Abstract
Introduction
Injury to the saphenous nerve at the ankle has been described as a complication resulting from incision and dissection over the distal tibia and medial malleolus. However, the exact course and location of the distal saphenous nerve is not well described in the literature. The purpose of this study was to determine the distal limit of the saphenous nerve and its anatomic relationship to commonly identified orthopaedic landmarks and surgical incisions.
Methods
Sixteen cadaveric ankles were examined at the level of the distal tibia medial malleolus. An incision was made along the medial aspect of the lower extremity from the knee to the hallux to follow the course and branches of the saphenous nerve under direct visualization. We recorded the shortest distance from the most distal visualized portion of the saphenous nerve to the tip of the medial malleolus, to the antero-medial arthroscopic portal site, and to the tibialis anterior tendon.
Results
The saphenous nerve runs posterior to the greater saphenous vein in the leg and divides into an anterior and posterior branch approximately 3 cm proximal to the tip of the medial malleolus. These branches terminate in the integument proximal to the tip of the medial malleolus, while the vein continues into the foot. The anterior branch ends at the anterior aspect of the medial malleolus near the posterior edge of the greater saphenous vein. The posterior branch ends near the posterior aspect of the medial malleolus.
The average distance from the distal-most visualized aspect of the saphenous nerve to the tip of the medial malleolus measured 8mm +/−; 5mm; from the nerve to the medial arthroscopic portal measured 14mm +/−;2mm; and from the nerve to the tibialis anterior measured 16mm +/−;3mm. In only one case (of 16) was there an identifiable branch of the saphenous nerve extending to the foot and in this specimen it extended to the first metatarsophalangeal joint. The first metatarsophalangeal joint was innervated by the superficial peroneal nerve in all cases. Small variations were also noted.
Discussion and Conclusions
This study highlights the proximity of the distal saphenous nerve to common landmarks in orthopaedic surgery. This has important clinical implications in ankle arthroscopy, tarsal tunnel syndrome, fixation of distal tibia medial malleolar fractures, and other procedures centered about the medial malleolus. While the distal course of the saphenous nerve is generally predictable, variations exist and thus the orthopaedic surgeon must operate cautiously to prevent iatrogenic injury. To avoid saphenous nerve injury, incisions should stay distal to the tip of the medial malleolus. The medial arthroscopic portal should be more than one centimeter from the anterior aspect of the medial malleolus which will also avoid the greater saphenous vein. Incision over the anterior tibialis tendon should stay within one centimeter of the medial edge of the tendon.
INTRODUCTION
Saphenous nerve injury has long been recognized as a potential complication after a variety of orthopaedic procedures, including knee arthroscopy, leg fascioto-mies, and procedures about the ankle.1-9 Despite this fact, there are relatively few anatomic studies that evaluate the course of the saphenous nerve distally at the level of the ankle.9-11
Saphenous nerve injury during ankle arthroscopic portal placement has been described.8 This topic was investigated by Saito and Kikuchi in 77 ankles. 9 They found that the average distance from the saphenous nerve to the medial border of the ankle and the tibialis anterior tendon were 6mm and 11mm respectively. They concluded that the saphenous nerve is not at risk with arthroscopic antero-medial portal placement.
Ballmer et al.10 dissected 30 ankles evaluating the neurovascular network about the medial malleolus. Their results showed the use of a distally based saphenous neurocutaneous island flap to be viable because of the close relationship of the saphenous nerve and vein. They established that the larger anterior and smaller posterior saphenous nerves correlated with the saphenous vein in 100% and 90% of the specimens respectively at the ankle.
Williams and Sugars11 anatomically evaluated the course of the L4 nerve root, a root that contributes to the saphenous nerve and the anterior division of the femoral nerve. They concluded that the L4 nerve root terminates in most cases near the medial malleolus and proximal to the first metatarsophalangeal joint of the forefoot. They also found that the saphenous nerve entered the dermis at an average of 14.7 mm distal to the tip of the medial malleolus.
