Adapted from Albright JP, Wilson AG. Modified Fulkerson Osteotomy. Techniques in Knee Surgery. 2006;5(1):39-46.
To simulate patellofemoral pathology in otherwise healthy cadaver specimens, the medial and lateral retinacula were dissected. In previous studies, this dissection resulted in an increased lateral patellar shift of up to 10mm6. The skin and subcutaneous tissue were removed from the thigh, and a running suture was placed through the central quadriceps tendon using Fiberwire 2.0. Traction was applied to the suture to create a force vector parallel to the femoral axis when viewed in the coronal plane, which best mimics the resultant vector of the combined muscle tensions acting on the quadriceps tendon as it inserts on the patella during concentric contraction.1
Imaging
Each knee was imaged prior to medial transfer of the tibial tubercle and again following 15mm medial transfer of the tibial tubercle. Knees were imaged at 30, 20, 10, and 0 degrees of flexion before and after medial transfer. This critical range of motion allowed investigation of patellofemoral kinematics as the patella moved proximally relative to the increasingly shallow trochlear groove.3,13 It is in this range where patellar instability is most often noted. Quadriceps contraction was simulated by applying traction to the running suture placed through the central quadriceps tendon, with enough force to maintain the leg in the degree of flexion desired. The vector of traction was parallel to the femoral diaphysis when viewed in the coronal plane. Knees were placed in a radiolucent apparatus that prevented femoral rotation during simulated contraction. The tibia was allowed to freely rotate during simulated quadriceps contraction, allowing for the natural external rotation as the leg approached full extension.
MRI Parameters
All images were acquired using a whole-body Siemens Tim Trio 3T with the knee positioned in the apparatus in the supine position. Images were acquired with a three-dimensional (3D) gradient-recalled echo (GRE) pulse sequence. Examination time was six minutes for each specimen in each evaluated degree of flexion.
The following imaging parameters were used to optimize time and contrast Flip angle 10 degrees, TE 1.6ms, TR 12.0ms, one excitation, field of view 14.0cm x 14.0cm x 14.4 cm, with a slice thickness of 1.0mm using continuous coverage (0mm inter-slice gap).
Measurement and Analysis
These established indices were used to quantitatively assess the patellofemoral joint at each set degree of flexion, including the bisect offset (BSO),8 lateral patellar displacement (LPD),16 lateral patellar edge (LPE),17 patellar tilt angle of Sasaki (PTA-S),18 sulcus angle,19 congruence angle (CA),19 and tibial tubercle-trochlear groove distance(TT-TG).14 Descriptions of each index are listed below.
Bisect offset (BSO)8, Figure 2A As described by Stanford et al., a line is drawn tangential to the medial and lateral posterior femoral condyles. A perpendicular line is then drawn through the deepest point of the sulcus. BSO is the ratio of the patella lateral to the perpendicular line compared to the total width of the patella.
Lateral patellar displacement (LPD)16, Figure 2B: Following the guidelines of Laurin et al., a line is drawn tangential to the medial and lateral anterior condyles. A perpendicular line is drawn through the apex of the medial condyle. The distance from this line to the most medial part of the patella is measured.
Lateral patellar edge (LPE)17, Figure 2C: First described by Brossman et al. as the distance ‘d', this measurement is identical to LPD except the apex of the lateral condyle is used.
Patellar tilt angle of Sasaki (PTA-S)18, Figure 2D: This is defined as the angle between the line that passes through the widest part of the patella and a line tangential to the anterior femoral condyles. The patellar tilt angle of Sasaki (PTA-S) was chosen over other patellar tilt indices because it has been shown to be effective in measuring patellar tilt independent of femoral rotation.15
Sulcus angle19, Figure 2E: As described by Merchant et al., this is the angle between the sulcus and the medial and lateral condyles.
Congruence angle19, Figure 2F: As described by Merchant et al., this is the angle created by the bisector of the sulcus angle and a line from the deepest point of the sulcus to the most posterior aspect of the patella.
TT-TG14, Figure 3: Using the guidelines established by Dejour et al., the horizontal distance between the tibial tubercle and trochlear groove was measured using axial MRI overlay.
