Abstract
Introduction
Very few cases of superior mesenteric vein thrombosis have been reported as a complication of appendicitis. In these handful of cases, the thrombosis was identified early with computerised tomography scan and patients have been managed conservatively with antibiotics and anticoagulation.
Presentation of case
A 45-year-old gentleman presented to the emergency department with a 13-day history of right lower quadrant abdominal pain and rigors. CT scan of the abdomen revealed an appendicular mass and superior mesenteric vein thrombosis. The patient was initially managed by anticoagulation and antibiotics for two weeks and was discharged after satisfactory clinical improvement. He represented after discharge for increased severity of his abdominal pain and abnormal inflammatory markers. Emergency open appendicectomy for complicated appendicitis was performed and his postoperative course was unremarkable. He was discharged on the 7th postoperative day with anticoagulation. Outpatient review at two months was unremarkable.
Discussion
Acute appendicitis is a common surgical presentation where history and examination is key in clinching the diagnosis. Inflammatory markers and imaging modalities such as a CT scan can be helpful. Although surgical intervention is the mainstay of treatment, conservative management with antibiotics is an option if the diagnosis of appendicitis is equivocal. Recent evidence has revealed that elective appendicectomy is not necessary upon successful conservative management. Acute appendicitis can lead to local perforations and abscesses. Complications such as thrombosis in the superior mesenteric vein are rare and can be managed successfully with anticoagulants.
Conclusion
Although this is a rare complication of appendicitis, the case was managed successfully with a conservative approach. This is inline with the general consensus which is to treat superior mesenteric vein thrombosis secondary to appendicitis conservatively unless the patient deteriorates.
Keywords: Superior mesenteric Vein Thrombosis, Appendicitis
1. Introduction
Acute appendicitis is the commonest surgical emergency. Common complications of appendicitis include abscess formation, perforation and peritonitis. These complications are relatively easy to recognize while rare complications such as mesenteric vein thrombosis are more difficult to recognize and manage.1,2 The aim of presenting this case is to discuss the management of this rare complication of appendicitis.
2. Case presentation
A 45-year-old gentleman presented to the emergency department with a 13-day history of severe right lower quadrant abdominal pain. It was initially a dull central lower abdominal pain that developed into a sharp intense pain associated with rigors. There was no history of nausea and vomiting. The patient was previously seen in Accident and Emergency (A&E) department nine days earlier and discharged home with a diagnosis of gastroenteritis as his examination and laboratory tests came back normal.
The patient is an accountant and had no significant past medical history. His alcohol intake was 100 units per week and smokes approximately 12 cigarettes a day.
On examination, his blood pressure was 138/70 mmHg with a pulse rate of 100/min. He had a temperature of 37.1 °C, with an oxygen saturation of 99% on air. The abdomen was soft but there was evidence of a smooth hepatosplenomegaly. Maximum tenderness was elicited in the right lower quadrant of the abdomen, particularly in the right iliac fossa. There was no rebound tenderness or guarding. Bowel sounds were sluggish and rectal examination was unremarkable.
Plain abdominal X-ray on admission showed some prominent loops of bowel (Fig. 1). A computerised tomography (CT) scan of the abdomen showed mildly enlarged liver and spleen, an appendicular mass, inflammation and stranding of the posterior peritoneum and an appendicolith. The scan also showed some fluid in the pelvis.
Fig. 1.

plain abdominal X-ray.
The other interesting finding was superior mesenteric vein obstruction due to thrombosis (Figs. 2 and 3).
Fig. 2.
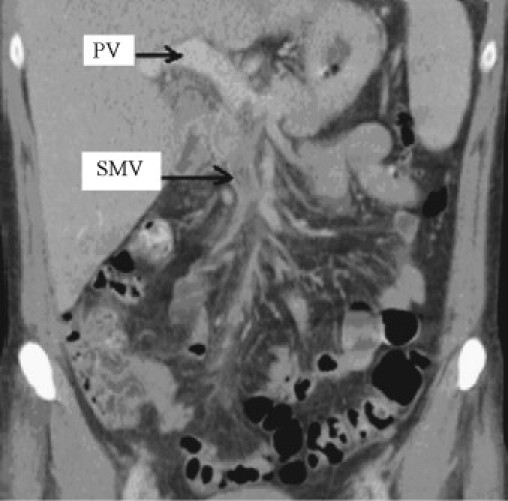
CT showed SMV thrombosis.
Fig. 3.
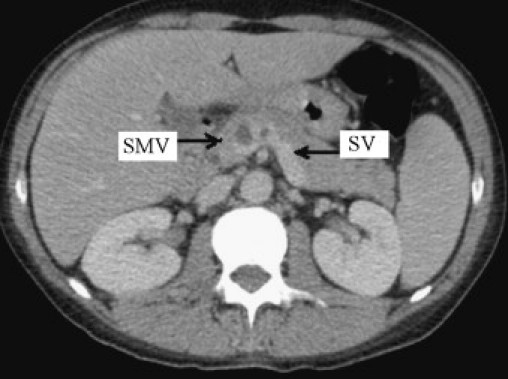
CT showed SMV thrombosis.