Anatomic reference books include the distal saphenous nerve, though there is a discrepancy between commonly used textbooks and the course of the saphenous nerve at the level of the ankle. In “Gray’s Anatomy,” it is written that the saphenous nerve “…descends behind the internal border of the tibia, and, at the lower third of the leg divides into two branches: one continues its course along the margin of the tibia, terminating at the inner ankle; the other passes in front of the ankle, and is distributed to the integument along the inner side of the foot, as far as the ball of the great toe, communicating with the [medial branch of the superficial peroneal nerve].”12 Hoppenfeld’s “Surgical Exposures in Orthopaedics,” fails to describe the exact course of the saphenous nerve distally. Instead, it is written that the saphenous nerve “…runs with the long saphenous vein in front of the medial malleolus, where it usually divides into two branches that lie on either side of the vein and bind closely to it”13 Hoppenfeld’s cautions that the nerve is often small and difficult to identify, and it is recommended in Hoppenfeld’s that in order to avoid a post-operative neuroma of the saphenous nerve, the nerve should be preserved by preserving the long saphenous vein.13 Hoppenfeld’s also includes a figure demonstrating the saphenous nerve continuing to the first metatarsophalangeal joint as a discrete structure, and it would appear, based on the drawing, that in a medial approach to the ankle or foot, one could identify and retract the saphenous nerve distal to the medial malleolus. Netter’s Atlas does not have a close-up depiction of the distal saphenous nerve, but in a sketch involving the entire nerve, a bifurcation is seen just above the medial malleolus with a large anterior branch continuing to the great toe, as in Hoppenfeld’s.13-14 Our experience is that this is not the case.
The purpose of our investigation was to determine the distal limit of the saphenous nerve and its anatomic relation to other structures, particularly common orthopedic landmarks.
METHODS
Eight cadavers with an age range of 69 to 95 years were used for this study providing a total of 16 ankles. A medial curvilinear incision was made from the knee to the hallux. Care was taken to avoid laceration of underlying structures. The saphenous vein was identified in the mid leg. The tip of the medial malleolus was used as a reference point for the location of the saphenous nerve. Branching of the nerve was identified and the location noted. The nerve branches were followed distally to the point of entry into the integument where they could no longer be dissected as distinct structures. The saphenous nerve, tip of the medial malleolus, antero-medial arthroscopic portal site, and tibialis anterior tendon were referenced and the shortest distance from the most distal visualized portion of the saphenous nerve to each structure was measured (Figures 1 and 2).
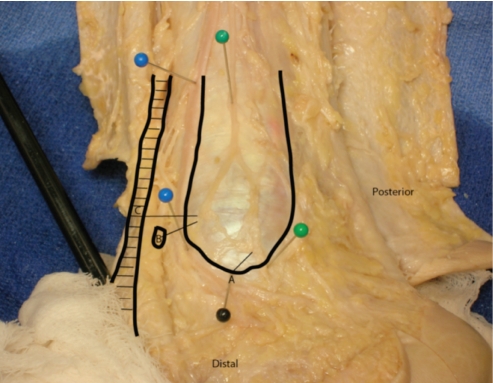
Figure 1.
Anatomic specimen of the saphenous nerve at the ankle. The saphenous nerve (proximal green pin) is identified posterior to the greater saphenous vein (blue pins). The saphenous nerve proximally (green pin) and the anterior and posterior (distal green pin) branches of the nerve are demonstrated.
The tip of the medial malleolus (A, and black pin), the anterior medial arthroscopic portal (B) and the medial edge of the tibialis anterior tendon (C) are identified as well as the shortest distance from each landmark to the nerve (dark solid lines). The Achilles tendon is seen posteriorly.
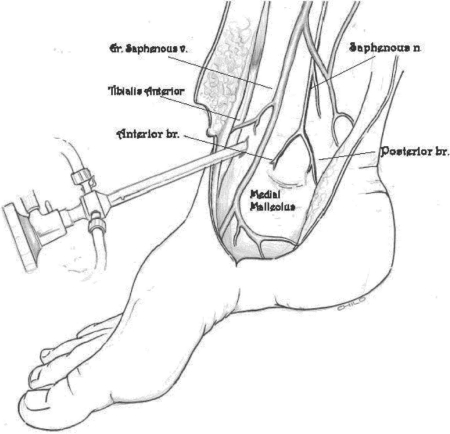
Figure 2.