Measurements were made by a single investigator (KD). Four knees were used to calculate mean and associated standard deviation at each chosen degree of flexion for both the control (Omm transfer) and 15mm transfer. The resulting values allowed the mean change in each patellofemoral index to be calculated to evaluate the change in patellofemoral kinematics following medial transfer. A one-tail Student's paired t-test was then used to determine the significance of the 15mm medial transfer on patellar tracking. A p-value of less than 0.05 was considered significant
RESULTS
The patellofemoral joint was evaluated using measurements listed above to compare patellar tracking following 15mm medial tibial tubercle transfer. Patterns of patellar tracking were consistent across all four knee specimens used in this study, and means were used in order to determine the significance of the 15mm transfer on patellofemoral kinematics as compared to the control (Omm transfer).
Medial transfer of the tibial tubercle produced a reduced bisect offset (BSO) value at all degrees of flexion except 30 degrees. This reduction was statistically significant with a p-value of 0.03 at 0 degrees of flexion, as BSO was reduced 0.055 ± 0.104 percent following 15mm transfer (Table 1). The reduced BSO values following medial transfer (from 20 to 0 degrees of flexion) indicate that the patella was medialized as the percentage of patella lying lateral to the sulcus was reduced.
TABLE 1.
Comparison of Patellofemoral Indices in Control Specimens (0mm) and 15mm Medial Transfer
| 30 Degrees Flexion | ||||
|---|---|---|---|---|
| Index | Control | 15mm | Change | P-value |
| BSO | 0.51 ± 0.06 | 0.54 ± 0.05 | 0.03 ± 0.08 | 0.029* |
| LPD | Q0.18 ± 2.3 | 03.8 ±2.2 | 3.7 ± 3.2 | 0.045* |
| LPE | 2.5 ± 1.9 | 00.23 ± 0.99 | 2.7 ± 2.2 | 0.031* |
| PTA-S | 14.4 ± 4.2 | 12.3 ± 2.85 | 2.1 ± 5.1 | 0.12 |
| Sulcus | 130 ± 7.3 | 127 ± 4.0 | 4.1 ± 8.2 | 0.15 |
| Congruence | Q8.2 ± 11.9 | 012.8 ±2.9 | 4.7 ± 14.9 | 0.13 |
| TT-TG | 8.3 ± 2.8 | 3.8 ± 1.7 | 4.6 ± 3.2 | 0.041* |
| 20 Degrees Flexion | ||||
| BSO | 0.53 ± 0.07 | 0.51 ± 0.04 | 0.03 ± 0.28 | 0.12 |
| LPD | 01.1 ±2.1 | 03.5 ± 1.6 | 2.4 ± 2.1 | 0.028* |
| LPE | 2.9 ± 1.4 | 0.73 ± 0.84 | 2.2 ± 1.4 | 0.035* |
| PTA-S | 14.0 ± 4.72 | 11.7 ± 2.1 | 2.3 ± 3.1 | 0.15 |
| Sulcus | 133 ± 8.9 | 127 ± 2.8 | 5.0 ± 4.1 | 0.15 |
| Congruence | 08.1 ± 13.9 | 08.1 ± 13.0 | 0.008 ± 13.5 | 0.5 |
| TT-TG | 10.2 ± 3.0 | 4.0 ± 0.94 | 6.2 ± 2.0 | 0.006* |
| 10 Degrees Flexion | ||||
| BSO | 0.52 ± 0.05 | 0.51 ± 0.05 | 0.01 ± 0.07 | 0.39 |
| LPD | 01.7 ±1.5 | 03.2 ± 1.9 | 1.5 ± 2.5 | 0.17 |
| LPE | 3.0 ± 1.1 | 1.9 ± 0.18 | 1.8 ± 1.4 | 0.045* |
| PTA-S | 16.7 ± 8.2 | 12.9 ± 1.3 | 4.0 ± 8.3 | 0.17 |
| Sulcus | 136 ± 5.0 | 130 ± 4.4 | 6.2 ± 6.7 | 0.058 |
| Congruence | 011.4 ±12.9 | 012.3 ±4.9 | 0.93 ± 13.8 | 0.45 |
| TT-TG | 10.6 ± 1.7 | 4.0 ± 1.4 | 6.6 ± 2.2 | 0.0005* |