We decided to treat the appendicitis conservatively with antibiotics and superior mesenteric vein (SMV) thrombosis with therapeutic dose of enoxaparin after discussion with a haematologist. This was subsequently changed to warfarin. An ultrasound scan of the abdomen carried out a week post admission had ruled out abdominal abscess. After two weeks of antibiotic therapy, the patient showed improvement in clinical and biochemical signs and was discharged home.
He re-presented to the A&E three days after discharge with worsening abdominal pain. Examination revealed pyrexia, tenderness in the right iliac fossa and guarding. An urgent abdominal CT scan revealed an inflammatory mass in the right iliac fossa in keeping with appendicitis and signs showing minor resolution of the superior mesenteric vein thrombosis.
Due to the patient's deterioration, a clinical decision was made to proceed with an open appendicectomy. On exploration by a muscle cutting incision, the appendix was retrocaecal and was acutely inflamed. The appendix was long, extended to the liver and had formed a mass with marked inflammatory changes in the caecum and ascending colon. A very difficult retrograde appendicectomy was done and a drain was placed in situ.
The patient made a good recovery post operatively and was discharged home seven days after his operation pain free. The patient was recommenced on warfarin and asked to continue warfarin therapy for six months. After discussion with the radiologist, a CT scan of his abdomen has been arranged in five months time to assess the extent of the superior mesenteric vein thrombosis.
3. Discussion
Appendicitis is the most common cause of emergency surgery. The most frequent cause of appendicitis is thought to be due to faecal impaction causing obstruction and hence the infection. Although appendicitis can occur at any age, incidence is higher in teenagers and young adults and is slightly more common in males.1 Populations with low fibre intake are thought to be at higher risk of developing appendicitis.
The diagnosis of appendicitis very much relies on history and examination. If there is any doubt from clinical examination, the diagnosis can be helped with laboratory tests which might reveal leucocytosis and increased inflammatory markers.3,4 Ultrasound imaging and more increasingly, CT scan of the abdomen can also be done to reduce the incidence of negative laparotomies/laparoscopies.5
If the diagnosis of appendicitis is clear, and other differentials have been ruled out, the mainstay of management is surgical intervention.6 Laparoscopic appendicectomies are becoming more and more popular compared to open appendicectomies due to the advantages of minimal access technique.7 However, this is not possible in all cases and therefore open appendicectomies are still widely performed. If there are doubts about the diagnosis, the surgeon might opt for conservative treatment with antibiotics and monitor for clinical improvement. If this is the case, the patient is normally discharged after complete resolution of symptoms and patient can be followed up in clinic to decide if an elective appendicectomy at a later date is necessary.5 The decision to carryout interval appendicectomy has to be made based on individual patients as recent evidence has revealed that after successful conservative management, there is low recurrence rates8,9 and there are no advantages in proceeding with an interval appendicectomy in terms of wound infection and hospital stay.10
Common complications of appendicitis include perforation, peritonitis and abscess formation and complications associated with the surgical procedures.1 It has also been reported that severe appendicitis can result in portal vein thrombosis.2,11,12
However, there have only been a handful of cases where thrombosis of the superior mesenteric vein occurs as a result of inflammation of the appendix.13–15 It is difficult to predict the diagnosis on the clinical ground. The pathogenesis of this complication is thought to be due to thrombophlebitis resulting in thrombosis.7 In these aforementioned cases, the initial imaging of choice was CT scan of the abdomen and the management of choice was conservative treatment with intravenous antibiotics and heparin therapy. Appendicectomy was then arranged at a later date as an elective procedure. Acute venous thrombosis carries a mortality rate of 30% and a recurrence rate of 25% if not treated with anticoagulant therapy. This rate of recurrence can be reduced to as low as 11% if anticoagulant therapy is combined with surgical treatment.16 There is a huge variability in the literature with regards to follow up in patients with mesenteric thrombosis. Patients can show almost complete resolution of their thrombosis as early as the first month of treatment with anticoagulation.17
There have been many cases of portal vein thrombosis following a superior mesenteric vein thrombosis. The pathogenesis of this is thought to be due to reduced flow and ascending infection in the portal system causing portal empyema. This occlusion in the portal system can result in portal hypertension.18
4. Conclusion
Acute appendicitis is a very common surgical problem with rare but possibly severe complications. This case clearly illustrates the importance of early diagnosis and treatment of acute appendicitis and it's rare complication.
Conflict of interest
None.
Funding
None.
Ethical approval
Written consent was obtained from the patient for publication of this case report and accompanying images. This consent is available for review by the Editor-in-Chief of the journal on request.
Contributors
Nik Bakti, information collection and write up; Abdul Hussain, review; and Shamsi El-Hasani, supervisor.