Line drawing of the typical anatomy of the saphenous nerve as it runs posterior to the greater saphenous vein, divides into anterior and posterior branches and terminates in the skin proximal to the tip of the medial malleolus. The anterior branch terminates posterior to the greater saphenous vein and near the anterior border of the medial malleolus. The posterior branch terminates proximal to the posterior edge of the medial malleolus.
The saphenous nerve runs posterior to the greater saphenous vein in the leg and divides into an anterior and posterior branch 3 cm (+/−; 4 mm) proximal to the tip of the medial malleolus. These branches terminate in the dermis proximal to the tip of the medial malleolus, while the vein continues into the foot The anterior branch ends at the anterior aspect of the medial malleolus near the posterior edge of the greater saphenous vein. The posterior branch ends near the posterior aspect of the medial malleolus (Figures 1 and 2).
We found that the average distance of the most distal visualized aspect of the saphenous nerve to the tip of the medial malleolus was 8 mm (+/−; 5 mm). The average distance to the antero-medial arthroscopic portal site was 14mm (+/−; 2mm). The shortest distance to the tibialis anterior tendon was 16mm (+/−; 3mm).
In all specimens, the saphenous nerve divided into an anterior and posterior branch 3 cm +/−; 4 mm proximal to the tip of the medial malleolus; both branches were posterior to the greater saphenous vein. These two branches were grossly the same size and continued for approximately 2 centimeters before entering the integument. In 15 of the 16 specimens, these branches ended approximately 8mm proximal to the tip of the medial malleolus.
There was one variation in which the anterior branch of the saphenous nerve extended distally past the tip of the medial malleolus and ended at the first metatarsophalangeal joint The size of this anterior branch was larger than that in the other specimens. The posterior branch of this specimen had the same location, termination, and size as that in the other specimens.
DISCUSSION
Knowledge of anatomy is critical for the foundation of any surgeon. Surgeons-in-training often focus on common textbooks for an understanding of pertinent anatomy. We have observed that a discrepancy exists in the description of the course of the saphenous nerve at the medial malleolus in textbooks and current journal articles.
The most common depiction of the saphenous nerve is that there is a branch (usually the anterior branch) that extends to the first metatarsophalangeal joint and communicates at this level with branches of the superficial peroneal nerve.12-14 In our study, only one case of sixteen demonstrated an anterior branch of the saphenous nerve extending to the first metatarsophalangeal joint, similar to that depicted in major anatomic references. In Gray’s Anatomy, the saphenous nerve is described as communicating with the superficial peroneal nerve. This communication was not observed in any of our specimens. It appears that the most common depiction of the distal saphenous nerve is more aptly described as an uncommon variation. The most common pattern is for the nerve to divide into two branches approximately those branches to terminate in the integument proximal to the tip of the medial malleolus.
Our study highlights the proximity of the distal saphenous nerve to common landmarks in orthopaedic surgery about the ankle. The distances that we observed from the distal-most visualized portion of the saphenous nerve to common orthopaedic landmarks were similar to those found in recent studies. 9 Consistent with other anatomic studies, this has important clinical implications in orthopaedic surgical procedures centered around the medial malleolus.6-10 We have also observed distal saphenous nerve injury following the placement of distal interlocking screws for tibial intramedullary nails position of the distal locking hole puts the nerve at risk. Although we were not able to identify a safe zone in this study, the incision for distal locking screws in tibial nails should be placed as posteriorly as possible to minimize the risk of saphenous nerve injury. Saphenous nerve injury, most often noted as a painful neuroma, can contribute to significant procedure-related morbidity. Ideally, with a better understanding of anatomy, such potential complications could be avoided. To avoid saphenous nerve injury, incisions should stay distal to the medial malleolus. The medial arthroscopic portal should be more than one centimeter lateral to the anterior aspect of the medial malleolus and this location will also avoid the greater saphenous vein. Incision over the anterior tibialis tendon should stay within 1 cm of the medial edge of the tendon.
Table 1.
Average observed distances of die most distal branch of die saphenous nerve to common orthopaedic landmarks
| Distance | Interval | Average | SD |
|---|---|---|---|
| A | Nerve to Medical Malleous | 8mm | 5mm |
| B | Nerve to Antero-Medical Portal Site | 14mm | 2mm |
| C | Nerve to Tibialis Anterior | 16mm | 3mm |
Our study, as well as the studies by Ballmer et al.10 and Saito and Kikuchi9, differ from the more generalized saphenous nerve description in Hoppenfeld’s, Netter’s and Gray’s Anatomy. Furthermore, despite the fact that the distal saphenous nerve has a generally predictable course, individual variations are known to exist Thus, the orthopaedic surgeon must place incisions carefully to prevent iatrogenic injury.