| 0 Degrees Flexion | ||||
| BSO | 0.53 ± 0.07 | 0.48 ± 0.08 | 0.06 ± 0.10 | 0.033* |
| LPD | 02.0 ± 3.8 | 05.1 ± 1.1 | 3.1 ± 1.2 | 0.011* |
| LPE | 3.9 ± 1.8 | 1.3 ± 1.8 | 2.5 ± 2.5 | 0.083 |
| PTA-S | 17.7 ± 4.7 | 16 ± 2.4 | 1.7 ± 5.2 | 0.22 |
| Sulcus | 138 ± 4.4 | 134 ± 5.7 | 4.0 ± 7.2 | 0.022* |
| Congruence | 013.5 ±14.7 | 014.4 ±8.7 | 0.89 ± 17.2 | 0.43 |
| TT-TG | 12.4 ± 2.9 | 3.7 ± 1.9 | 8.7 ± 3.4 | 0.003* |
Lateral patellar displacement (LPD) was reduced at all degrees of flexion following 15mm medial transfer, resulting in statistically significant reduction at 30, 20, and 0 degrees of flexion. The largest reduction in LPD occurred at 30 degrees of flexion when the value changed 3.66 ± 3.17mm (Table 1). The negative values associated with all of the LPD measurements, including the control measures, indicate that the most medial aspect of the patella was, on average, medial to the apex of the medial femoral condyle when using non-pathologic knee specimens.
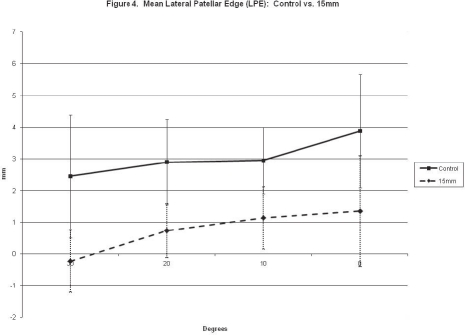
Similar to the LPD, lateral patellar edge (LPE) was reduced at all degrees of flexion following 15mm medial transfer. The reductions in LPE were statistically significant at 30,20, and 10 degrees of flexion. Although it was not statistically significant, the reduction in LPE following medial transfer at 0 degrees of flexion was 2.53 ± 2.51mm, a reduction that surpassed statistically significant changes in LPE at 20 and 10 degrees of flexion. However, this was subject to high variability (Table 1). The greatest reduction in LPE was seen at 30 degrees of flexion, as LPE decreased from 2.45 ± 1.94mm to -0.233 ± 0.988mm, the negative value indicating that the most lateral aspect of the patella was medial to the apex of the lateral femoral condyle (Table 1). In both the control and 15mm-transfer specimens, LPE gradually increased as the knee reached full extension, suggesting that the patella translates laterally in near-full extension (Figure 4).
Figure 4.
In both the control and 15mm-transfer specimens, LPE gradually increased as the knee reached full extension. Following 15mm medialization, LPE was decreased at all measured degrees of flexion.
The tibial tubercle-trochlear groove distance (TT-TG) was reduced a statistically significant amount at all evaluated degrees of flexion. Despite an intraoperative measurement of 15mm from the edge of the bony cut to the transferred tubercle, the largest measured change in TT-TG using axial MRI overlay (Figure 3) was 8.73 ± 3.41mm at 0 degrees of flexion (Table 1).
Following medial transfer, no statistically significant changes were detected at any evaluated degree of flexion for either the patellar tilt angle of Sasaki (PTA-S) or congruence angle. For both indices, 15mm transfer resulted in reduced or unchanged values when compared to the control at all investigated degrees of flexion (Table 1).