References
- 1.Humes D.J., Simpson J. Acute appendicitis. BMJ. 2006;333(7567):530–534. doi: 10.1136/bmj.38940.664363.AE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Marova K., Chochola M., Golan L., Krivanek J., Aschermann M. Liver abscesses with portal and mesenteric vein thrombosis in combination with late onset of appendicitis. Cas Lek Cesk. 2005;139(3):135–136. [PubMed] [Google Scholar]
- 3.de Carvalho B.R., Diogo-Filho A., Fernandes C., Barra C.B. Leucokyte count C reactive protein, alpha-1 acid glycoprotein and erythrocyte sedimentation rate in acute appendicitis. Gastroenterology. 2003;40(1):25–30. doi: 10.1590/s0004-28032003000100006. [DOI] [PubMed] [Google Scholar]
- 4.Asfar S., Safar H., Khoursheed M., Dashti H., al-Bader A. Would measurement of C-reactive protein reduce the rate of negative exploration of acute appendicitis. J R Coll Surg Edinb. 2000;45(1):21–24. [PubMed] [Google Scholar]
- 5.Harswick C., Uyenishi A.A., Kordick M.F., Chan S.B. Clinical guidelines, computed tomography scan and negative appendicectomies: a case series. Am J Emerg Med. 2006;24(1):68–72. doi: 10.1016/j.ajem.2005.07.015. [DOI] [PubMed] [Google Scholar]
- 6.Benjamin I.S., Patel A.G. Managing acute appendicitis. BMJ. 2002;325(7363):505–506. doi: 10.1136/bmj.325.7363.505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sauerland S., Lefering R., Neugebauer E.A. Laparoscopic versus open surgery for suspected appendicitis. Cochrane Database Syst Rev. 2004;18(4):CD001546. doi: 10.1002/14651858.CD001546.pub2. [DOI] [PubMed] [Google Scholar]
- 8.Anderson R.E., Petzold M.G. Nonsurgical treatment of appendiceal abscess or phlegmon: a sustemic review and meta-analysis. Ann Surg. 2007;246(5):741–748. doi: 10.1097/SLA.0b013e31811f3f9f. [DOI] [PubMed] [Google Scholar]
- 9.Hall N.J., Jones C.E., Eaton S., Stanton M.P., Burge D.M. Is interval appendicectomy justified after successful nonoperative treatment of an appendix mass in children? A systemic review. J Pediatr Surg. 2011;46(4):767–771. doi: 10.1016/j.jpedsurg.2011.01.019. [DOI] [PubMed] [Google Scholar]
- 10.St Peter S.D., Aguayo P., Fraser J.D., Keckler S.J., Sharp S.W., Leys C.M. Initial laparoscopic appendectomy versus initial nonoperative management and interval appendectomy for perforated appendicitis with abscess: a prospective, randomized trial. J Pediatr Surg. 2010;45(1):236–240. doi: 10.1016/j.jpedsurg.2009.10.039. [DOI] [PubMed] [Google Scholar]
- 11.Ayantunde A.A., Debrah S.A. Portal vein thrombosis complicating appendicitis. West Afr J Med. 2004;23(4):332–334. doi: 10.4314/wajm.v23i4.28151. [DOI] [PubMed] [Google Scholar]
- 12.von Bertele M.J. Late presentation of portal vein thrombosis as a complication of appendicitis. J R Army Med Corps. 1993;144(7):135–136. doi: 10.1136/jramc-139-03-16. [DOI] [PubMed] [Google Scholar]
- 13.Germain M.A., Soukhni N., Bourzard D. Mesenteric venous thrombosis complicating acute appendicitis. Ann Chir. 2002;127(5):381–384. doi: 10.1016/s0003-3944(02)00776-9. [DOI] [PubMed] [Google Scholar]
- 14.van Spronsen F.J., de Lange Z.J., van Elburg R.M., Kimpen J.L. Appendicitis in an eleven-year-old boy complicated by thrombosis of the portal and superior mesenteric veins. Pediatr Infect Dis J. 1996;15(10):910–912. doi: 10.1097/00006454-199610000-00017. [DOI] [PubMed] [Google Scholar]
- 15.Echtibi S.S., Bashir M.O., Ahmed M.U., Branicki F.J., Abu-Zidan F.M. Superior mesenteric vein thombosis complicating appendicular masses. Saudi Med J. 2003;24(9):1016–1018. [PubMed] [Google Scholar]
- 16.Divino C.M., Park I.S., Angel L.P., Ellozy S., Spiegel R., Kim U. A retrospective study of diagnosis and management of mesenteric vein thrombosis. Am J Surg. 2001;181(1):20–23. doi: 10.1016/s0002-9610(00)00532-8. [DOI] [PubMed] [Google Scholar]
- 17.Kemppainen E., Kokkola A., Siren J., Kiviluoto T. Superior mesenteric and portal vein thrombosis following laparoscopic nissen fundoplication. Dig Surg. 2000;12(3):279–281. doi: 10.1159/000018848. [DOI] [PubMed] [Google Scholar]
- 18.Aldrete J.S., Slaughter R.L., Han S.Y. Portal vein thrombosis resulting in portal hypertension in adults. Am J Gastroenterol. 1976;65(3):236–246. [PubMed] [Google Scholar]