REFERENCES
- 1.Luo H, Yu JK, Ao YF, Yu CL, Peng LB, Lin CY, Zhang JY, Fu X. Relationship between different skin incisions and the injury of the infrapatellar branch of the saphenous nerve during anterior cruciate ligament reconstruction. Chin Med J (Engl) 2007;120(13):1127–30. [PubMed] [Google Scholar]
- 2.Portland GH, Martin D, Keene G, Menz T. Injury to the infrapatellar branch of the saphenous nerve in anterior cruciate ligament reconstruction: comparison of horizontal versus vertical harvest site incisions. Arthroscopy. 2005;21(3):281–5. doi: 10.1016/j.arthro.2004.10.018. [DOI] [PubMed] [Google Scholar]
- 3.Kjaergaard J, Fauno LZ, Fauno P. Sensibility loss after ACL reconstruction with hamstring graft. IntJ Sports Med. 2008;29(6):507–ll. doi: 10.1055/s-2008-1038338. [DOI] [PubMed] [Google Scholar]
- 4.Mochida H, Kikuchi S. Injury to infrapatellar branch of saphenous nerve in arthroscopic knee surgery. Clin Orthop RelatRes. 1995;320:88–94. [PubMed] [Google Scholar]
- 5.Iizuka M, Yao R, Wainapel S. Saphenous nerve injury following medial knee joint injection: a case report. Arch Phys Med Rehabil. 2005;86(10):2062–5. doi: 10.1016/j.apmr.2005.05.002. [DOI] [PubMed] [Google Scholar]
- 6.Kim J, Dellon AL. Pain at the site of tarsal tunnel incision due to neuroma of the posterior branch of the saphenous nerve. J Am PodiatrMed Assoc. 2001;91(3):109–13. doi: 10.7547/87507315-91-3-109. [DOI] [PubMed] [Google Scholar]
- 7.Pyne D, Jawad AS, Padhiar N. Saphenous nerve injury after fasciotomy for compartment syndrome. Br J Sports Med. 2003;37(6):541–2. doi: 10.1136/bjsm.37.6.541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ferkel RD, Heatii DD, Guhl JF. Neurological complications of ankle arthroscopy. Arthroscopy. 1996;12(2):200–8. doi: 10.1016/s0749-8063(96)90011-0. [DOI] [PubMed] [Google Scholar]
- 9.Saito A, Kikuchi S. Anatomic relations between ankle arthroscopic portal sites and the superficial peroneal and saphenous nerves. Foot Ankle Int. 1998;19(11):748–52. doi: 10.1177/107110079801901107. [DOI] [PubMed] [Google Scholar]
- 10.Ballmer FT, Hertel R, Noetzli HP, Masquelet AC. The medial malleolar network: a constant vascular base of the distally based saphenous neurocutaneous island flap. Surg Radiol Anat. 1999;21(5):297–303. doi: 10.1007/BF01631327. [DOI] [PubMed] [Google Scholar]
- 11.Williams RP, Sugars W. Lumbar Root Innervation of the Medial Foot and Ankle Region. Aust NZJ Surg. 1998;68(8):565–7. doi: 10.1111/j.1445-2197.1998.tb02101.x. [DOI] [PubMed] [Google Scholar]
- 12.Pick TP, Howden R, editors. Gray’s Anatomy. 15th ed. Philadelphia: Lea Brothers & Co; 2003. p. 787. ISBN 1-587260654. [Google Scholar]
- 13.Hoppenfeld S, deBoer P. Surgical Exposures in Orthopaedics; The Anatomic Approach. 3rd ed. Philadelphia: Lippincott Williams & Wilkins; 2003. pp. 614–22. ISBN-13:978-0-7817-4228-3. 650-3. [Google Scholar]
- 14.Netter FH. Atlas of Human Anatomy. 3rd ed. Teterboro, NJ: ICON Learning Systems; 2003. p. 520. ISBN: 1-929007-11-6. [Google Scholar]