Although trochleoplasty was not performed in this study, the sulcus angle was reduced at all investigated degrees of flexion following 15mm transfer. The reduction was statistically significant at 0 degrees of flexion, resulting in a p-value of 0.02 as the sulcus angle changed 3.98 ± 7.15 degrees following 15mm transfer, as compared to the control (Table 1). The reduced sulcus angle values at all investigated degrees of flexion indicate that the surgical technique used to medialize the tibial tubercle in this study may have pulled the patella distally relative to the trochlear groove, placing the patella in a deeper portion of the trochlear groove when viewed in the axial plane.
DISCUSSION
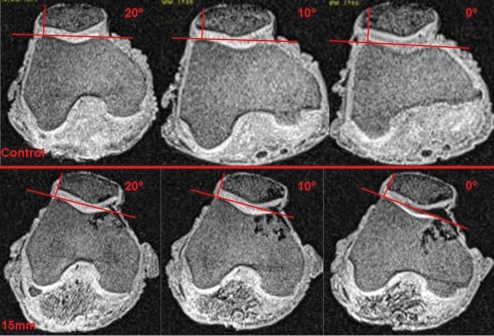
The results of this study indicate that medialization of the tibial tubercle as little as 15mm can significantly affect patellar tracking in non-pathologic cadaver specimens. However, the magnitude of these changes was not as great as expected. Significant changes in BSO, LPD, and LPE (Table 1) across the critical range of motion from 0-30 degrees where patellar instability is greatest, indicates that medialization had the greatest effect in reducing lateral patellar translation. When looking specifically at the LPE measurement, which has been reported as the best pre- and postoperative parameter to analyze patellar lateralization, a 15mm medial transfer produced a 2.53 ± 2.51mm medialization (Table 1).17 These changes yielded a 6:1 (15.0mm/2.53mm) intraoperative medialization-to-translation ratio with the knee in full extension and the quadriceps actively contracted. LPE appears to be of particular value as it correlates to the qualitative clinical J-sign defined previously (Figure 5). Because the presence or absence of the J-sign is used preoperatively to provide a dynamic evaluation of the patellofemoral joint during the physical examination, and postoperatively to evaluate the outcome of surgery, the quantification of this clinical finding has important surgical value.
Figure 5.
Images were collected using dynamic MRI during the final 20 degrees of knee flexion. When comparing me control and 15mm-transfer knees, it is clear that me amount of patella lateral to me perpendicular drawn from me apex of me lateral femoral condyle is reduced. Additionally, in both the control and 15mm knee, the amount of patella lateral to the perpendicular increases as the knee nears extension (0 degrees flexion).
Patellar tilt and congruence were not significantly altered following 15mm tibial tubercle transfer (Table 1). One reason for this may be that the medial and lateral retinacula were dissected in this experimental setup to create a more pathological situation by inducing lateral translation of the patella. 6 Because of this, the influence of the medial and lateral retinacula on patellar tilt and congruence was lost, eliminating the tethering effect that these structures have on the patella as the knee nears full extension. 5
When examining the TT-TG measurements in this study, the discrepancy between intraoperative bony measurements and postoperative radiographic measurements described in previous studies is apparent By using calipers to measure from the edge of the bony cut to the transferred bone block, the intraoperative tibial tubercle transfer distance was measured to be 15mm in every specimen. However, when making measurements on radiographs using the axial overlay technique as described by Dejour et al. (Figure 3), the mean change in TT-TG was only 8.73 ± 3.41mm with the leg in full extension (Table 1). This may be due to the external rotation of the tibia as the knee reaches full extension, altering the relationship between the tibial tubercle and trochlear groove when viewing axial radiographs. The inconsistencies in the intraoperative and postoperative TT-TG measurements have been investigated previously, and may be at least partially related to correctly and consistently locating the depth of the sulcus, accurately identifying the apex of the tibial tubercle, and the difficulty in making measurements on postoperative images with hardware artifact The findings in this study follow the trends seen in previous research, and continue to call into question the reliability of the TT-TG measurement.
The setup for this study evaluated patellofemoral kinematics in a non-weightbearing setting, as the force exerted by traction on the quadriceps tendon was equivalent to the weight of the components of the transected lower leg, including the tibia, fibula, and associated musculature. These loads were much lower than forces exerted across the knee during even low-impact activities such as walking. However, weightbearing has been shown to have a centering effect on the patella, significantly reducing lateral patellar displacement as the force generated by the quadriceps is increased.4,7 Because of this, the experimental setup used in this study examined the knee in a low-load setting where patellar instability is the greatest, and therefore it is not seen as a limitation.
However, several limitations of this study should be acknowledged. The small number of cadaver specimens (n=4) substantially limits statistical power. Still, when using only four specimens, statistically significant changes in patellar tracking were detected. Future studies should select a larger patient population exhibiting patellofemoral pathology requiring surgery. Retrospective analysis of pre- and postoperative MR images could be compared to the amount of tubercle transfer described in the surgical document to determine a relationship between intraoperative transfer distance and the effect on patellar tracking. Determining such a relationship would provide more objective guidance intraoperatively when medial-izing the tibial tubercle, reducing the dependence on clinical judgment currently required in medial transfer procedures.
Additionally, the non-pathologic knees used in this study do not have the same kinematics as pathological knees that the Southwick-Fulkerson osteotomy aims to correct in vivo. The cadaveric specimens in this study did not display any of the typical pathological anatomy commonly associated with severe cases of patellar instability including trochlear dysplasia, patella alta, malalignment of the extensor mechanism, TT-TG greater than 20mm, 11 patellar tilt greater than 20 degrees, and imbalance of soft-tissue restraints. 10,20 Previous research by Heegard et al. indicated that lateral translation of the patella could be increased by up to 10mm by dissecting the medial and lateral retinacula.6 While this step was taken in order to increase lateral patellar translation and simulate patellar instability, this simple dissection fails to fully mimic the complex bony and soft-tissue anatomy of a knee exhibiting severe patellar instability.
CONCLUSION
While the results of this study are limited by statistical power, it was found that quantitative evaluation of the patellofemoral joint following 15mm tibial tubercle medi-alization yielded signifcant changes in patellar tracking. These findings suggest that quantitative evaluation of patellofemoral kinematics may be a valuable pre- and postoperative tool when coupled with qualitative clinical findings. Although the results from this study were less than initially anticipated, they warrant future investigation using a larger sample size of pathologic knees in order to more accurately define the intraoperative me-dialization to translation ratio (TT-TG:LPE) proposed in this study. Accurately establishing such a measure could be of significant clinical value by reducing the amount of clinical judgment currently required to successfully perform tibial tubercle transfer procedures.
REFERENCES
- 1.Amis AA. Current Concepts on Anatomy and Bio-mechanics of Patellar Stability. Sports Medicine and Arthroscopy Review. 2007;15(2):48–56. doi: 10.1097/JSA.0b013e318053eb74. [DOI] [PubMed] [Google Scholar]
- 2.Feller JA, Amis AA, Andrish JT, Arendt EA, Erasmus PJ, Powers CM. Surgical Biomechanics of the Patellofemoral Joint. Arthroscopy. 2007;23(5):542–53. doi: 10.1016/j.arthro.2007.03.006. [DOI] [PubMed] [Google Scholar]
- 3.Brossmann J, Muhle C, Schroder C, Melchert UH, Bull CC, Spielmann RP, Heller M. Patellar Tracking Pattern during Active and Passive Knee Extension: Evaluation with Motion-Triggered Cine MR Imaging. Radiology. 1993;187(1):205–12. doi: 10.1148/radiology.187.1.8451415. [DOI] [PubMed] [Google Scholar]
- 4.Powers CM, Shellock FG, Pfaff M. Quantifcation of patellar tracking using kinematic MRI. Journal of Magnetic Resonance Imaging. 1998;8(3):724–732. doi: 10.1002/jmri.1880080332. [DOI] [PubMed] [Google Scholar]
- 5.Van Kampen A, Huiskes R. The three-dimensional tracking pattern of the human patella. Journal of Orthopaedic Research. 1990;8(3):372–82. doi: 10.1002/jor.1100080309. [DOI] [PubMed] [Google Scholar]
- 6.Heegaard J, Leyvraz PF, van Kampen A, Rakotomanana L, Rubin PJ, Blankevoort L. Infuence of Soft Structures on Patellar Three-Dimensional Tracking. Clinical Orthopaedics and Related Research. 1994;299:235–243. [PubMed] [Google Scholar]
- 7.Powers CM, Ward SR, Fredericson M, Guillet M, Shellock FG. Patellofemoral kinematics during weight-bearing and non-weight-bearing knee extension in persons with lateral subluxation of the patella: a preliminary study. The Journal of Orthopaedic and Sports Physical Therapy. 2003;33(11):677–85. doi: 10.2519/jospt.2003.33.11.677. [DOI] [PubMed] [Google Scholar]
- 8.Stanford W, Phelan J, Kathol MH, Rooholamini SA, El-Khoury GY, Palutsis GR, Albright JP. Patellofemoral joint motion: Evaluation by ultrafast computed tomography. Skeletal Radiology. 1988;17(7):487–92. doi: 10.1007/BF00364042. [DOI] [PubMed] [Google Scholar]
- 9.Brunet ME, Brinker MR, Cook SD, Christakis P, Fong B, Patron L, O'Connor DP. Patellar tracking during simulated quadriceps contraction. Clinical Orthopaedics and Related Research. 2003;414:266–75. doi: 10.1097/01.blo.0000079266.91782.11. [DOI] [PubMed] [Google Scholar]
- 10.Lavery M, Bell J, Rickelman T, Boezaart A, Albright J P. Patellofemoral realignment: dynamic intraoperative assessment. Iowa Orthopaedic Journal. 2005;25:160–163. [PMC free article] [PubMed] [Google Scholar]
- 11.Servien E, Verdonk PC, Neyret P. Tibial tuberosity transfer for episodic patellar dislocation. Sports Medicine and Arthroscopy Review. 2007;15(2):61–67. doi: 10.1097/JSA.0b013e3180479464. [DOI] [PubMed] [Google Scholar]
- 12.Albright J P, Wilson AG. Modified Fulkerson Osteotomy. Techniques in Knee Surgery. 2006;5(1):39–46. [Google Scholar]
- 13.Muhle C, Brossmann J, Heller M. Kinematic CT and MR imaging of the patellofemoral joint. European Radiology. 1999;9(3):508–18. doi: 10.1007/s003300050702. [DOI] [PubMed] [Google Scholar]
- 14.Dejour H, Walch G, Nove-Josserand L, Guier C. Factors of Patellar Instability: an anatomic radio-graphic study. Knee surgery, sports traumatology, arthroscopy: Offcial journal of ESSKA. 1994;2(1):19–26. doi: 10.1007/BF01552649. [DOI] [PubMed] [Google Scholar]
- 15.Lin YF, Jan MH, Lin DH, Cheng CK. Different effects of femoral and tibial rotation on the different measurement of patella tilting: An axial computed tomography study. Journal of Orthopaedic Surgery and Research. 2008;3(5) doi: 10.1186/1749-799X-3-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Laurin CA, Dussault R, Levesque HP. The tangential x-ray investigation of the patellofemoral joint: x-ray technique, diagnostic criteria and their interpretation. Clinical Orthopaedics. 1979;144:16–26. [PubMed] [Google Scholar]
- 17.Brossman J, Muhle C, Bull CC, Zieplies J. Cine MR imaging before and after realignment surgery for patellar maltracking – comparison with axial radiographs. Skeletal Radiology. 1995;24(3):191–96. doi: 10.1007/BF00228921. [DOI] [PubMed] [Google Scholar]
- 18.Sasaki T, Yagi T. Subluxation of the Patella – Investigation by computerized tomography. International Orthopaedics. 1986;10(2):115–20. [PubMed] [Google Scholar]
- 19.Merchant AC, Mercer RL, Jacobsen RH, Cool CR. Roentgenographic Analysis of Patellofemoral Congruence. Journal of Bone and Joint Surgery. 1974;56(7):1391–96. [PubMed] [Google Scholar]
- 20.Elias DA, White LM. Imaging of patellofemoral disorders. Clinical Radiology. 2004;59(7):543–57. doi: 10.1016/j.crad.2004.01.004. [DOI] [PubMed] [Google Scholar]